Tutorial
TBP Tweetorial

White Blood Cell Count and Differential
The white cell count represents the total concentration of all circulating leukocytes in the blood. A normal count in adults is between 4-11.
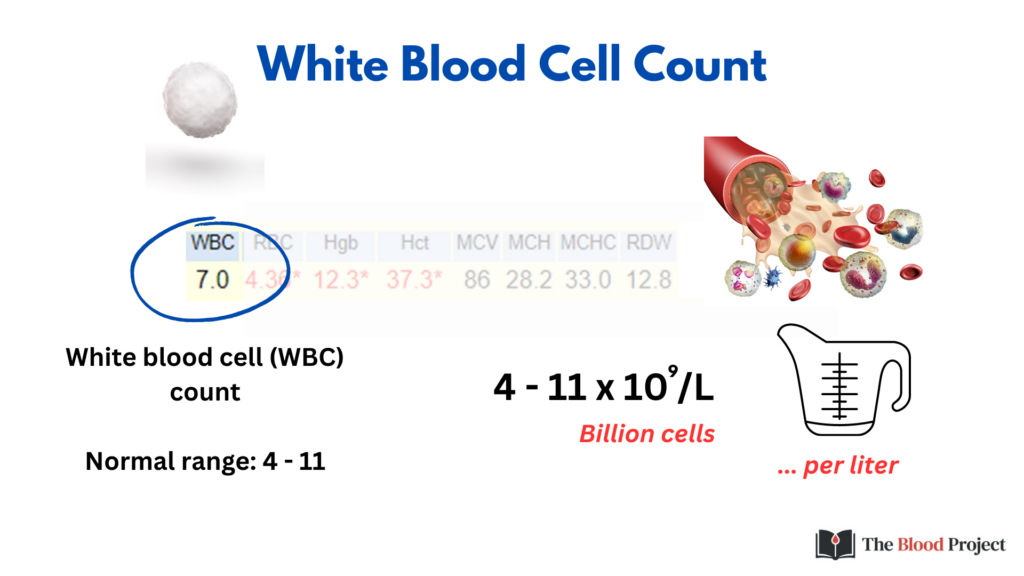
109 is a billion cells!
Numbers this large are hard to grasp. Consider this comparison: if we were to stack one billion pennies, they would fill the equivalent of five school buses.
For more details on how white blood cells are counted, click here.
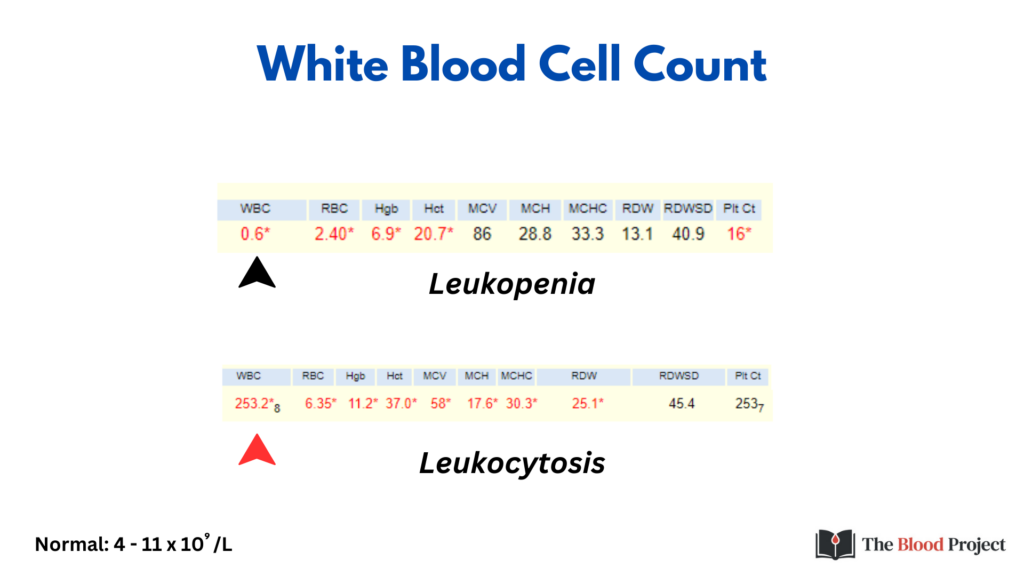
Here are CBC results from 2 patients showing polar opposites in total WBC counts. On the top is a patient with a low white cell count or leukopenia – a mere 0.6 x 109/L or 600/ul. On the bottom is a patient with a grossly elevated white cell count or leukocytosis.
