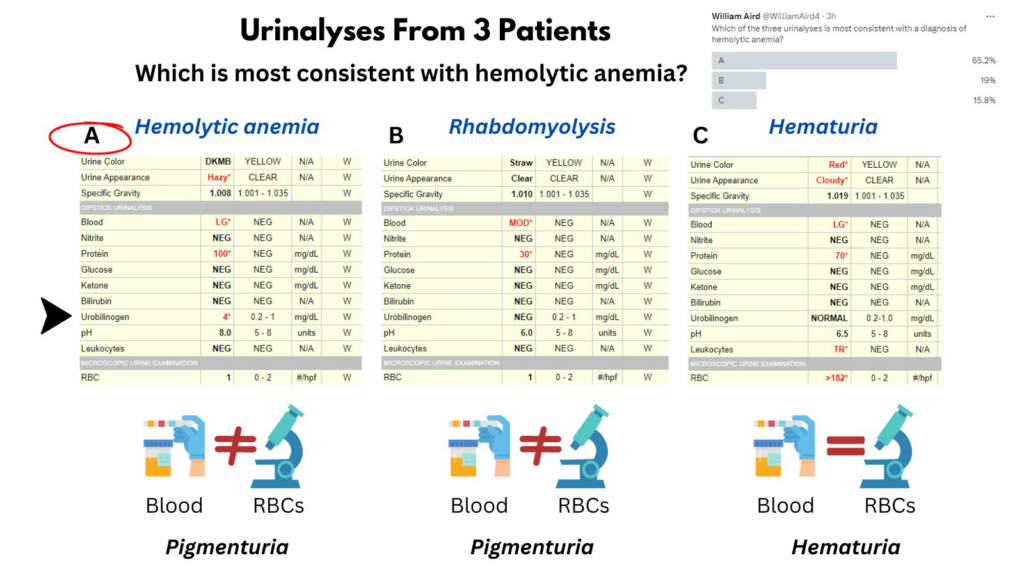
In a recent quiz, users were asked to identify which patient has hemolytic anemia based on their urinalysis. The correct answer was (A). How do we arrive at this answer?
- Discordance between positive blood on dipstick and negative red cells on microscopy = Hb or myoglobin in urine (pigmenturia) … so that eliminates C, in which both dipstick and microscopy were positive. This was a case of hematuria.
- A and B are c/w pigmenturia. If only one contains Hb (from hemolytic anemia) then the other must contain myoglobin (from rhabdomyolysis). How do we decide which is which? The amount of pigment (LG vs MOD) does not discriminate between the two.
.. but the urobilinogen does!
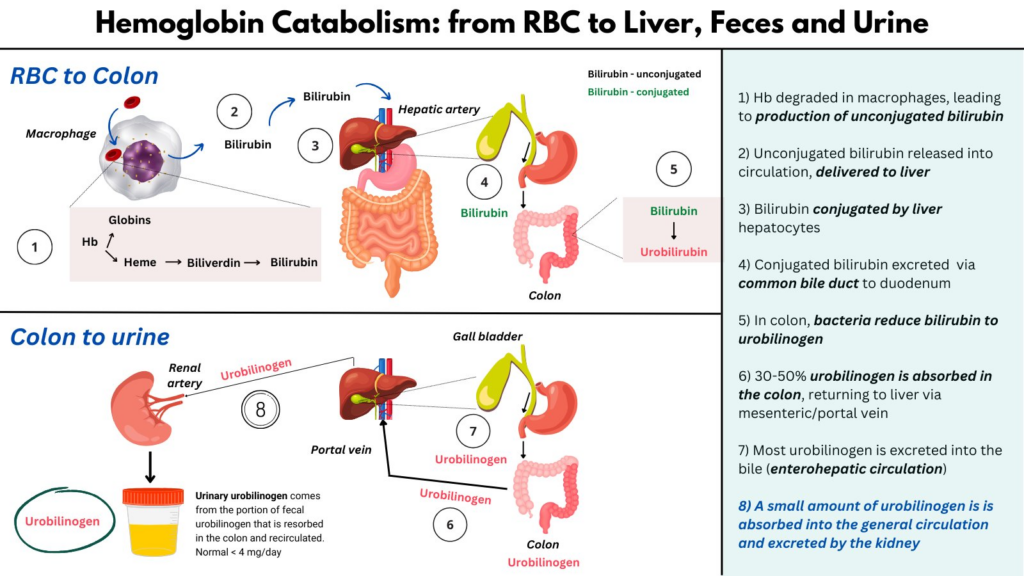
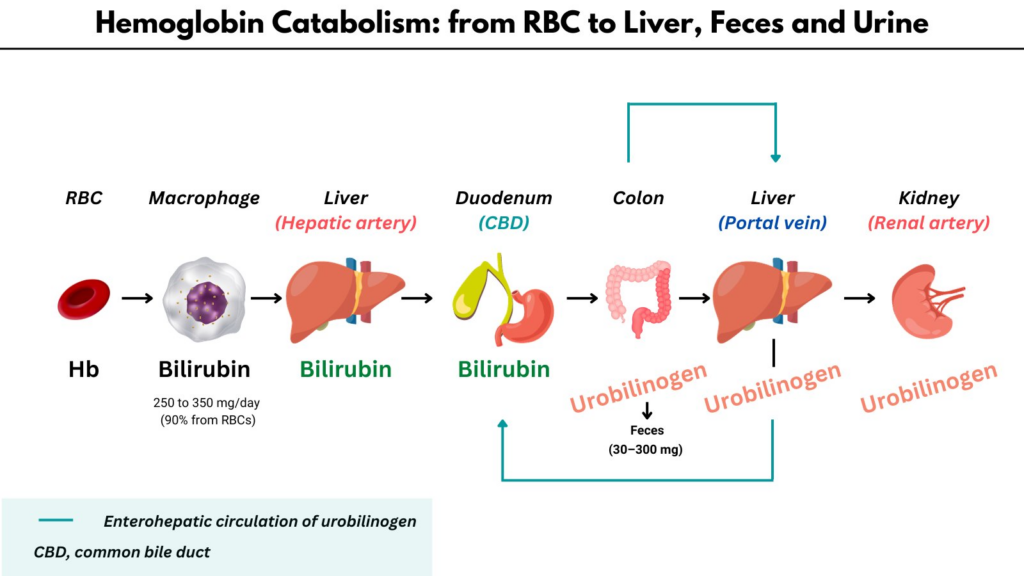
Urobilinogen is an end product of Hb metabolism. It is derived from bacterial degradation of bilirubin in the colon. Most is excreted in the feces, but some is reabsorbed and makes its way back to the liver.
