Overview:
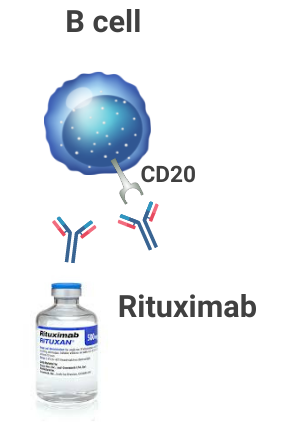
- Rituximab is a humanized monoclonal antibody that targets CD20 antigen present on B lymphocytes, leading to depletion of B lymphocytes.
- Rituximab has been used in the treatment of a wide variety of autoimmune diseases, including immune thrombocytopenia and autoimmune hemolytic anemia.
- The rationale for considering treatment with rituximab is that > 95% of adult patients with immune thrombotic thrombocytopenic purpura (iTTP) are reported to have autoantibodies against ADAMTS13.
- Prospective studies have shown that rituximab is effective and safe in iTTP. There is no evidence of increased infection risk.
- Rituximab was first used to treat iTTP in relapsed or refractory cases, where it was found to be effective in attaining remission and reducing relapse rates.
- Rituximab was subsequently used:
- In acute de novo iTTP cases, leading to reduced relapse rates and an increase in time to relapse.
- On a prophylactic basis to patients deemed to be at high risk of an acute TTP relapse.
Suggested dosing:
- 375 mg/m2 IV weekly for 4 weeks.
- Therapeutic plasma exchange (TPE) should be discontinued for ≥ 4 hours after rituximab infusion, to minimize removal of rituximab during exchange.
- Giving rituximab more frequently than weekly, e.g. every 3–4 days, may overcome removal during TPE.
Notes:
- Rule out hepatitis B infection before giving rituximab, which may delay use in emergency settings.
First-line therapy:
- Scully et al, 2011
- Phase 2, nonrandomized trial.
- Forty patients with acquired (immune) TTP (34 de novo, 6 relapse) received rituximab 375 mg/m2 intravenously within the first 3 days of admission and diagnosis. A total of 4 treatments, 1 per week for 4 weeks, were given.
- Clinical outcomes were compared to historical controls (n = 40) who had not received rituximab.
- All patients received corticosteroids and TPE continued daily from admission and until a sustained platelet count of > 150 x 109/L was reached for 2 consecutive days.
- As compared with historical controls, patients receiving rituximab showed:
- No overall difference in length of stay
- Fewer TPE episodes (in whites compared to nonwhites in the rituximab group)
- Significant reduction in relapse risk
- Decrease in anti-ADAMTS13 IgG and a rise in ADAMTS13 activity
- No excess infections or serious adverse events with rituximab
- Westwood et al, 2013
- Rituximab given in 104 episodes of acute TTP, 86 patients who had never been previously treated with rituximab (rituximab-naïve patients).
- Of the rituximab-naïve patients, rituximab was given within 3 days of admission in 54, and after 3 days in 32.
- In rituximab-naïve patients:
- Administration of rituximab early (< or equal to 3 days) rather than late (> 3 days) was associated with:
- A significant reduction in the number of TPE.
- Faster attainment of remission
- Shorter hospital stay
- Complete remission was achieved in 82/86 (95%) patients. All four patients who did not achieve remission died during the acute episode.
- The overall time to remission was 14 days (range 4–52 days).
- Administration of rituximab early (< or equal to 3 days) rather than late (> 3 days) was associated with:
Second-line therapy:
- Scully et al, 2007
- Twenty-five patients with acute refractory/relapsing idiopathic TTP received rituximab in conjunction with PEX because of progressive clinical disease or deterioration in laboratory parameters, despite intensive standard therapy.
- All patients received daily i.v. methylprednisolone for 3 d and daily PEX until the platelet count was >150 · 10 9 /l for longer than 48 hours.
- PEX was continued on an alternate day regime until a continued rise in platelets was maintained.
- Patients received i.v. infusion of 375 mg/m 2 rituximab each week for 4 weeks, immediately following PEX.
- All 25 patients attained complete clinical and laboratory remission in a median of 11 d after initiating rituximab.