It’s really hard to know what is going on in either case, without opening the hood and counting the various subtypes of white blood cells.
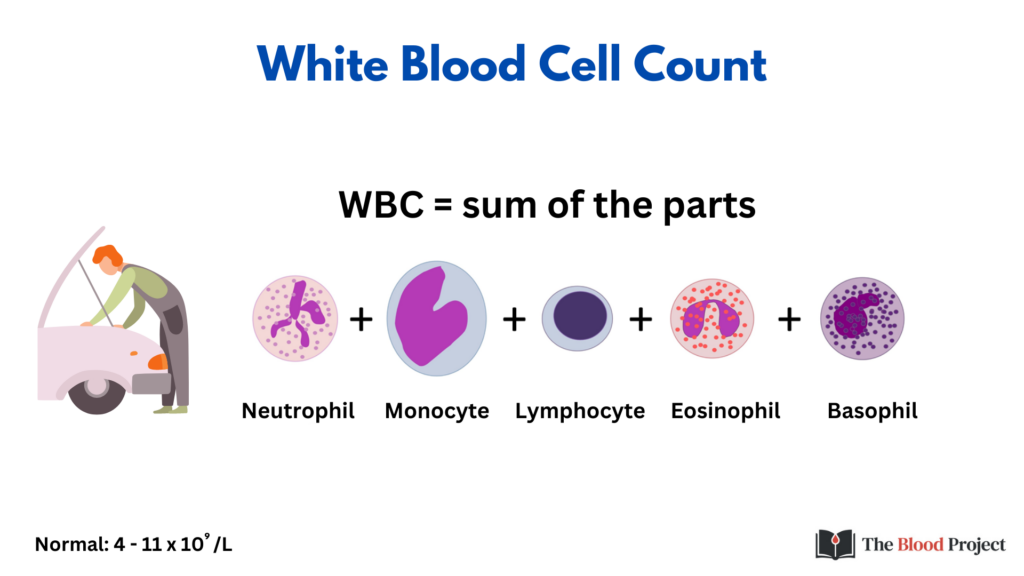
There are normally 5 white blood cell types in the blood:
- Neutrophils, which participate in:
- The acute inflammatory response to bacterial infection.
- Removal of bacteria by phagocytosis.
- Monocytes, which:
- Differentiate into macrophages in tissues where they function as antigen-presenting cells.
- Play important roles in phagocytosis of bacteria, cells, debris.
- Lymphocytes, which:
- Mediate the acquired immune response.
- Eosinophils, which are involved in:
- Allergic reactions.
- Host deference against parasitic infection.
- Basophils:
- Have a high affinity for binding IgE antibodies on their surface.
- Participate as effector cells in allergic reactions.
