I posted a poll on Twitter asking whether you would treat a newly diagnosed patient with immune thrombocytopenia (ITP) with prednisone 1 mg/kg/day or with high dose dexamethasone (HD-DXM) 40 mg/day x 4 days.
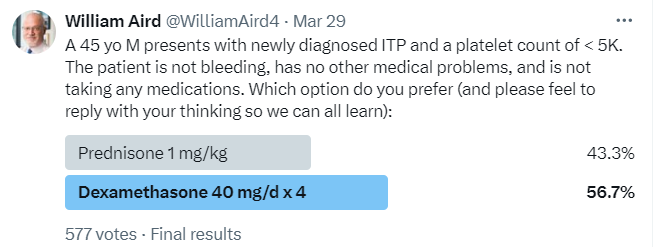
Most respondents (56.7%) chose HD-DXM.
There is no right answer!
Bottom line
According to clinical practice guidelines, prednisone and HD-DXM are both acceptable first-line agents for treating ITP. A systematic review and meta-analysis showed:
- Higher initial response (2 weeks) with HD-DXM
- No difference in response at 6 months.1
- Fewer reported toxicities with HD-DXM
The American Society of Hematology 2019 guideline for ITP states: “If a high value is placed on rapidity of platelet count response, an initial course of dexamethasone may be preferred over prednisone”.2
Fewer days of treatment, better initial response, less bleeding, few sider effects – what’s not to prefer about a single cycle of HD-DXM over prednisone?
| Parameter | Prednisone | HD-DXM |
|---|---|---|
| Total prednisone equivalent dose | 2100 mg3 | 1,000 mg4 |
| Need for (often cumbersome) taper | Yes5 | No |
| Potential for compliance issues | More6 | Less |
| Initial response | Slower and less CRs | Faster and more CRs |
| Sustained response | No difference | No difference |
| Adverse effects | More (including bleeding) | Less |
Overview
- Primary immune thrombocytopenia (ITP) is an autoimmune disorder characterized by isolated thrombocytopenia in the absence of underlying causes.
- ITP has an incidence of 2 to 4 cases per 100 000 person-years with 2 peaks:
- Age between 20 and 30 years; slight prevalence for female sex.
- Age >60 years; same prevalence for males and females.
- Pathogenesis of ITP involves autoantibody-mediated destruction of platelets.
- Patients present with incidental finding of thrombocytopenia or with bleeding.
- First line therapy is with corticosteroids, either prednisone or high dose dexamethasone. Although 60 to 80% of patients with ITP have an initial response to glucocorticoids, only 30 to 50% of adults have a sustained response after glucocorticoids are discontinued.
Corticosteroids
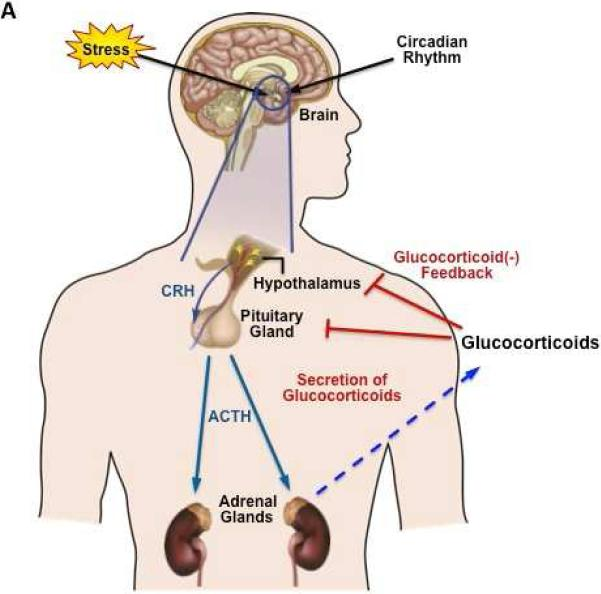
- Corticosteroids are a class of steroid hormones released by the adrenal cortex, which includes glucocorticoids and mineralocorticoids. However, the term “corticosteroids” is generally used to refer to glucocorticoids.
- Glucocorticoids may be:
- Natural, for example:
- Cortisone
- Cortisol
- Synthetic
- Natural, for example:
- Natural glucocorticoids are steroid hormones synthesized and released by the adrenal glands in a circadian manner, in response to physiological cues and stress.
- Synthetic glucocorticoids are:
- Widely available
- One of the most widely prescribed drugs in the world
- Quick acting
- Often well tolerated when used for short periods at low doses
- Therapeutic benefits of glucocorticoids are limited by the adverse side effects that are associated with high dose and long-term use. These side effects include:
- Osteoporosis
- Skin atrophy
- Diabetes
- Abdominal obesity
- Glaucoma
- Cataracts
- Avascular necrosis
- Infection
- Hypertension
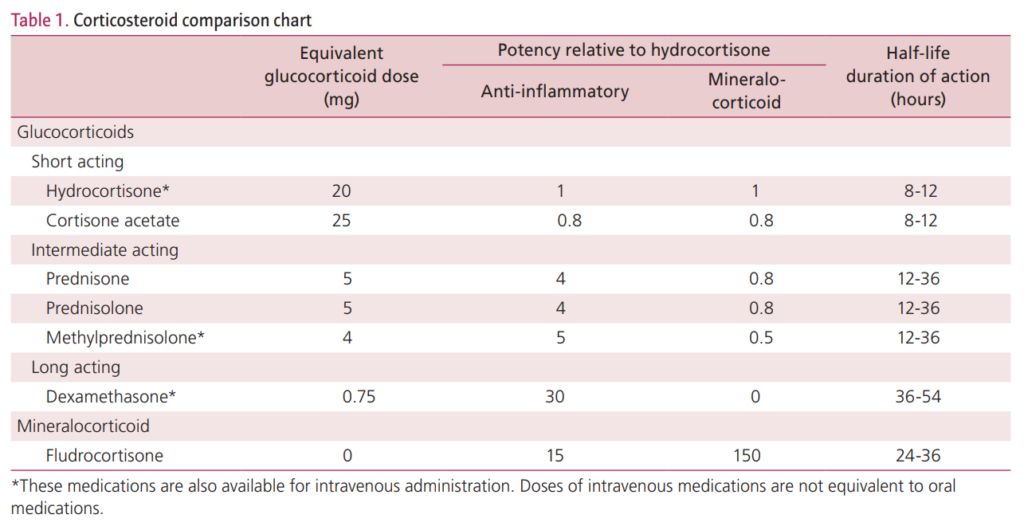
- Different preparations of oral glucocorticoids:
- Have same rate of absorption and are roughly bioequivalent.
