For Your Healthcare Provider
Have your patient scan this QR code with their smartphone camera to instantly access this educational guide on their device.
A guide for patients with a low platelet count
Access the Resources
Note: The video and audio linked above were generated with the assistance of AI. Clinical accuracy has been reviewed, but no AI-generated content can be guaranteed to be fully error-free.
A low platelet count, or thrombocytopenia, can be unexpected and concerning when you first see it on a blood test.
Mild thrombocytopenia is common and often temporary, especially around illness, medications, or pregnancy, and does not automatically mean bleeding problems. Many people feel well, and the platelet count may improve as the underlying trigger resolves or remain safely stable over time. Your doctor will explain what your number means, why follow-up matters, and how monitoring keeps you safe.
This guide is for people with a low platelet count found in outpatient or non-emergency settings. It does not apply to urgent situations such as ICU care, suspected TTP, severe bleeding, or rapidly falling counts.
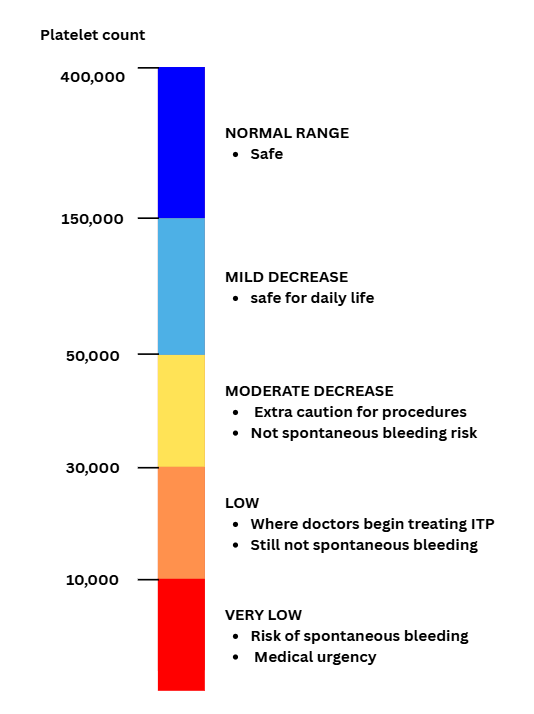
Figure 1. This chart shows platelet levels and what they usually mean for daily life and bleeding risk. Most people with mild decreases are safe and have no symptoms. Spontaneous bleeding is uncommon until platelet counts are very low (usually below 10,000).
First things first
A low platelet count is usually found on routine blood work. Most people with mild thrombocytopenia have no symptoms, and many causes are temporary or reversible.
A single low value often improves on its own. Your doctor will guide whether any follow-up is needed.
What are platelets?
Platelets are tiny cell fragments that help your blood clot. They rush to a site of injury, stick together, and form the first layer of a clot to stop bleeding.
Your body makes platelets in the bone marrow, releases them into the bloodstream, and replaces them continuously.
Most adults have 150,000–400,000 platelets per microliter (150–400 × 10⁹/L).

What is thrombocytopenia?
Thrombocytopenia means your platelet count is lower than the laboratory’s reference range.
How platelets are measured
Most adults have 150,000–400,000 platelets per microliter (150–400 × 10⁹/L).
A value below 150,000 is considered thrombocytopenia in most laboratories.
Your CBC may report platelets using different units:
- “×10⁹/L”
- “K/µL”
Both represent the same quantity. Platelet counts can vary day to day, and mild decreases are often temporary.
Ranges that matter
- mild: 100–150
- moderate: 50–100
- low: 30–50
- very low: <30 (bleeding becomes more likely, especially at very low levels)
Most people with mild thrombocytopenia have no symptoms.
Why it happens (causes)
Temporary causes (most common)
Platelets often return to normal once the trigger improves.
- viral infections
- pregnancy
- alcohol use
- medications (including many common drugs)
Underlying medical conditions
Some health conditions can lower platelets, including:
- autoimmune conditions
- some infections
Liver disease and spleen enlargement (platelet “trapping”)
In liver disease or an enlarged spleen, platelets may become trapped in the spleen, leaving fewer circulating in the bloodstream.
Less common bone marrow causes
These include disorders where the bone marrow does not make enough platelets. These causes almost always affect more than one blood count. When platelets are the only low value, bone marrow problems are much less likely.
Does it cause symptoms?
Many people with thrombocytopenia have no symptoms, especially when the count is mildly or moderately low.
Is it dangerous?
Most cases are not dangerous, especially when platelets are above 50,000.
Bleeding risk depends on how low the count is:
- Below 10,000: the risk of spontaneous bleeding is higher, and this level usually requires urgent treatment or close monitoring.
- 10,000–30,000: bleeding can occur with injuries, certain medications (such as blood thinners), or medical procedures.
- Above 50,000: most daily activities and many medical procedures are safe.
- Around 70,000: epidural or spinal anesthesia is usually considered safe at this level if the platelet count is stable and there are no other bleeding concerns.
- Above 100,000: this level is preferred for neurosurgery or certain eye surgeries.
Your doctor will focus on the pattern over time, the cause, and your overall health, not just the number on one test.
How your doctor evaluates it
Repeat CBC
to confirm the finding and assess trends
Blood smear
to evaluate cell appearance
Viral testing
examples include HIV when clinically appropriate
Medication review
to identify possible causes
Autoimmune testing
when symptoms suggest these conditions
Pregnancy test
when indicated
Bone marrow testing (reserved for)
very low counts, multiple abnormal blood counts, or concern for marrow disease
Most people do not need all of these tests.
How is it treated
Treatment depends on the cause:
- temporary thrombocytopenia → often no treatment
- medication-related → adjusting or stopping the medicine may help
- infection-related → treating the infection may raise the count
- liver or spleen conditions → address the underlying issue
- immune thrombocytopenia (ITP) → may require specific therapy
Many people only need periodic follow-up CBCs.
Daily life and self-care
- avoid unnecessary NSAIDs or aspirin unless your doctor approves
- avoid high-injury-risk activities if your count is very low
- report unusual bruising or bleeding early
- maintain good sleep, nutrition, and activity
- follow your doctor’s follow-up schedule
Most routine daily activities are safe when platelets are above 50,000.
When should I contact my doctor?
Contact your doctor if you have:
- increased bruising
- nosebleeds
- heavy periods
- small red or purple spots on the skin
- bleeding that is slow to stop
Seek urgent care for:
- vomiting blood
- black or tarry stools
- blood in urine
- severe headache
- difficulty breathing
- confusion
What is the usual plan going forward?
Your doctor will:
- monitor your platelet count over time
- repeat CBCs if symptoms develop or counts change
- watch the pattern to see whether the count is stable, rising, or falling
- decide whether any additional tests are needed
Many mild or temporary cases improve once the underlying trigger resolves, and most people with stable, mildly low platelets do well with regular monitoring.
Making sense of it
Platelets are like tiny repair patches that your body sends out whenever a blood vessel needs attention.
When the count is a little low, you still have plenty of patches for everyday life, which is why many people feel well even with thrombocytopenia.
A low platelet count often reflects something temporary or reversible. Your doctor’s job is to make sure the number fits a safe explanation and to watch for changes over time.
Key takeaways
- thrombocytopenia is common and often temporary
- most mild cases cause no symptoms and are found on routine lab tests
- bleeding risk depends on how low the count is, especially below 30,000
- evaluation looks at patterns and causes, not just one number
- monitoring helps keep you safe, and treatment is tailored to the cause
For clinicians: Read our detailed guide on how to communicate about thrombocytopenia to patients.