Under pathological conditions, other white cell types may appear in the blood, including:
- Immature white cells
- Atypical white cells

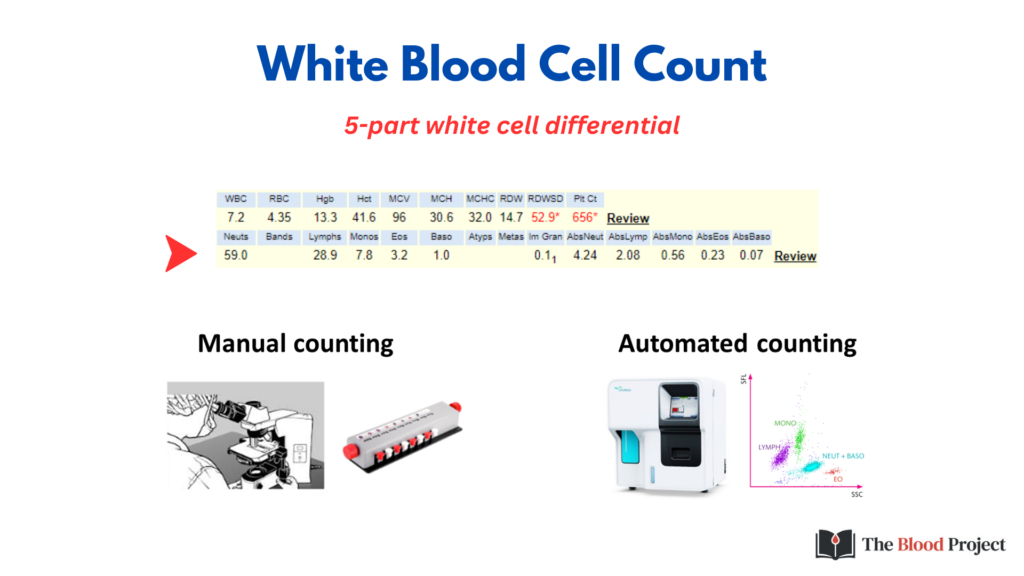
Quantitation or enumeration of morphologically distinct subpopulations of WBCs is called the 5-part white cell differential.
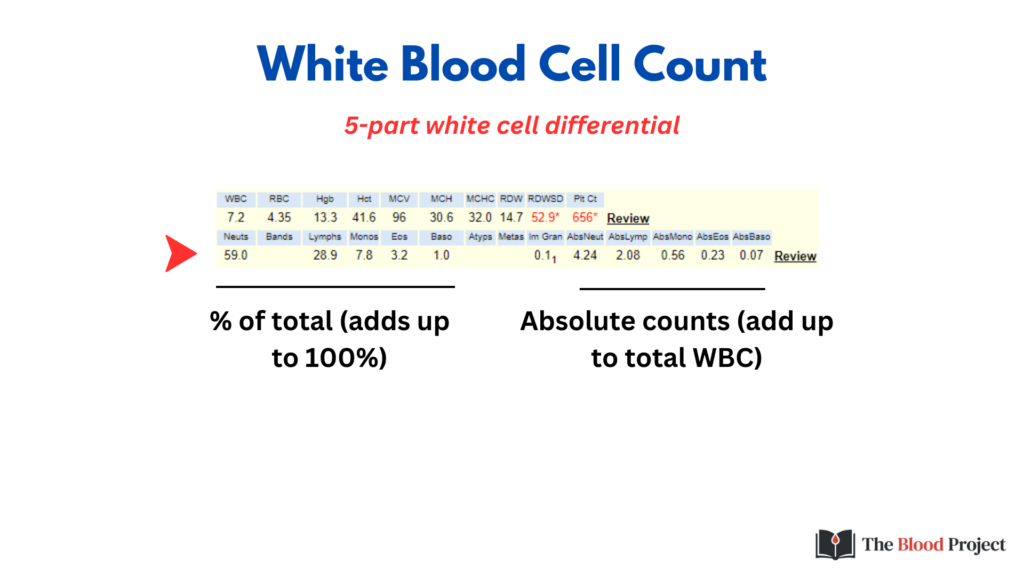
White blood cell subtypes are expressed as:
- % of the total white cell count. Under normal conditions, these numbers add up to 100%.
- Absolute counts, which add up to the total WBC count.
