Differential Diagnosis
When seeing a patient with thrombocytopenia, there are several ways to approach the differential diagnosis. For the last 2 classification schemes, click on the links for more detail:
1. According to whether or not the thrombocytopenia is real:
- Pseudothrombocytopenia
- True thrombocytopenia
2. According to whether the thrombocytopenia is congenital or acquired:
- Congenital (familial)
- Acquired
3. According to other changes in the complete blood count:
- Isolated thrombocytopenia – no other significant changes in the complete blood count.
- Thrombocytopenia associated with other abnormalities in blood counts.
4. According to the mechanism of thrombocytopenia:
- Decreased production
- Increased consumption/destruction
- Sequestration – hypersplenism, especially in setting of cirrhosis
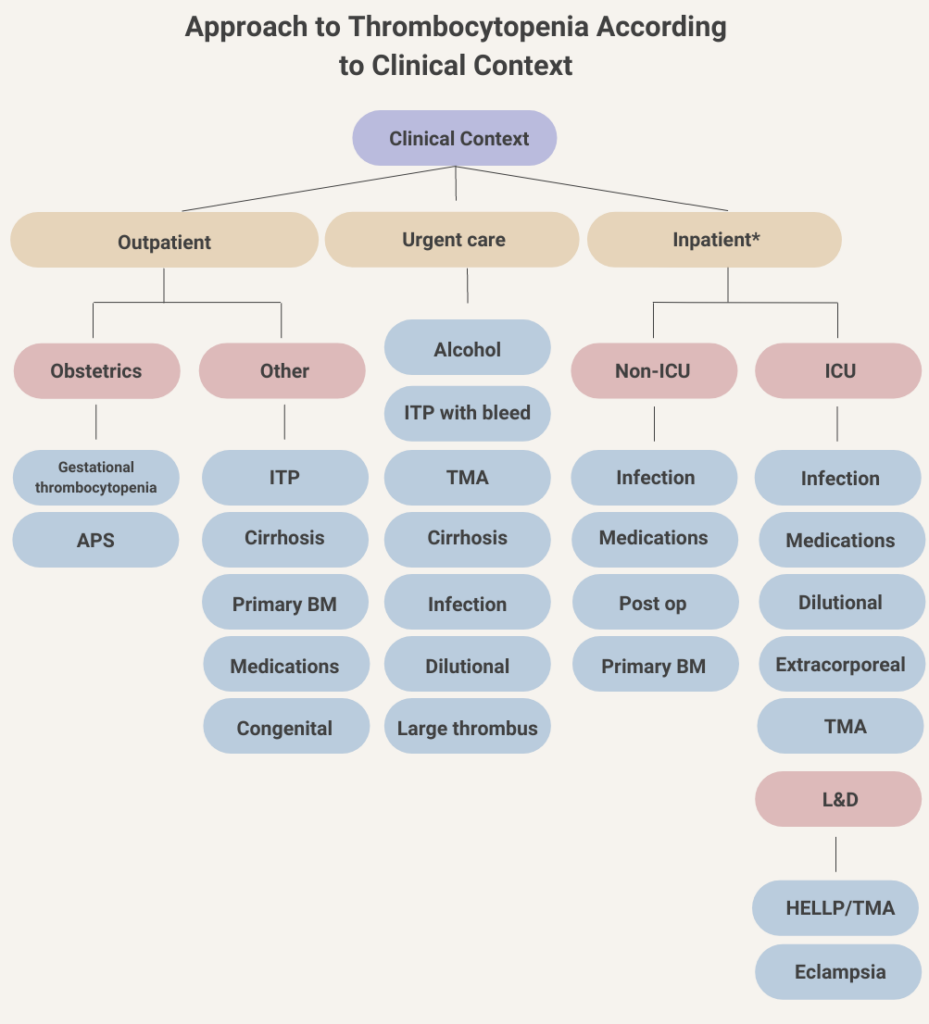
5. According to clinical context:
- Outpatient
- Emergency department
- Inpatient (new onset)
The most useful of these classifications is clinical context. The classification scheme, which is detailed here, can be conveniently organized as a flow chart:
In our case, we can focus on the differential diagnosis of isolated thrombocytopenia in an outpatient. The most common conditions include:
| Differential diagnosis | History & physical | Labs |
|---|---|---|
| Pseudothrombocytopenia | In vitro artifact, so patients are asymptomatic. | Peripheral smear to examine for platelet clumping. Repeat complete blood count in non-EDTA-containing tube. |
| Immune thrombocytopenia | Bleeding and easy bruising. Symptoms associated with causes of secondary ITP. Signs of mucocutaneous bleeding. | HCV, HIV, H. pylori to rule out secondary causes. |
| Drug-induced thrombocytopenia | History of drug intake, negative in this patient. | No specific testing. |
| Familial (congenital) thrombocytopenia (FT) | Family history of thrombocytopenia and/or bleeding. | Peripheral blood smear to examine for giant platelets (present in some but not all causes of FT). |
| Alcohol abuse | History of heavy drinking, which was negative in this patient. | No specific testing. |
| Cirrhosis | History/findings of liver disease, jaundice, encephalopathy, spider nevi, palmar erythema, splenomegaly. Negative history/physical exam in this patient. | Transaminases, bilirubin, PT, aPTT, albumin. |
| Antiphospholipid syndrome (APS) | History of thrombosis (or in case of women, pregnancy loss), livedo reticularis and other cutaneous manifestations, symptoms associated with secondary causes such as systemic lupus erythematosus. Negative history/physical exam in this patient. | Thrombocytopenia is usually mild (platelet count 50-150 × 109/L) and asymptomatic. Severe thrombocytopenia is extremely rare outside the context of APS-associated thrombotic microangiopathy. |
At this point, we only have a history and physical exam. We have not yet ordered lab tests. Based on what we know so far:

