For Your Healthcare Provider
Have your patient scan this QR code with their smartphone camera to instantly access this educational guide on their device.
A guide to what matters — and what usually doesn’t — on your blood count
Most patients now see their blood tests directly in the medical record. This is helpful, but a complete blood count (CBC) includes many numbers, and electronic systems highlight many of them in red even when they are not medically important. This guide explains which values matter most, which ones you can usually ignore, and when you should contact your doctor.
This page explains individual CBC values in detail. For a big-picture overview of how doctors interpret these numbers and decide what matters most, see our CBC overview.
Access the Resources
The ABCs of the CBC
A CBC tells us about three types of cells made in your bone marrow:
- White blood cells (WBCs) – help fight infection
- Red blood cells (RBCs) – carry oxygen
- Platelets – help stop bleeding
Not every number on the CBC is equally important.
The Three Key Numbers to Focus On
1. White Blood Cell Count (WBC)
The total number of white cells, which help fight infections.
In most labs, the white blood cell count is usually between 4,000 and 11,000 cells/µL (or 4-11 x 109/L)
What matters:
- Very low counts → higher infection risk
- Very high counts → infection, inflammation, or (rarely) a blood disorder
- Trends over time
What usually doesn’t matter:
- Slight increases with stress, exercise, pain, or mild illness
- Small day-to-day fluctuations
This is one of the three most important numbers on your CBC.
A note about the differential:
The CBC tells you only the total number of white blood cells. The total WBC is like reading the odometer of a car — it gives an overall number, but not what’s happening under the hood. Sometimes your doctor also orders a differential, which breaks the total into types of white cells (neutrophils, lymphocytes, and monocytes, eosinophils and basophils).
The differential can be important because:
- It helps explain why the WBC is high or low
- Subtle changes in white cell types can matter even when the total WBC is normal
- It helps guide whether further testing is needed
Patients do not need to interpret the differential themselves, but your doctor may look closely at it if the WBC is abnormal — or even if it is normal but symptoms or trends suggest something more is going on.
2. Hemoglobin or Hematocrit
When we talk about red blood cells, doctors do not rely on the “red blood cell count.” Instead, we look at hemoglobin or hematocrit, because these numbers tell us how much oxygen your blood can carry. They rise and fall together and give very similar information.
Typical ranges:
- Hemoglobin:
- Women: ~12–16 g/dL
- Men: ~13.5–17.5 g/dL
- Hematocrit:
- Women: ~36–46%
- Men: ~41–53%
What matters:
- A hemoglobin or hematocrit that is lower than normal (anemia)
- A hemoglobin or hematocrit that is higher than normal, which may indicate polycythemia
- Symptoms such as fatigue, shortness of breath, headaches, dizziness, or redness of the skin
- Trends over time, not single values
- Trends over time, especially a steady rise or fall
- Significant changes compared with your prior CBCs
What doesn’t matter:
- Small day-to-day fluctuations
- Minor differences between hemoglobin and hematocrit
- A slightly high or low RBC count when hemoglobin and hematocrit are normal
- A mildly high hematocrit during dehydration (often normalizes with hydration)
This is the second key number to look at.
3. Platelet Count
The total number of platelets, which help prevent bleeding.
In most labs, the platelet count is usually between 150,000 and 400,000 cells/µL (or 150-400 x 109/L).
What matters:
- A platelet count below 100,000, which usually means something is going on (often infection, inflammation, or a medication effect). This level does not automatically mean you are at risk of bleeding, but it does warrant attention from your doctor.
- A platelet count below ~50,000 may increase bleeding risk in certain situations, such as:
- if you are taking antiplatelet or anticoagulant medications
- if you need an invasive procedure or surgery
- A platelet count below ~10,000 increases the risk of spontaneous bleeding and always requires prompt medical evaluation.
- New symptoms such as unexpected bruising, nosebleeds, or bleeding gums.
- A very high platelet count is usually reactive (infection, inflammation, iron deficiency) but occasionally needs further evaluation.
What doesn’t matter:
- Platelet counts in the 100,000–150,000 range — these are often stable, long-standing, and not associated with increased bleeding risk.
- Temporary drops during illness, after exercise, or from certain medications.
- Mild elevation from inflammation, infection, or iron deficiency.
- A one-time abnormal value that normalizes on repeat testing.
Additional reassurance:
- Nature has given us a large safety buffer. You do not begin to lose normal clotting ability the moment your platelet count falls below 150,000. Many people walk around with platelets just under that level and have no bleeding problems at all.
- Sometimes a low platelet count is due to the platelets clumping in the test tube. If the number is unexpectedly low, your doctor may repeat the test or look at a peripheral smear to confirm the true count.
This is the third major CBC number worth your attention.
What About All the Other Numbers?