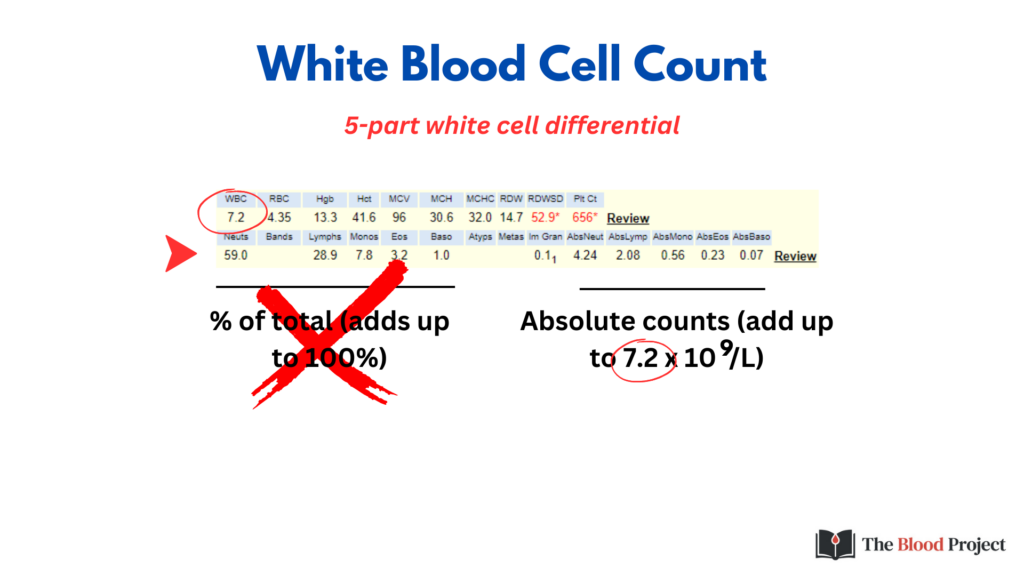
As a general rule of thumb, when considering the 5 mature subtypes of WBCs, it is best to ignore the % and focus on the absolute values.
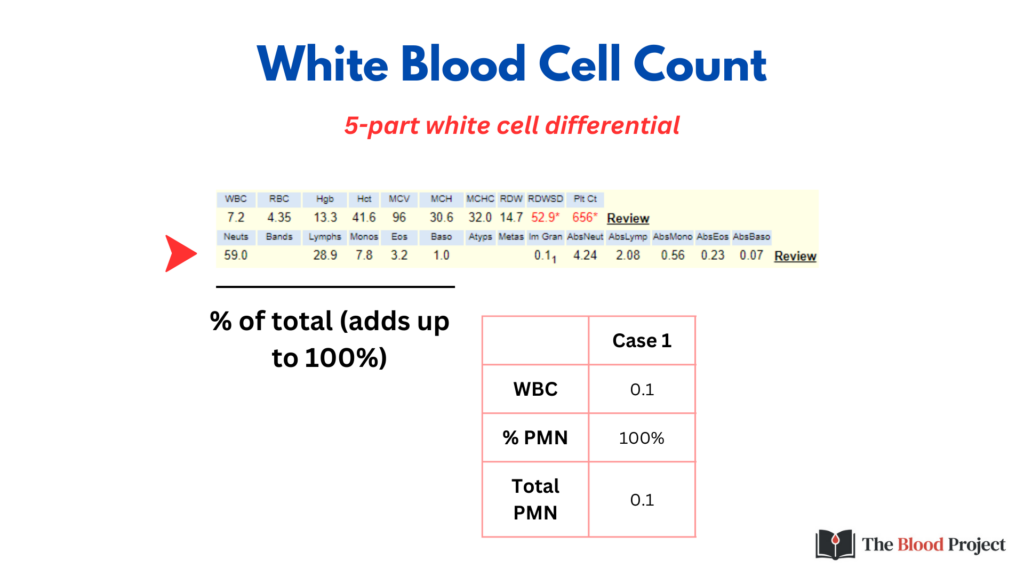
This slide shows a hypothetical example of how the % can be misleading. Consider the patient who has received large doses of chemotherapy and has a dangerously low white cell count – a mere 0.1 x 109/L. 100% of these cells are neutrophils. Sounds reassuring, right? But 100% of 0.1 x 109/L is still just 0.1 x 109/L! With an absolute neutrophil count (ANC) this low, the patient is at high risk for developing a lethal infection.
