Bottom line
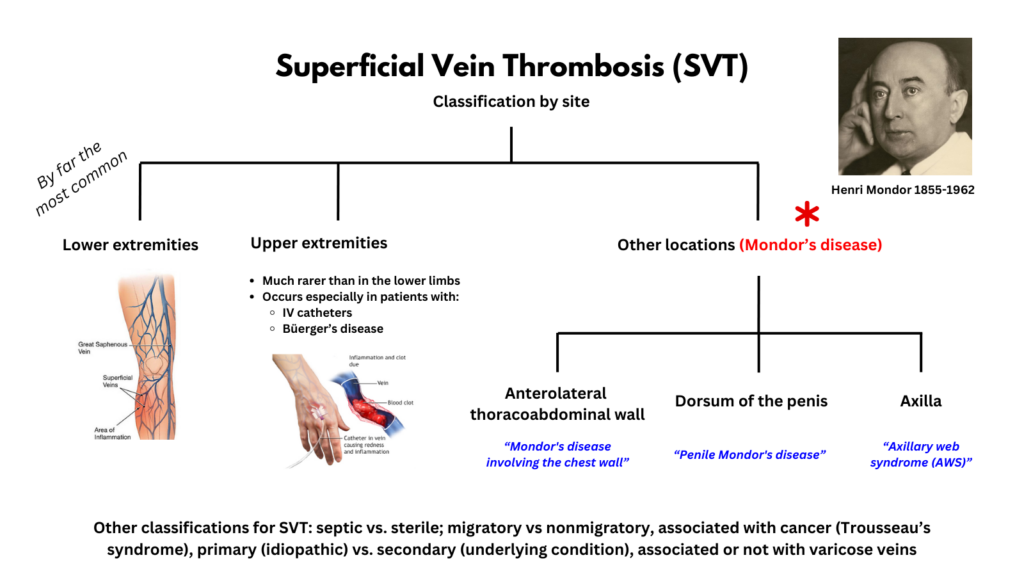
- Mondor’s disease was first described in 1893 in 4 patients with SVT of the thoracoepigastric vein. Over time, the term was coopted to include superficial thrombosis of the superficial dorsal vein of the penis and superficial thrombosis of in veins of the axially region after lymph node dissection. Now it seems that any variant of superficial thrombosis that does not involve the lower or upper extremities is fair game to be termed a variant of Mondor’s. In other words, while Mondor’s disease once referred to superficial thrombus in very specific location (the thoracoepigastric vein), it is now used to describe superficial venous thrombosis located anywhere outside the legs and arms!1
Introduction
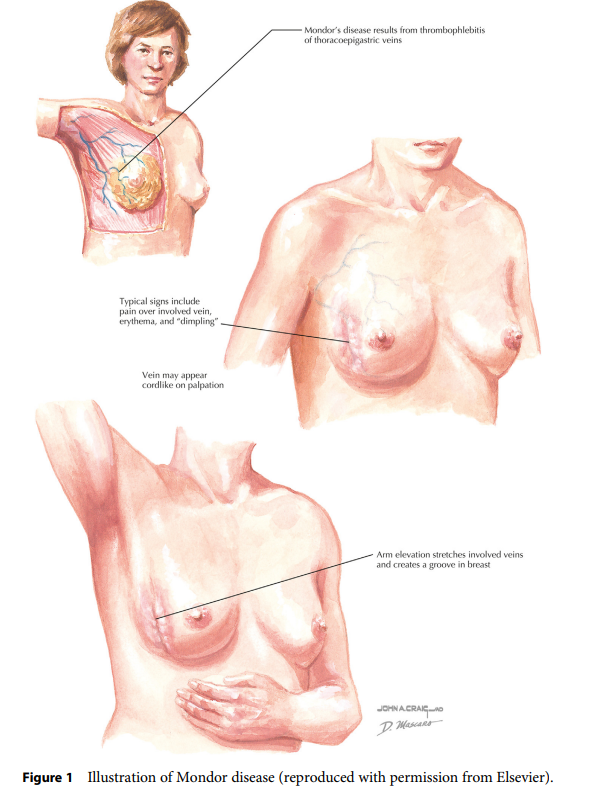
- Mondor’s disease (MD) is a rare, benign, self-limiting form of superficial thrombophlebitis that affects the subcutaneous veins on the anterolateral thoracoabdominal wall, the dorsum and dorsolateral aspects of the penis or the mid-upper arm after axillary surgery, presenting with cord-like indurated lesions on the body surface.2345
- Diagnosis of MD is straightforward and based on physical examination.6
- MD is typically self-limited, resolving in four to eight weeks without any specific treatment.7
Definitions
- According to a consensus statement on superficial vein thrombosis:8
- Superficial vein thrombosis (SVT) is a well-recognized clinical entity characterized by a painful, warm, erythematous, tender, palpable cord-like structure along the course of a superficial vein, usually involving the lower extremities, but potentially affecting any superficial vein in the body.
- SVT is an acute disease where thrombus formation is connected with an inflammatory response of the venous wall.
- The term superficial thrombophlebitis should be discouraged because inflammation and infection are not the primary pathology.