- Differ in their potency and kinetics or have slight variations in their mechanisms of action.
- Typical corticosteroid regimens in ITP:
- Prednisone or prednisolone at a starting dose of 0.5 to 2 mg/kg per day for 2 to 4 weeks.
- Pulsed high-dose dexamethasone, administered every 28 days for a 4-day course, 1-6 cycles.
- Dexamethasone is a corticosteroid that has an anti-inflammatory effect that is more than six times more potent than prednisone (40 mg of dexamethasone is equivalent to 250 mg of prednisone) with a longer biological half-life (36–72 h compared with 12–36 h).78
- Any difference in efficacy or toxicity between the two approaches probably reflects differences in dosage rather than intrinsic properties of the drugs.9
History
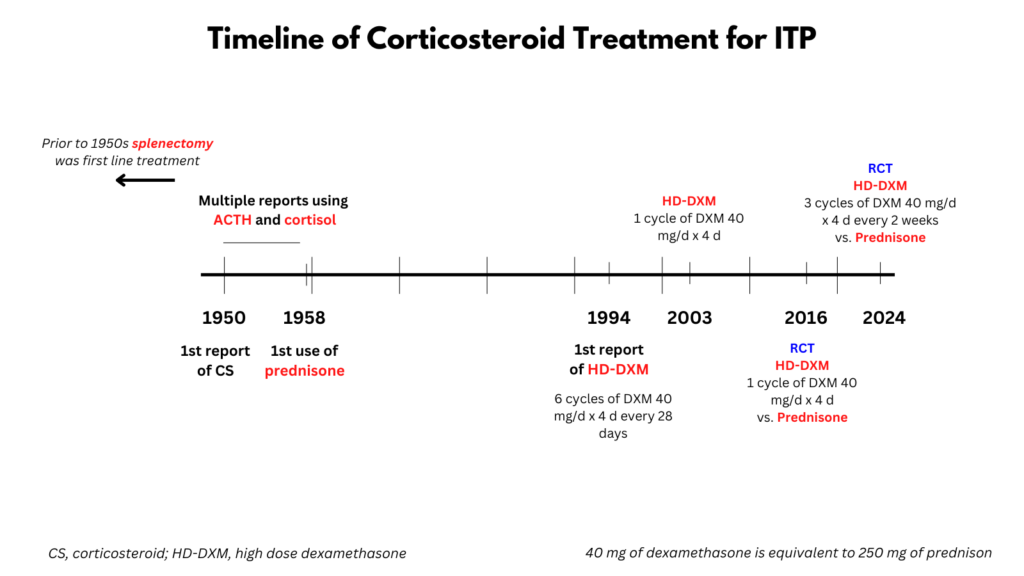
- In 1950, Robson and Duthie studied the effect of cortisone in two cases of ITP; one patient achieved remission.10
- In 1950, Meyer and co-workers treated five patients with 100 mg of corticotropin11 per day and concluded that the drug had value in the treatment of ITP.13
- In 1951, Faloon and co-workers treated 3 patients with ITP with corticotropin and one with cortisone, noting improvement of bleeding manifestations and of the capillary fragility.14
- In 1952, Stefanini and colleagues reported on 3 patients with ITP treated with corticotropin and/or cortisone with mixed results.15
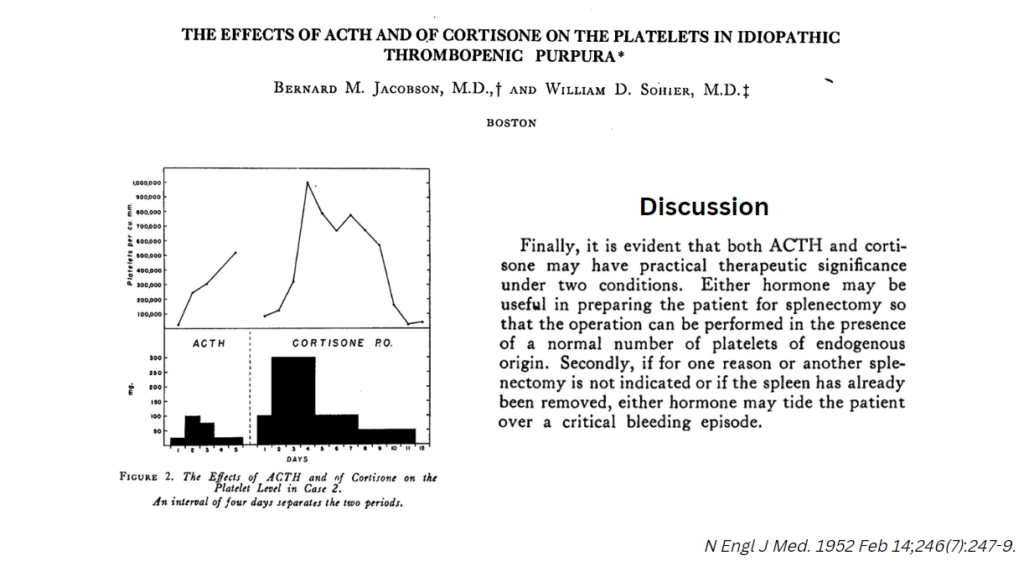
- In 1952, Jacobson and Sohier reported prompt increase in platelet counts in 3 patients with ITP treated with ACTH and/or cortisone.