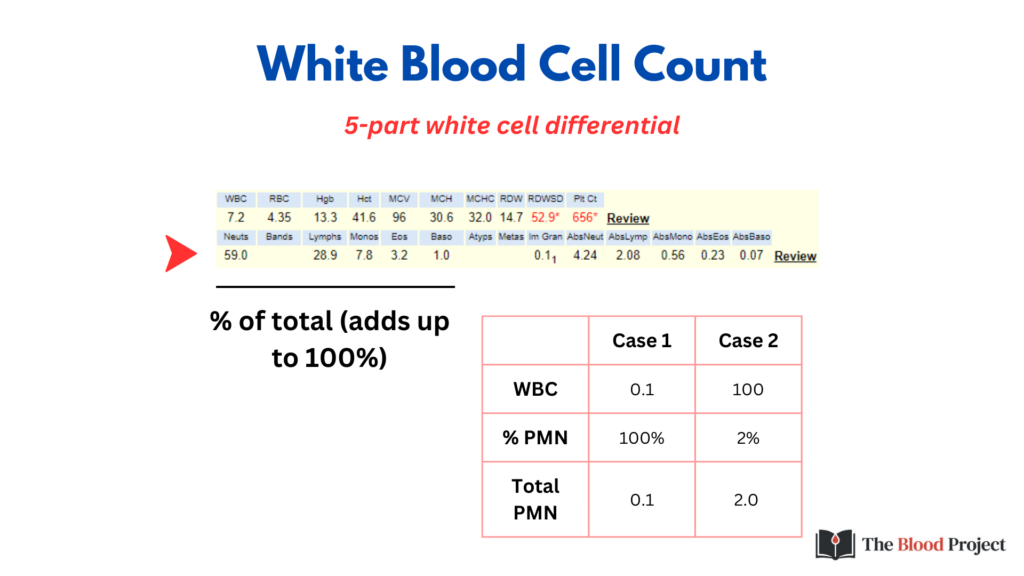
Here is another example of how the % can be misleading. This is a patient with chronic lymphocytic leukemia (CLL) whose total white cell count is 100 x 109/L. The vast majority of their circulating leukocytes are lymphocytes. The neutrophils comprise a tiny fraction, a mere 2%. Yet, 2% of such a high WBC count gives a perfectly normal absolute neutrophil count, and at the end of the day that’s all that matters.
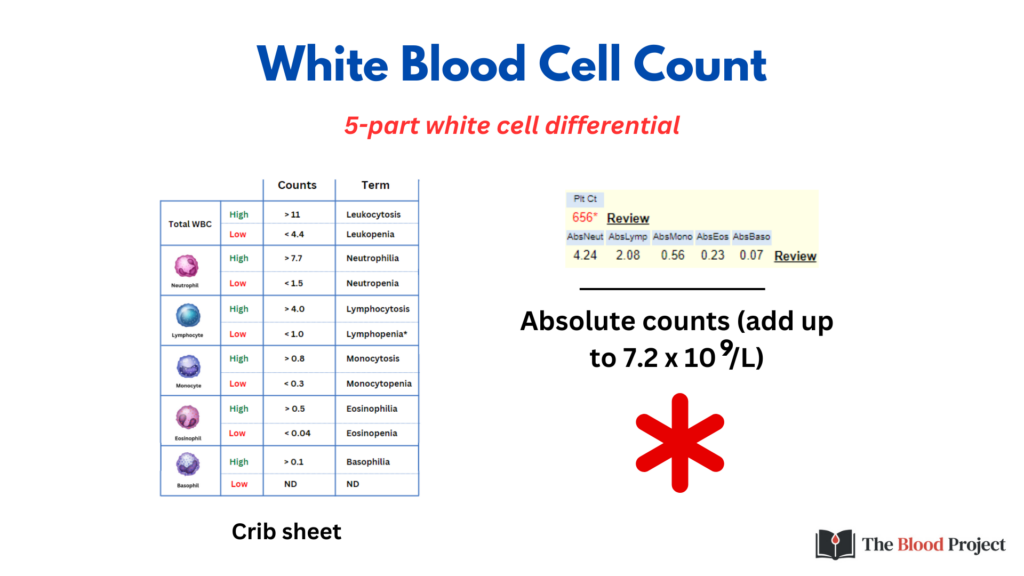
Our diagnostic and therapeutic decisions are based not on % counts, but rather on on absolute counts. Are they increased above the normal range or are they decreased? Alterations in each white cell subset – whether neutrophilia or neutropenia or eosinophilia or monocytosis – carry their own differential diagnosis and trigger their own unique order set and diagnostic workflow. It is helpful to keep in hand a crib sheet of normal ranges for quick reference (for downloadable version of the table, click here).

