- Is there hemolysis?
- Reticulocyte count – increased
- Lactate dehydrogenase (LDH) – may be normal or increased
- Haptoglobin – reduced
- Blood film – spherocytes, agglutination or polychromasia
- Urinalysis/dipstick test positive for blood but urine microscopy negative for red cells – if hemolysis is intravascular, leading to hemoglobinuria.
- Urinary hemosiderin – can be detected approximately 1 week after onset of intravascular hemolysis.
- Is the hemolysis autoimmune?
- A positive direct antiglobulin test (DAT) suggests an immune etiology.
- DAT should include monospecific anti-IgG and anti-C3d.
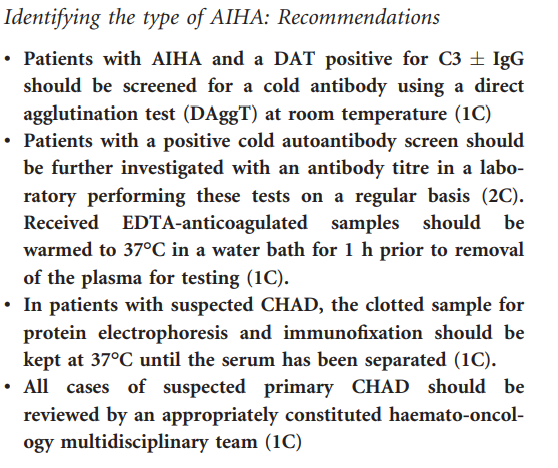
- What is the type of AIHA?
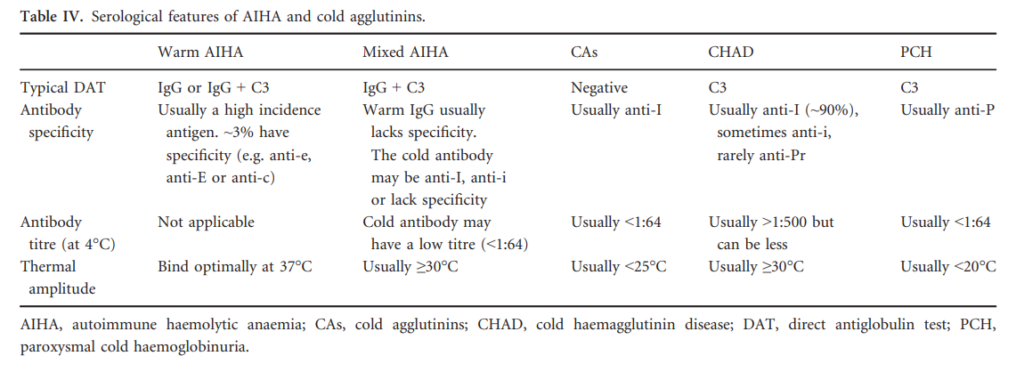
- Warm AIHA
- Caused by autoantibodies (usually IgG) that bind red cells optimally in vitro at 37°C.
- When tested with anti-C3 and anti-IgG reagents, the DAT would be positive for: IgG only (35%), IgG + C3 (56%) or C3 only (9%).
- AIHA can be considered warm when there is a consistent clinical picture and a DAT positive to IgG, C3 or both, when a clinically significant cold reactive antibody has been excluded.
- Cold AIHA (Cold hemagglutinin disease, CHAD):
- Caused by autoantibodies (usually IgM) that bind red cells optimally in vitro at 4°C.
- DAT is usually positive for C3 only, 21–28% are also positive with IgG.
- CHAD can be diagnosed in patients with AIHA and a DAT positive to C3 +/- IgG, with a consistent clinical picture and a high titer cold reactive antibody. The thermal amplitude may be considered as a supportive serological investigation where diagnostic uncertainty exists.
- Warm AIHA
Learn more here.