- In 1952, Wilson and Eisemann described complete clinical and hematologic remission in 5 of 12 patients with ITP following the therapeutic administration of ACTH or cortisone.
- In 1954, Pariser and Wasserman reported on 16 cases of ITP treated with ACTH and cortisone with better effects in acute vs. chronic ITP.
- In 1958, Dameshek et al published a study on the use of prednisone in ITP:
- In the Introduction, the authors wrote (all worth quoting for context):
- “In recent years, the danger of fatal, usually cerebral, bleeding in the course of ITP has been considerably reduced by the introduction of two “medical” methods, i.e., the use of siliconized bottles or plastic bags for transfusion of fresh whole blood, including viable platelets, and the use of ACTH and the corticosteroid hormones. It has been adequately demonstrated that with these two measures even the acute cases of ITP, with severe bleeding into the skin and mucous membranes, can be kept under good control and tided over the hemorrhagic crisis, usually a matter of a few to several days.”
- “The effects of ACTH and later of cortisone on the bleeding disorder appeared to be mediated largely through the small blood vessels. Thus, striking improvement in the bleeding tendency usually took place even without a rise in platelets.”
- “Our own studies indicated that, although ACTH and cortisone were of distinct value in diminishing bleeding, they were of uncertain value in initiating a rise in platelets. Thus, the use of these agents in ITP during a period of approximately five years led us to conclude that splenectomy was still the specific method of therapy in those cases continuing at low platelet levels for more than four to six months and that steroid therapy was chiefly valuable as a nonspecific “antihemorrhagic” agent.”
- “In the past few years, as it became increasingly apparent that the initial remissions after splenectomy were followed by increasing numbers of relapses, a reevaluation of the effects of the steroids in ITP, with particular reference to the blood platelet count, seemed desirable, especially when the new steroid, prednisone (Meticorten), became available. Since it was possible to use this material in large, even massive doses and with minimal water retention, a series of consecutive cases of ITP was treated. It was soon evident that striking rises in platelet level took place with great consistency, whether the patient’s condition was acute or chronic or had relapsed after splenectomy.”
- 30 consecutive cases of ITP treated with prednisone:
- The initial dose of prednisone varied from case to case; doses of 20 to 250 mg per day were used.
- 22 (73%) achieved complete remission:
- 10/11 (90%) acute cases
- 12/19 (60%) chronic cases
- Average time to response (“well-defined rise in platelets”) 9 days in acute cases, 16 days in chronic cases
- Relapse common after discontinuation of prednisone
- In the Discussion, the authors wrote:
- “The consistent effect of prednisone in raising the platelet level in these cases of ITP has been a striking phenomenon; its mechanism is by no means obvious:
- A direct (inhibitory?) effect on the spleen can be ruled out because the steroid was effective even in the absence of the spleen.
- Was the effect due to a:
- Stimulatory one on the megakaryocytic production of platelets
- Reduction in thrombocytopenic factor, which is presumably of immunological nature?
- This is by no means clear and requires further study, but in view of the demonstration by several groups of workers of an immunological mechanism in ITPs and the well-known effects of the corticosteroids in inducing a reduction in antibody concentration, not only with the infectious antibodies but with the antibodies of “autoimmune” hemolytic anemia, it seems more likely to us that prednisone acts through depression of antibody production. We have commented previously on the many similarities between autoimmune hemolytic anemia and ITP.”
- “The consistent effect of prednisone in raising the platelet level in these cases of ITP has been a striking phenomenon; its mechanism is by no means obvious:
- In the Introduction, the authors wrote (all worth quoting for context):
- In 1958, Williams et al reported on the treatment of of acute and chronic ITP:
- 19 patients were treated with corticotrophin (ACTH), cortisone, or prednisolone less than a hundred days from the onset of symptoms:
- 11 cases the duration of treatment was ten days or less:
- Complete remission in 5 patients, which persisted after treatment was stopped.
- One patient had improvement in platelet count, but relapsed after discontinuation of corticosteroid.
- No response in 5 patients.
- 8 cases received more than 10 days of treatment:
- Complete remission in 4.
- No response in 4.
- 11 cases the duration of treatment was ten days or less:
- 23 patients were treated with corticotrophin (ACTH), cortisone, or prednisolone more than a hundred days from the onset of symptoms (20 of whom also had splenectomy):
- 8/17 patients treated with steroids before splenectomy achieved remission.
- 5/9 patients treated with steroids after splenectomy achieved remission.
- In the Discussion, the authors wrote:
- “The results of steroid therapy in our short-history cases suggest that these drugs do no more than facilitate the natural tendency of this disease to spontaneous remission and possibly accelerate its onset.”
- “Our results suggest that the initial management of the patient with a short history of purpura should be blood transfusion to replace any serious blood-loss and administration of cortisone (75 mg. every six hours) or prednisolone (15 mg. every six hours) for three weeks. If the platelet-count rises during this time, there is a very good chance that it will be maintained. If there is no improvement within three weeks, splenectomy should be performed in the expectation that at this time it will be followed by a good result in 75% of cases. We can adduce no evidence to show that the patient in the acute hemorrhagic phase is benefited by splenectomy.”