Note that normal WBC does not guarantee that the subsets are normal in number. In the following slides, we will look at some examples of this.
Example 1: Acute leukemia

Example 2: Hypereosinophilia

Example 3: Chronic myelomonocytic leukemia (CMML)
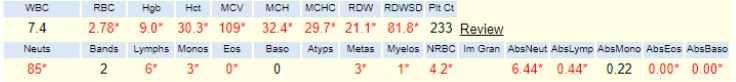
Example 4: Chronic lymphocytic leukemia (CLL)

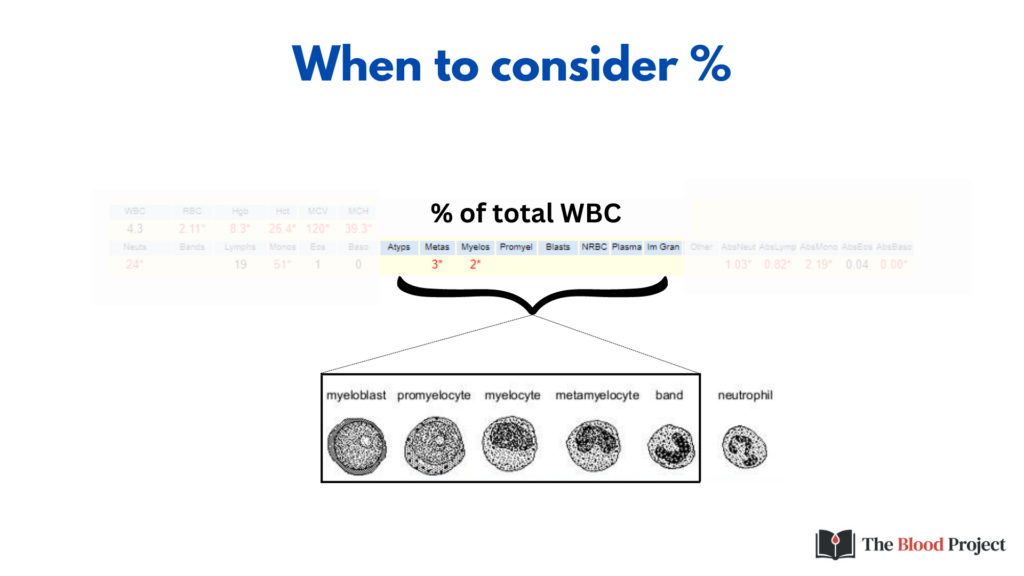
As much as it is preferable to use absolute counts when assessing the concentration of the 5 mature white cell types, it is more conventional to use percentages when enumerating immature white blood cells (in this example 3% metamyelocytes, 2% myelocytes) because they usually occur in very small numbers and because their mere presence (no matter how small in number) may be clinically significant.