- In 21 cases, ADAMTS-13 activity was within the normal range following rituximab.
- Inhibitors were detected in 24/25 patients by mixing studies and/or immunoglobulin G (IgG) antibodies to ADAMTS-13 pre-rituximab.
- There was no evidence of inhibitors and/or IgG activity <10% in 23/25 patients following rituximab.
- In acute refractory cases, the median number of PEX pre-rituximab and following the first rituximab infusion was 13 and 9, respectively.
- No infectious complications
- Conclusion: In patients with acute refractory/relapsing idiopathic TTP, rituximab appears to be a safe, effective, targeted therapy with a significant reduction in the requirement for PEX.
- Benhamou et al, 2016
- 24 patients with a flare-up episode of iTTP were enrolled in this prospective multicenter single arm phase II study and then compared to patients from a previous study.
- Goal was to assess the efficacy of a rituximab regimen based on B cell depletion.
- Patients with a suboptimal response to a plasma exchange-based regimen received two infusions of rituximab 375 mg/m2 within 4 days, and a third dose at day +15 of the first infusion if peripheral B cells were still detectable.
- Results were compared to patients from a previous study who had received standard four-rituximab infusion.
- TPE was carried out daily immediately after TTP diagnosis.1
- Patients without active infection received steroids.
- Primary endpoint was the assessment of the time required to platelet count recovery from the first plasma exchange.
- Time to platelet count recovery was comparable between groups.
- Three patients died after the first rituximab administration. In the remaining patients, the B cell-driven treatment hastened remission and ADAMTS13 activity recovery as a result of rapid anti-ADAMTS13 depletion in a similar manner to the standard four-rituximab infusions schedule.
- The 1-year relapse-free survival was also comparable between both groups.
- Conclusion: A rituximab regimen based on B cell depletion is feasible and provides comparable results than with the four-rituximab infusions schedule. This regimen could represent a new standard in TTP.
Guideline recommendations:
- ISTH guidelines:
- For patients with iTTP experiencing their first acute event, the panel suggests the addition of rituximab to corticosteroids and TPE over corticosteroids and TPE alone. (A conditional recommendation in the context of very low certainty evidence.)
- The panel notes that the primary effect of rituximab appears to be the prevention of relapses; however, many patients with iTTP may not experience a relapse, regardless of the initial treatment regimen. Given such low certainty evidence, a fairly narrowed range of outcomes affected by rituximab, and issues related to drug cost, the panel choose to make conditional recommendation for the use of rituximab.
- Practitioners may consider among the conditions in favor of rituximab use, the presence of a known comorbid autoimmune disorder, albeit with scant supportive evidence.
- For patients with iTTP experiencing a relapse, the panel suggests the addition of rituximab to corticosteroids and TPE over corticosteroids and TPE alone. (A conditional recommendation in the context of very low certainty evidence.)
- For patients with iTTP who are in remission but still have low plasma ADAMTS13 activity with no clinical signs/symptoms, the panel suggests the use of rituximab over nonuse of rituximab for prophylaxis.
- British Committee for Standards in Haematology:
- In acute idiopathic TTP with neurological/cardiac pathology, which are associated with a high mortality, rituximab should be considered on admission, in conjunction with PEX and steroids (Grade 1B).
- Patients with refractory or relapsing immune-mediated TTP should be offered rituximab (Grade 1B).
- Guidelines on the Use of Therapeutic Apheresis in Clinical Practice:
- Rituximab is commonly used to treat refractory or relapsing TTP.
- Studies have also described the incorporation of rituximab as adjunctive agent with initial TPE.
- Since rituximab immediately binds to CD20-bearing lymphocytes, an 18-24-hour interval between its infusion and TPE is used in practice.
Want to explore this further?
Check out the related sections in our TTP module:
- Journal Club on Scully et al. A phase 2 study of the safety and efficacy of rituximab with plasma exchange in acute acquired thrombotic thrombocytopenic purpura. Blood. 2011 Aug 18;118(7):1746-53
- Treatment of TTP – Overview
- Video Lecture on TTP Treatment
- Section on Refractory TTP