- 19 patients were treated with corticotrophin (ACTH), cortisone, or prednisolone less than a hundred days from the onset of symptoms:
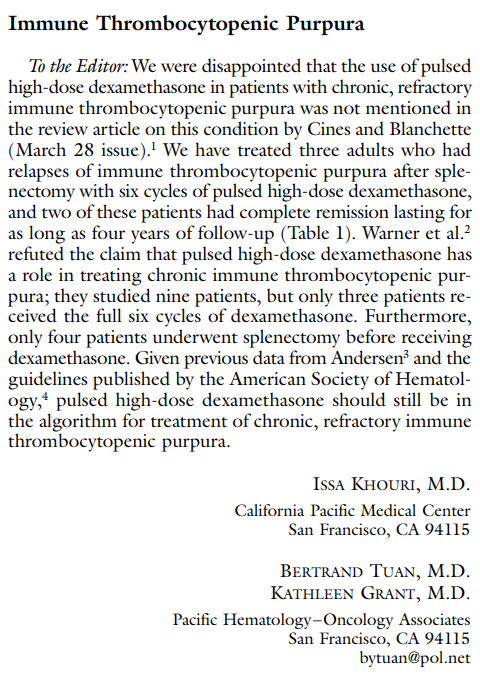
- In 1994, Andersen was the first to report on the use of high-dose dexamethasone in ITP
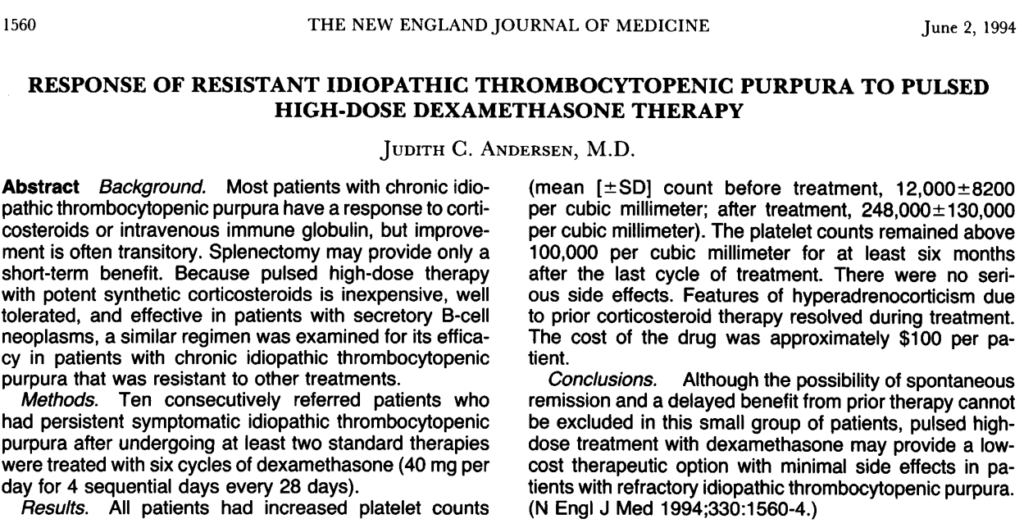
- A comment that refers to the Andersen paper:
Selected Studies16
- 2003 study on initial treatment of ITP with HD-DXM:
- 125 patients with ITP received 40 mg of oral dexamethasone daily for four consecutive days (single cycle).
- 106/125 patients (85%) had an initial response to high-dose dexamethasone:
- Platelet count had increased by at least 20,000 per cubic millimeter by the third day of treatment.
- The mean platelet count was 101,400±53,200 per cubic millimeter (range, 50,000 to 260,000 per cubic millimeter) one week after the initiation of treatment in this group of 106 patients.
- Follow-up:
- Median follow-up period was 30.5 months (range, 13.0 to 59.5 months).
- No patients were lost to follow-up.
- Among the 106 patients with a response to dexamethasone therapy, 53 (50%) had a sustained platelet count of more than 50,000 per cubic millimeter after a single course of high dose dexamethasone therapy and required no further treatment during two to five years of follow-up.
- All patients with a relapse had a response to a second course of high-dose dexamethasone therapy.
- Authors’ conclusions: “In summary, a four-day course of high-dose oral dexamethasone is an effective initial treatment for immune thrombocytopenic purpura in adults. Long-term remission is obtained in more than 40 percent of patients after a single course of this treatment.”
- 2006 pilot studies (monocentric and multicentric, respectively) on the use of repeated pulses of HD-DXM in untreated ITP patients:
- Single center study:
- 37 patients with severe ITP.
- Age at least 20 years and no more than 65 years.
- HD-DXM was given in 4-day pulses every 28 days, for 6 cycles.
- Response:
- Response rate was 89.2%.
- Relapse-free survival (RFS) was 90% at 15 months.
- Long-term responses (median time of 26 months) were 25 of 37 (67.6%).
- In the multicenter study:
- 95 patients with severe ITP.
- Age at least 2 years and no more than 70 years.
- HD-DXM was given in 4-day pulses every 14 days, for 4 cycles.
- 90 patients completed 4 cycles.
- Response
- Response rate (85.6%) was similar in patients classified by age (< 18 years, 36 of 42 85.7%; > 18 years, 41 of 48 85.4%).
- RFS at 15 months 81%.
- Long-term responses (median time of 8 months) were 67 of 90 (74.4%).
- In both studies, therapy was well tolerated.