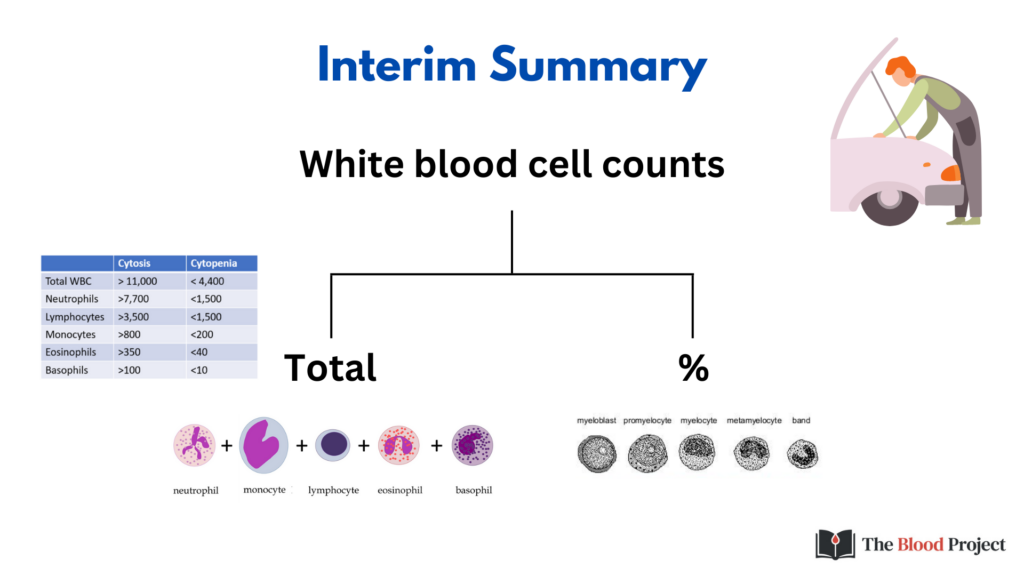
To summarize at this point, the assessment of the total WBC is merely a starting point. Don’t assume that a normal WBC means a normal differential. Depending on the clinical context, it is important drill down and enumerate the various white cell subsets. Be prepared to interpret the absolute numbers of mature WBCs and the % of immature WBCs.
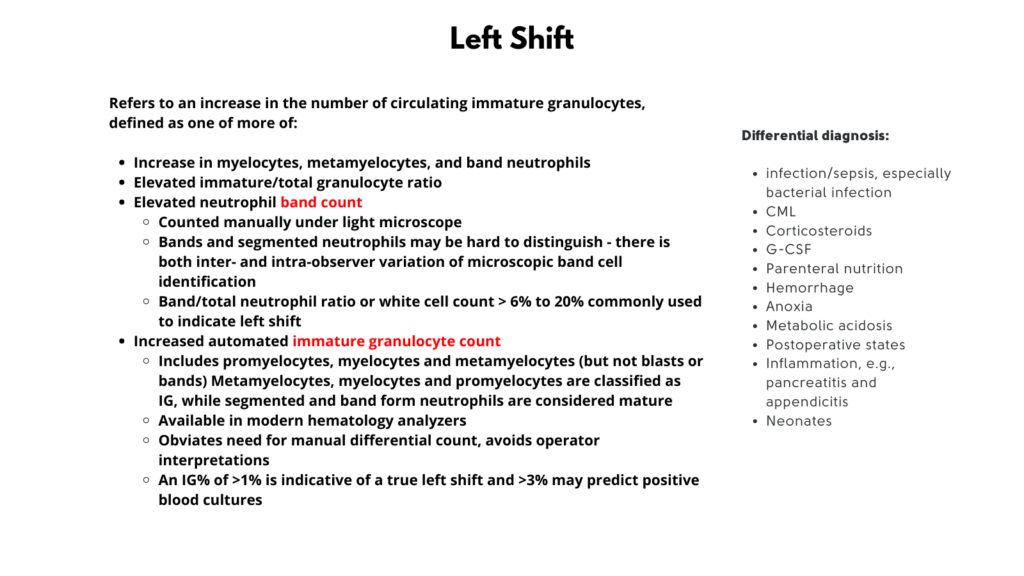
In the next few slides, we will discuss three issues that relate to the WBC count:
- Definitions of terms related to increased white blood cells
- Immature granulocytes
- Left shift
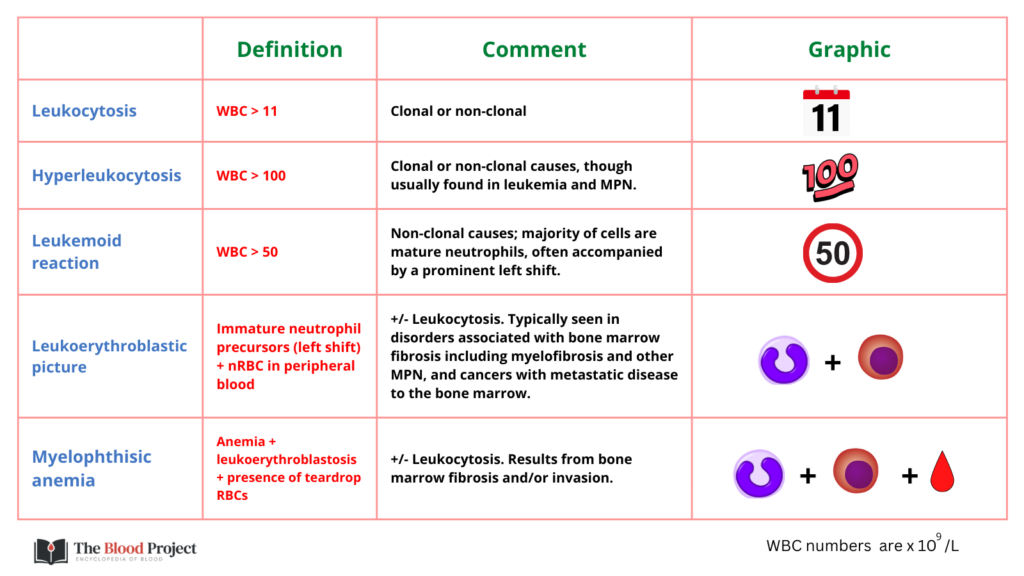
