The following poll was posted on Twitter Jan 6, 2024.

With over 6,900 votes cast, the most popular choice was transfusion followed by IV iron replacement therapy, but there was a spread across all answers. There were lots of interesting comments (examples shown in graphic), and some healthy back-and-forth!

There is no “right” answer here. Stated another way, there are no clinical trials comparing treatment strategies in this exact situation. But some there are some overarching themes:
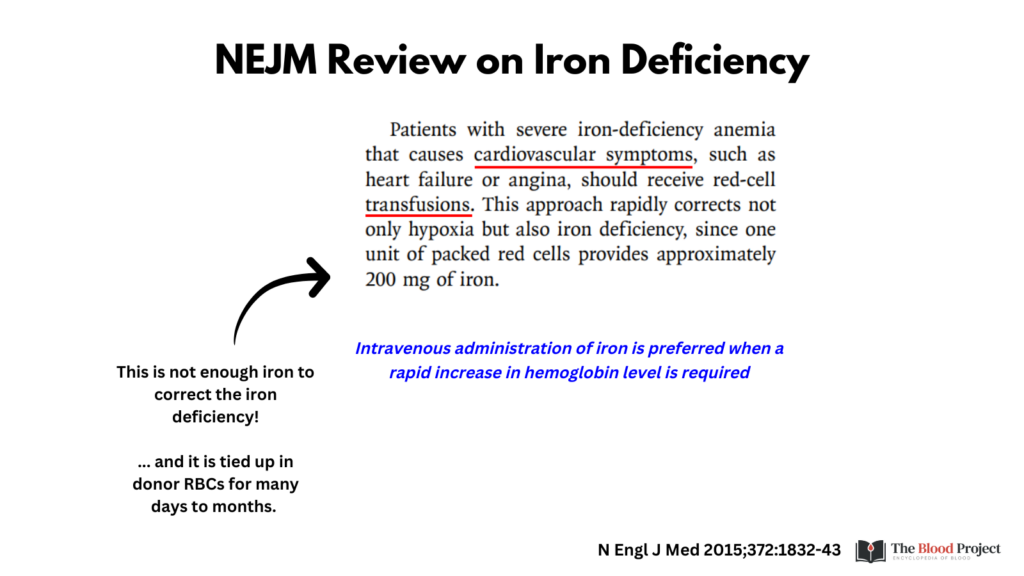
- Transfusion alone may improve symptoms of anemia, but will not fix the problem. A unit of RBCs contains 200-250 mg Fe, hardly enough to replete the patient’s overall deficit. Moreover, the iron is “tied up” in Hb until donor cells die and are processed by the RES.
- Otherwise healthy patients with chronic anemia such as iron deficiency anemia (IDA) are well compensated from a cardiovascular perspective. There is usually time for iron to work!
- IV iron works faster than oral iron and should be considered if it is available.
- Transfusions carry small but definite risks.
One Tweet stated: “Imo people will answer according to their imagined experiences, not the ideal.” How many of us signaled IV iron in the poll, but might be tempted to transfuse in real life?
Let’s look at what the experts say:
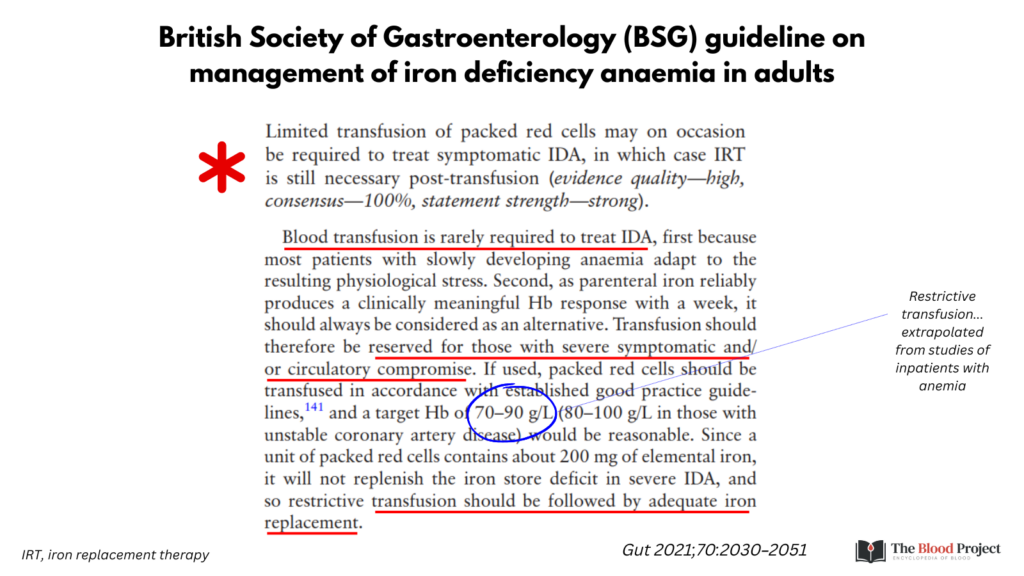
The only clinical practice guideline that provides a recommendation about treating such patients is from the British Society of Gastroenterology (BSG; see graphic below). Based on expert opinion, they recommend limiting transfusion to treat IDA with severe symptoms or circulatory compromise.
The American Red Cross advises treating patients with IDA with iron, but acknowledges that transfusion may be required to minimize symptoms. Without providing any data, they state that transfusion is usually required for Hb < 6 g/dL (assuming the patient is otherwise healthy).

A New Engl J Med review on IDA suggests transfusion in patients with severe IDA that causes cardiovascular symptoms.
AABB guidelines do not address IDA per se, but they endorse a restrictive transfusion threshold (Hb < 7 g/dL) for inpatients who are hemodynamically stable. As mentioned earlier, these data have been extrapolated – rightly or wrongly – to outpatients with chronic anemia.

Choosing Wisely is typically succinct: “Don’t transfusion pRBCs for iron deficiency without hemodynamic instability”.

In summary, this patient would ideally be treated with IV Fe alone.
But what if IV Fe is not available? What if it cannot be scheduled for several days? Or what if, in the spirit of shared decision making, the patient requests a transfusion? So many ifs!
.