- Single center study:
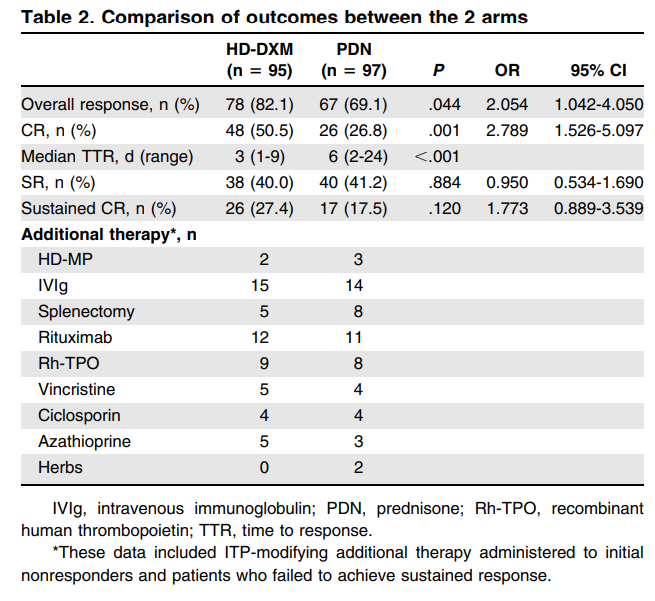
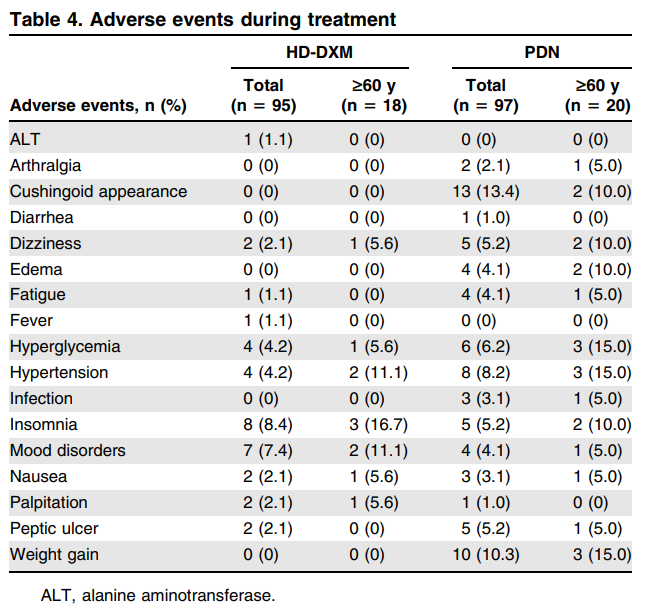
- 2016 prospective multicenter randomized trial of HD-DXM vs. prednisone for treatment of adult immune thrombocytopenia:
- Patients eligible for enrollment were aged 18 years or older.
- Patients enrolled were randomized to receive DXM 40 mg/d for 4 days (n = 95, nonresponses received an additional 4-day course of DXM17) or prednisone 1.0 mg/kg daily for 4 weeks and then tapered (n = 97).18
- End points:
- The primary end points were:
- Initial response, assessed by:
- Day 10 in the HD-DXM arm
- Day 28 in the PDN arm
- Sustained response, assessed by:
- Platelet count maintained >30 x 109/L with an absence of bleeding symptoms or no requirement for additional ITP-modifying treatment of 6 consecutive months following achievement of initial response.
- Initial response, assessed by:
- CR was defined as platelet count >100 x 109/L and absence of bleeding.
- Response was defined a as platelet count >30 x 109/L and at least 2-fold increase of the baseline count and absence of bleeding.
- The primary end points were:
- Baseline characteristics were comparable between the 2 arms.
- Initial response:
- Compared with prednisone, HD-DXM resulted in a:
- Higher incidence of:
- Overall initial response (82.1% vs 67.4%, = .044)
- Complete response (50.5% vs 26.8%, P = .001)
- Shorter median time to response (P< 0.001):
- 3 days (range 1-9) in HD-DXM arm
- 6 days (range 2-24) in PDN arm
- More effective control of bleeding (P = .028)
- Higher incidence of:
- Compared with prednisone, HD-DXM resulted in a:
- Sustained response 40.0% of patients in the HD-DXM arm and 41.2% in the PDN arm (P = .884).
- HD-DXM was generally tolerated better.19
- No deaths were recorded throughout the treatment or the follow-up periods.
- Author’s conclusion: “HD-DXM could be a preferred corticosteroid strategy for first-line management of adult primary ITP.”
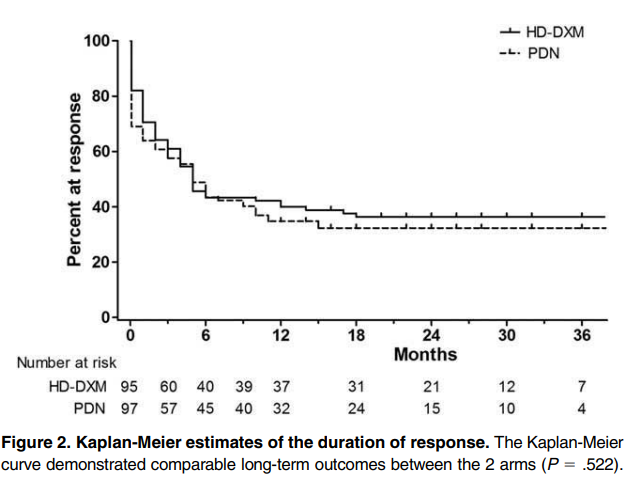
curve demonstrated comparable long-term outcomes between the 2 arms (P = .522).
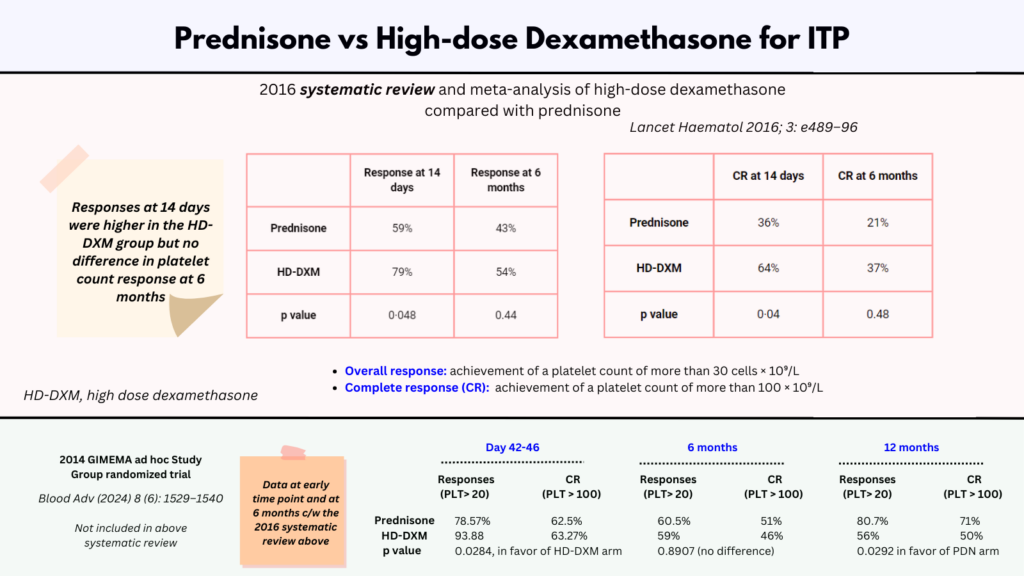
- 2024 GIMEMA ad hoc Study Group randomized trial:20
- Multicenter, prospective, randomized, controlled, open-label, phase 3 clinical trial.