1. MCV (Mean Corpuscular Volume)
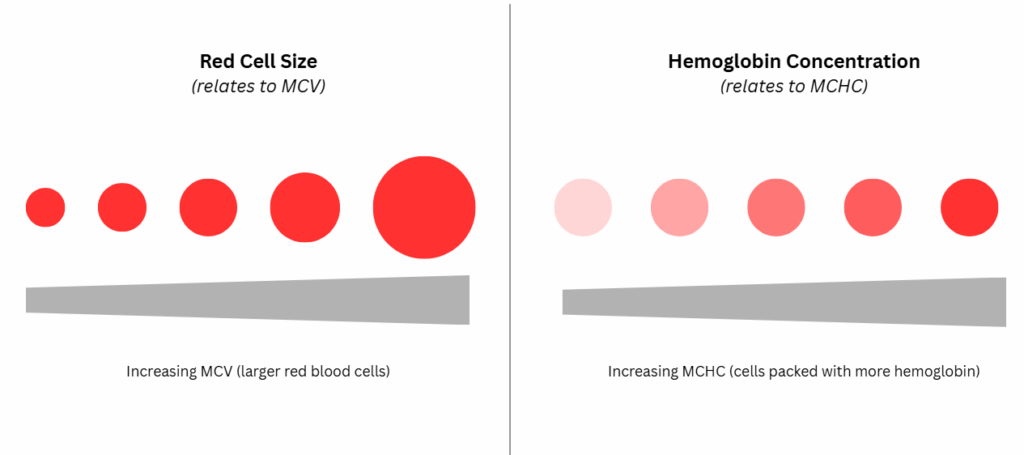
The MCV reflects the average (mean) size of red blood cells.
What matters:
- The MCV helps your doctor understand why anemia is present if your hemoglobin is low.
- It can support the overall picture when evaluating iron deficiency, vitamin levels, or other causes of anemia.
What usually doesn’t matter:
- A slightly high or low MCV on its own
- An MCV in the red when your hemoglobin and hematocrit are normal
- Day-to-day changes
Bottom line: The MCV is mainly a tool for your doctor when interpreting anemia. Most patients do not need to focus on this number.
2. MCH (Mean Corpuscular Hemoglobin)
The MCH tells us how much hemoglobin is inside the average red blood cell. If you imagine a red cell as a tiny packet, the MCH is like emptying that packet onto a scale to see how much hemoglobin it contains.
What matters:
- Almost nothing — this number adds no useful information beyond what the MCV and hemoglobin already show.
- MCH usually moves in parallel with the MCV.
What usually doesn’t matter:
- Small changes in MCH
- A red “out of range” flag — this is very common and rarely meaningful
Bottom line: Patients can safely ignore this number. And truthfully, most hematologists can too — the MCH almost never changes clinical decisions.
MCHC (Mean Corpuscular Hemoglobin Concentration)
The MCHC is the average concentration of hemoglobin in each red cell. You can think of it like a sponge: two sponges can hold the same amount of water, but one may feel more “soaked” because the water is more concentrated inside it. MCHC is similar — it reflects how saturated the red cell is with hemoglobin.
What matters:
- The MCHC helps physicians understand the type of anemia when hemoglobin is low (for example, whether red cells are hypochromic, normochromic, or hyperchromic).
- It supports the overall interpretation of the CBC when your doctor is evaluating anemia.
What usually doesn’t matter:
- Mildly high or low values
- A red “out of range” flag — this is extremely common and almost never meaningful
- Small day-to-day changes in MCHC
Bottom line: Doctors use MCHC as part of the diagnostic workup for anemia, but patients do not need to interpret this number. On its own, an abnormal MCHC almost never means anything urgent.
RDW (Red Cell Distribution Width)
This measures how much the red blood cells vary in size. RDW appears in two forms on CBCs (RDW-CV and RDW-SD).
- Two types: RDW-CV and RDW-SD (RDW-SD is more meaningful if either matters).
- A high RDW is common and often benign, especially when hemoglobin and hematocrit are normal.
- Doctors mainly look at RDW only when evaluating anemia.
Understanding MCV and MCH at a glance
Why Are So Many Values in Red?
Electronic systems flag anything slightly outside a population range—even normal personal variation.
A value in red:
- does not mean something is wrong
- does not require treatment
- is often completely normal for you
Doctors interpret the CBC in context: your symptoms, medical history, and trends over time.
Quick Reference Table
| CBC Value | What It Tells You | When to Worry | Usually Not Important |
|---|---|---|---|
| WBC | Immune function | Very high or very low | Small daily changes |
| Hemoglobin/Hematocrit | Oxygen-carrying ability | Low + symptoms | Small fluctuations |
| Platelets | Clotting ability | <100,000 or very high | Mild reduction or elevation |
| MCV/MCH/MCHC | Red cell details | Only during anemia evaluation | Routine interpretation |
| RDW | Red cell size variation | Rarely meaningful | Commonly in red |
Key Takeaways
- Most CBC values in red are not medically important.
- The three key numbers are WBC, hemoglobin (or hematocrit), and platelets.
- MCV, MCH, MCHC, RDW, and RBC count are mainly tools for physicians, not for patients.
- A normal hemoglobin/hematocrit means most of the other red-cell numbers aren’t important.
- Trends over time matter far more than any single number.