From the liver, most urobilinogen is sent back out the common bile duct to the intestines (enterohepatic circulation) but a small amount leaks into the systemic circulation and is excreted in the urine (normally 4 mg/day, too low to see on a dipstick).
In hemolytic anemia, hemoglobin degradation and bilirubin production may increase 6-10 fold, which results in elevated urobilinogen production, absorption from the colon, and excretion in the urine.
Unfortunately, however, elevated urinary urobilinogen is neither specific (also seen in liver disease when the liver cannot excrete it properly) or sensitive for hemolysis.
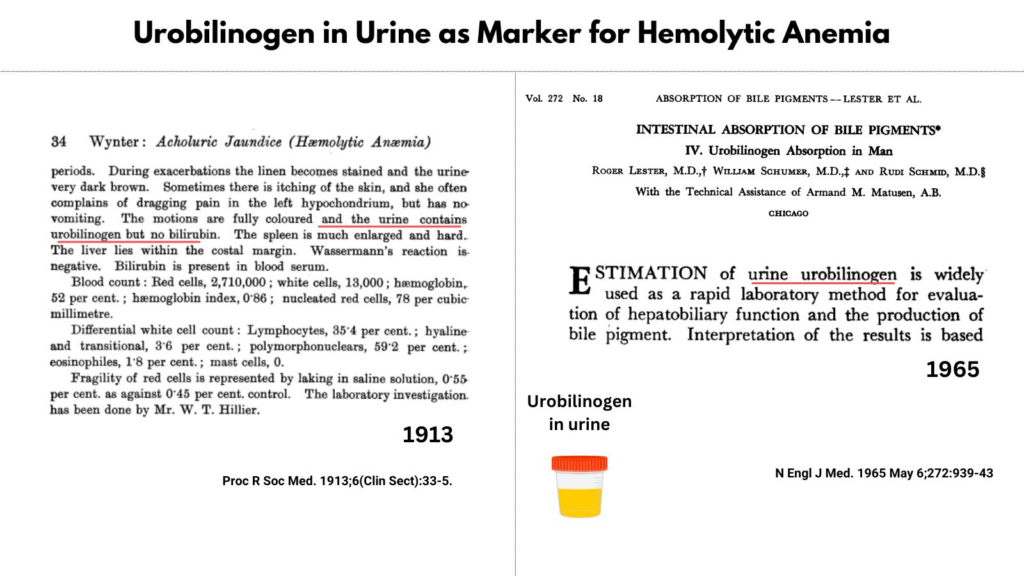
Interestingly, from a historical perspective, urinary (and fecal) urobilinogen was among the first tests used to diagnose hemolytic anemia!