- 113 patients with newly diagnosed adult primary ITP were treated with prednisone vs high-dose dexamethasone.21
- Inclusion criteria included:
- Signed informed consent
- New diagnosis of primary ITP
- Previously untreated
- Adult patients aged ≥18 years but ≤80 years
- Platelet count of ≤20 × 109/L or >20 × 109/L but <50 × 109/L plus bleeding score of ≥8
- Treatment scheme:22
- Prednisone was administered orally at a dose of 1 mg/kg per day for 4 consecutive weeks (from day 0-day 28), then, after day 28 PDN was tapered off in 14 days.23
- Dexamethasone was administered orally at single fixed daily dose of 40 mg for 4 consecutive days, every 14 days, for 3 consecutive courses
- Response criteria were:
- Complete response (CR), platelet count of ≥100 × 109/L
- Partial response (PR), platelet count ≥50 × 109/L but <100 × 109/L
- Minimal response (MR), platelet count of >20 × 109/L but <50 × 109/L
- No response (NR), platelet count of ≤20 × 109/L or platelet count >20 × 109/L but <50 × 109/L and bleeding score of ≥8.
- Relapse was defined as a platelet count decrease to levels of ≤20 × 109/L or >20 × 109/L but <50 × 109/L and bleeding score ≥8 after the assessment of the final response.
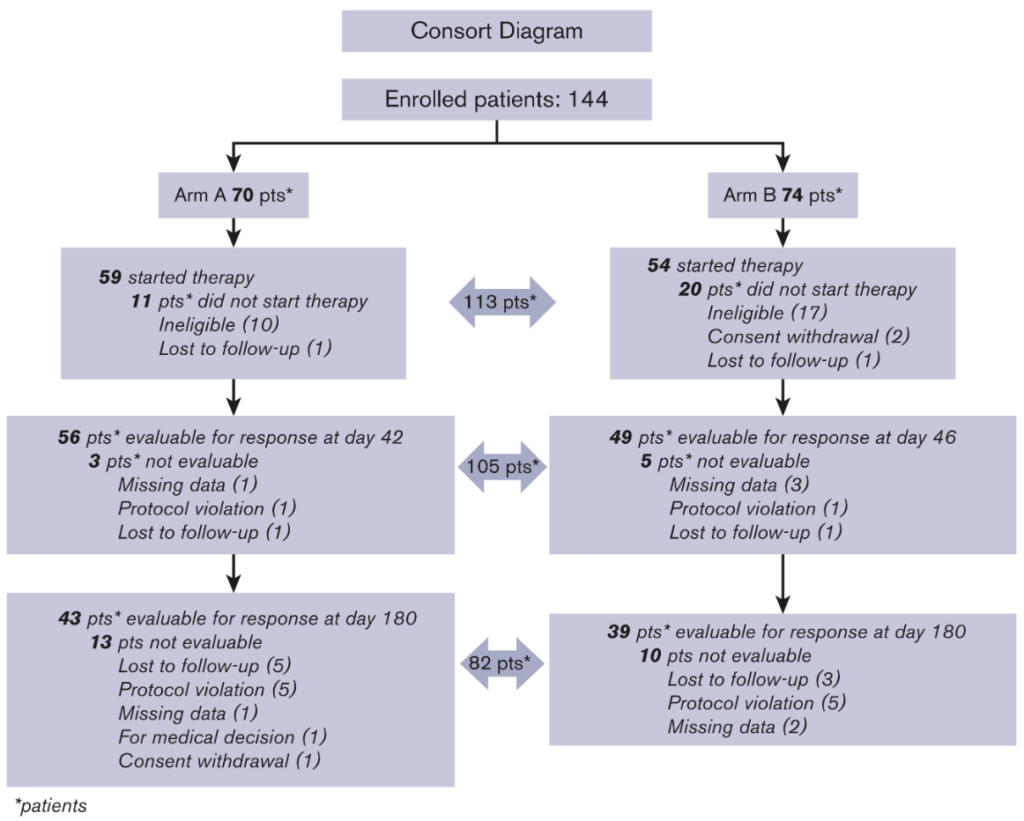
- 2024 GIMEMA ad hoc Study Group randomized trial (cont’d)
- Response
- Initial response:
- Assessed at:
- Day 42 for PDN arm
- Day 46 for HD-DXM arm
- 105 patients (56 in PDN arm, and 49 in HD-DXM arm) were evaluable.