Definitions of terms related to increased white blood cells:

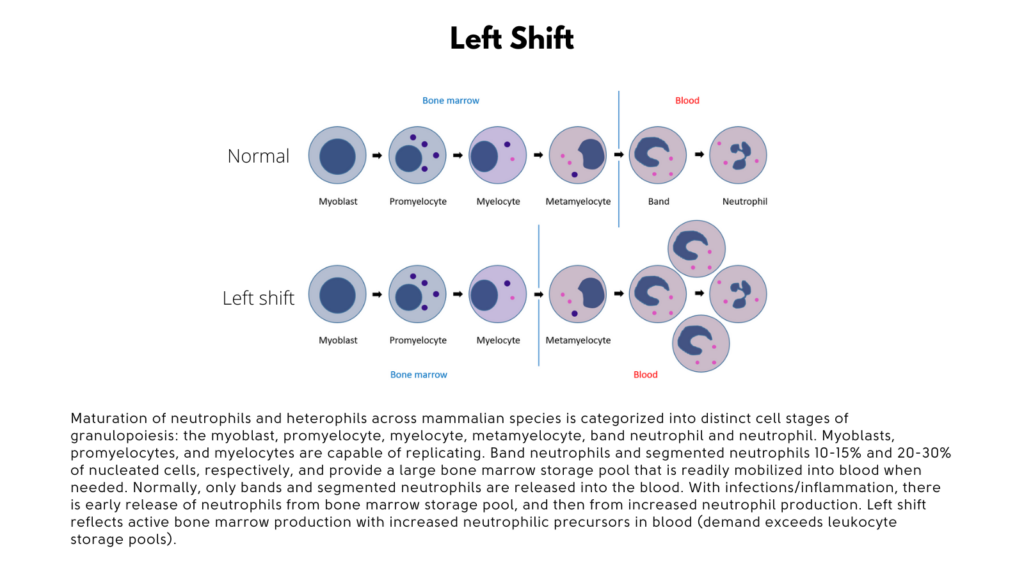
Most modern haematology analyzers have developed methods for quantitation of immature granulocytes (IG), specifically promyelocytes, myelocytes and metamyelocytes. These are typically reported as a percentage of the total white blood cell count. These analyzers cannot reliably distinguish bands from segmented neutrophils, so these are counted together. Eosinophilic or basophilic immature cells are not classified as IG.
- Under normal physiological conditions IG% is low, less than 1%
- Left shift – IG > 1%