- PDN arm:
- CRs in 35 (62.50%) patients
- PRs in 7 (12.50%)
- MRs in 2 (3.57%)
- NRs in 12 (21.43%)
- Total initial responses (CR + PR + MR) were 44 (78.57%)
- HD-DXM arm:
- CRs in 31 (63.27%) patients
- PRs in 11 (22.45%)
- MRs in 4 (8.16%)
- NRs in 3 (6.12%)
- Total initial responses (CR + PR + MR) were 44 (93.88%)
- The difference in initial response rate between the 2 arms was statistically significant (P = .0284), in favor of HD-DXM arm.24
- Assessed at:
- Final response
- Final response, assessed at day 180:25
- PDN arm:
- CRs in 22 (51.16%) patients
- PRs in 3 (6.98%)
- MRs in 1 (2.33%)
- NRs in 12 (27.91%)
- Total final responses (CR + PR + MR) were recorded in 26 of 43 (60.47%) patients
- HD-DXM arm:
- CRs in 18 (46.15%) patients
- PRs in 4 (10.26%)
- MRs in 1 (2.56%)
- NRs in 3 (7.69%)
- Total final responses (CR + PR + MR) were recorded in 23 of 39 (58.97%) patients
- The difference in final response rate between the 2 study arms was not statistically significant.26
- PDN arm:
- Persistent response assessed at 12 months:27
- PDN arm:
- CRs in 22 (70.97%) patients
- PRs in 1 (3.23%)
- MRs in 2 (6.45%)
- NR in 6 of 31 (19.35%)
- Total persistent responses (CRs + PRs + MRs) were observed in 25 of 31 (80.65%) in PDN arm.
- HD-DXM arm:
- CRs in 18 (50%) of patients
- PRs in 2 (5.56%)
- MR in 0
- NRs in 16 (44.44%)
- Total persistent responses (CRs + PRs + MRs) were observed in 20 of 36 (55.56%) in HD-DXM arm.
- The difference between the 2 arms was statistically significant (P = .0292) in favor of PDN arm.
- PDN arm:
- Initial response:
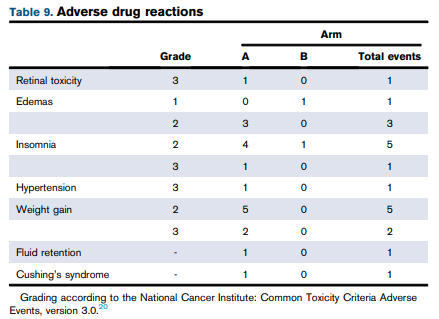
- Adverse drug reactions and adverse events:
- Adverse drug reactions:
- Nine patients experienced ≥1 adverse drug reactions:
- 7 patients in PDN arm
- 2 patients in HD-DXM arm
- In 7 of 9 patients adverse drug reactions occurred before day 180.
- Nine patients experienced ≥1 adverse drug reactions:
- Severe adverse events:
- PDN arm:
- One patient experienced depression:
- 26 days after the start of therapy.
- “Probably related to treatment”.
- One patient had bronchopneumonia:
- 13 days after the start of therapy.
- “Possibly related to PDN”.
- One patient experienced depression:
- HD-DXM arm:
- One patient experienced appendicitis:
- 34 days after therapy start.
- “Considered unrelated to HD-DXM”.
- One patient experienced appendicitis:
- Authors: “We emphasize that HD-DXM courses were better tolerated than standard-dose PDN, as also reported in the literature“.28
- PDN arm:
- Adverse drug reactions:
- Response
- 2024 GIMEMA ad hoc Study Group randomized trial (cont’d)
- Authors conclusions:
- “[The] results seem to indicate that HD-DXM allows an effective initial response but a response less long lasting over time than that obtained with PDN.”
- Authors conclusions:
Systematic Reviews
- 2016 systematic review and meta-analysis of high-dose dexamethasone compared with prednisone for previously untreated primary immune thrombocytopenia:
- Nine randomized trials (n=1138) were included. Of those, five (n=533) compared one to three cycles of dexamethasone (40 mg per day for 4 days) with prednisone (1 mg per kg) for 14–28 days followed by dose tapering in adults.
- The trials comparing prednisone with HD-DXM were:
- Wei Y, Ji XB, Wang YW, et al. High-dose dexamethasone vs prednisone for treatment of adult immune thrombocytopenia: a prospective multicenter randomized trial. Blood 2016; 127: 296–302.
- Bae SH, Ryoo HM, Lee WS, et al. High dose dexamethasone vs. conventional dose prednisolone for adults with immune thrombocytopenia: a prospective multicenter phase III trial. Blood 2010; 116: 3687.
- Din B, Wang X, Shi Y, Li Y. Long-term effect of high-dose dexamethasone with or without low-dose dexamethasone maintenance in untreated immune thrombocytopenia. Acta Haematol 2015; 133: 124–28.
- Mashhadi MA, Kaykhaei MA, Sepehri Z, Miri-Moghaddam E. Single course of high dose dexamethasone is more effective than conventional prednisolone therapy in the treatment of primary newly diagnosed immune thrombocytopenia. Daru 2012; 20.
- Praituan W, Rojnuckarin P. Faster platelet recovery by high-dose dexamethasone compared with standard-dose prednisolone in adult immune thrombocytopenia: a prospective randomized trial. J Thromb Haemost 2009; 7: 1036–38.
- Long-term response was defined as the achievement of a platelet count of more than 30 cells × 10⁹/L (overall response) or more than 100 cells × 10⁹/L (complete response) at 6 months or longer without concomitant treatment.
- Initial responses were reviewed within 14 days in all trials except one which assessed responses at 28 days in the prednisone group only.
- Pooling data from randomized trials, we found no difference in platelet count response at 6 months in adults treated with 1–3 cycles of high-dose dexamethasone or standard-dose prednisone; durable clinical outcomes were similar with either regimen:
- Overall platelet count response: pooled proportions 54% vs 43%; relative risk [RR] 1·16 [95% CI 0·79–1·71]; p=0·44).
- Complete platelet count response: 37% vs 21%, RR 1·49 [95% CI 0·50–4·48]; p=0·48).
- However, responses at 14 days were higher in the HD-DXM group:
- Initial overall platelet count response (79% vs 59%, RR 1·22 [95% CI 1·00–1·49], p=0·048)
- Complete response (64% vs 36%, RR 1·67 [95% CI 1·02–2·72], p=0·040)
- The dexamethasone group had fewer reported toxicities.29
- The results support findings of a previous study showing that the choice of initial corticosteroid probably does not impact the natural history of immune thrombocytopenia in adults
Clinical Practice Guidelines
- 2019 updated international consensus report on the investigation and management of primary immune thrombocytopenia:
- Corticosteroids remain the standard initial treatment of newly diagnosed patients and should be used for a limited time.
- Corticosteroids have multiple beneficial hemostatic effects on platelets by:
- Decreasing platelet clearance
- Increasing platelet production.
- +/- Reducing bleeding, independent of the platelet count increase, via a direct effect on blood vessels.6
- “Although the consensus panel believed that some patients were able to maintain a platelet response to a daily dose of predniso(lo)ne < 5 mg, the side effects of corticosteroids outweigh their benefits in the long-term.”
- “There are multiple small trials on prednisone and dexamethasone with various outcomes. In a meta-analysis of high-dose dexamethasone vs prednisone, there was no difference in platelet count response at 6 months; however, high-dose dexamethasone led to faster responses without additional toxicity.”
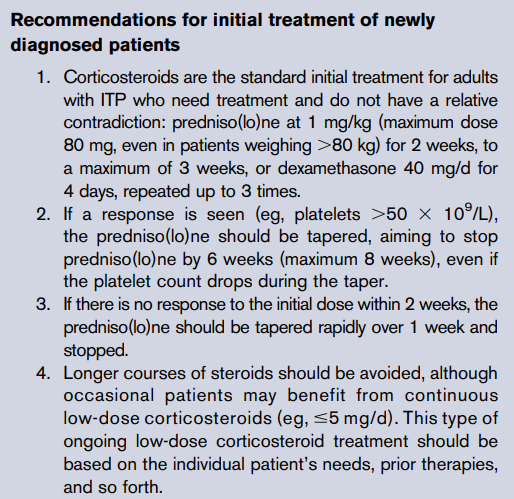
- American Society of Hematology 2019 guideline for immune thrombocytopenia:
- CORTICOSTEROIDS VS OBSERVATION. Recommendation 1a. In adults with newly diagnosed ITP and a platelet count of <30 x 109 /L who are asymptomatic or have minor mucocutaneous bleeding, the American Society of Hematology (ASH) guideline panel suggests corticosteroids rather than management with observation (conditional recommendation based on very low certainty in the evidence of effects)
- DURATION AND TYPE OF CORTICOSTEROIDS. Recommendation 3. In adults with newly diagnosed ITP, the ASH guideline panel recommends against a prolonged course (.6 weeks including treatment and taper) of prednisone and in favor of a short course (<6 weeks) (strong recommendation based on very low certainty in the evidence of effects.30
- In adults with newly diagnosed ITP, the ASH guideline panel suggests either prednisone (0.5-2.0 mg/kg per day) or dexamethasone (40 mg per day for 4 days) as the type of corticosteroid for initial therapy (conditional recommendation based on very low certainty in the evidence of effects Å◯◯◯). Remark: If a high value is placed on rapidity of platelet count response, an initial course of dexamethasone may be preferred over prednisone, given that dexamethasone showed increased desirable effects with regard to response at 7 days.)31
Expert opinion
- UpToDate:
- Glucocorticoids raise the platelet count in approximately two-thirds of patients with ITP. Most responses occur within two to five days but may take up to two weeks.
- The mechanism is uncertain but may involve increased apoptotic death of autoantibody-producing lymphocytes and downregulation of macrophage activity responsible for platelet phagocytosis.
- The most common treatment regimens are:
- Pulse dexamethasone
- Typically administered as 40 mg orally or intravenously once per day for four days with no taper. T
- Oral prednisone with a taper
- Typically administered as 1 mg/kg orally, once per day (range, 0.5 to 2 mg/kg daily) for one to two weeks, followed by a gradual taper, typically completed over less than six weeks.
- Administration of glucocorticoids for longer than six weeks should be avoided to minimize side effects.
- If there is no platelet count response after two weeks, a faster taper (over one week) can be used
- Pulse dexamethasone
- The choice among glucocorticoids is individualized. Practice is variable:
- Reasons to prefer dexamethasone include:
- Faster responses
- Reduced risk of dose confusion
- No need for dose tapering
- Completion of therapy in four days
- Fewer bleeding events
- Reasons to prefer prednisone include greater ability to titrate therapy to match the patient’s individual response.
- In our experience, the overall effectiveness of prednisone and high-dose dexamethasone are similar.
- Reasons to prefer dexamethasone include:
- David Garcia, MD in Hematologist: ASH News and Reports, commenting on the 2016 prospective multicenter randomized trial of HD-DXM vs. prednisone for treatment of adult ITP:
- “The results of this randomized, controlled trial suggest that HD-DXM may have some important advantages over a more traditional, longer course of prednisone for the initial treatment of ITP:
- First, this option would likely be preferred by many patients simply on the basis of convenience. For most patients, a four-day course of treatment (with one possible iteration 10 days later) will be much less burdensome than a two- to three-month course of therapy.
- This trial indicates that both interventions will cause a small number of patients to experience insomnia or mood disorder, but there is no evidence from this study that the frequency of these psychotropic effects would be significantly more common with HD-DXM.
- Alternatively, adverse effects typically associated with longer steroid exposures (weight gain, Cushingoid facies, and hyperglycemia) can be expected more frequently with a prednisone taper.
- Finally, since more than half of adult patients will ultimately require some treatment other than corticosteroids, the HD-DXM strategy may offer the advantage of permitting the clinician to identify which patients will require additional therapy (e.g., splenectomy, rituximab or a thrombopoietin mimetic agent) sooner.
- If the physician and the patient value these potential advantages, they can now proceed with HD-DXM knowing that it is at least as effective as a prednisone taper for both short- and long-term responses.”
- “The results of this randomized, controlled trial suggest that HD-DXM may have some important advantages over a more traditional, longer course of prednisone for the initial treatment of ITP:
See Quiz.