- Mondor’s disease (MD) is a rare, benign, self-limiting form of SVT that affects the subcutaneous veins on the anterolateral thoracoabdominal wall, the dorsum and dorsolateral aspects of the penis or the mid-upper arm after axillary surgery (some authors include other sites in the trunk), presenting with cord-like indurated lesions on the body surface.9101112
- Mondor’s disease is defined by the location of the SVT. Depending on the circumstances it may qualify as:
- Trousseau syndrome, if it is associated with cancer at time of diagnosis.13
- Migratory thrombophlebitis, if there is involvement of one vein group first, then improving and followed by the involvement of other vein groups (occurs in Behcet disease and malignancy [paraneoplastic phenomenon]).
History
- In 1939, Henri Mondor, a French surgeon, described 4 patients exhibiting an SVT of the thoracoepigastric vein and its tributaries.141516
- More about Henri Mondor:
- Born in Saint-Cernin, France in 1885.
- Began his studies in the Faculty of Medicine of Paris in 1903.
- Received his medical doctorate in 1909.
- Began his surgical training under the tutelage of Paul Lecene.
- Authored the book Diagnostic Urgente, which was published in five editions, along with many published articles in various journals.
- Served as Co-editor of the Journal de Chirugie and Presse Medicale.
- Named Professor of Surgical Pathology and Surgery at La Salpetriere in Paris.
- Died in 1962.
- Twenty years later, France issued postage stamps in his honor.
- There is a hospital named after him (Hôpitaux Universitaires Henri Mondor).
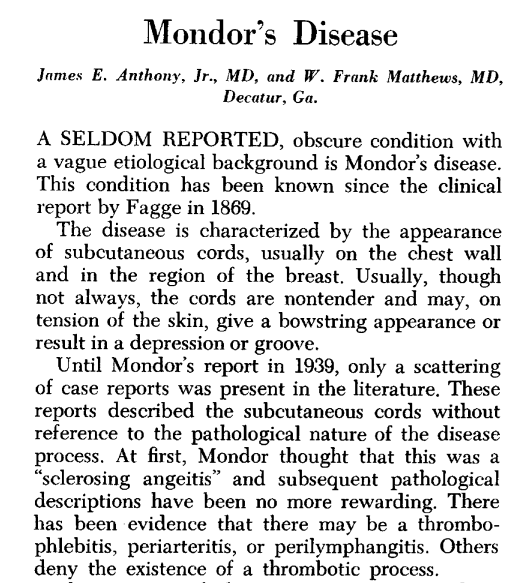
- Mondor was not the first to report the condition, but he provided the most definitive description including the clinical and pathological demonstration of thrombosis.17
- According to Pugh et al:
- “There had been many other descriptions of Mondor’s disease before 1939. However, when Mondor published his article describing the four patients he had seen, he also demonstrated clinically and pathologically the thrombophlebitis of the thoracoepigastric vein and its tributaries. After his first paper became known as the most complete description of the breast lesion, he subsequently wrote two additional papers on the disease.”18

- Subsequently, similar cord-like indurations were reported to occur at other sites, including:19
- Penis (penile Mondor’s disease, PMD):
- Dorsal phlebitis of the penis in the context of generalized phlebitis was first reported by Baun-Falco in 1955.20
- Isolated superficial penile vein thrombosis was first described by Helm and Hodge in 1958.21
- Because thrombosis of the superficial dorsal penile vein resembles superficial venous thrombosis of the chest, a well-known disease described by Mondor in 1939, it is also called penile Mondor’s disease.22
- Axilla (axillary web syndrome, AWS):
- First described and named by Moskovitz in 2001 in a retrospective study of 750 patients with breast cancer undergoing axillary lymph node dissection underwent ALND , 44 (6%) of whom developed postoperative pain and limited range of motion associated with a palpable web of tissue extending from the axilla into the ipsilateral arm. Most cases occurred during the second postoperative week. AWS resolved in all patients within 3 months The authors commented:23
- “The AWS syndrome is analogous to an axillary variant of Mondor’s disease. Mondor’s disease is a superficial thrombophlebitis of thoracoepigastric veins that has been observed infrequently in patients after breast procedures, from local trauma, as an idiopathic variant, and in patients with previously undiagnosed breast cancer. Typical symptoms include the appearance of a palpable, usually painful, subcutaneous cord on the chest wall that has been described as a “string phlebitis”. As in the AWS, symptoms of Mondor’s disease have been reported to resolve spontaneously 2 to 10 weeks after onset. Some investigators have observed histologic characteristics more consistent with thrombosed lymphatics than veins.”
- First described and named by Moskovitz in 2001 in a retrospective study of 750 patients with breast cancer undergoing axillary lymph node dissection underwent ALND , 44 (6%) of whom developed postoperative pain and limited range of motion associated with a palpable web of tissue extending from the axilla into the ipsilateral arm. Most cases occurred during the second postoperative week. AWS resolved in all patients within 3 months The authors commented:23
- Penis (penile Mondor’s disease, PMD):
Classification
- According to anatomical site of the lesion:
- Mondor’s disease involving the chest wall:24
- Superficial vein thrombosis (SVT) involving veins of the anterolateral thoracoabdominal wall.25
- Corresponds to the original Mondor’s disease, as it was described in 1939.
- Physical examination reveals a fibrous painful cord with skin retraction but unlike classical SVT, there is no cutaneous inflammation.
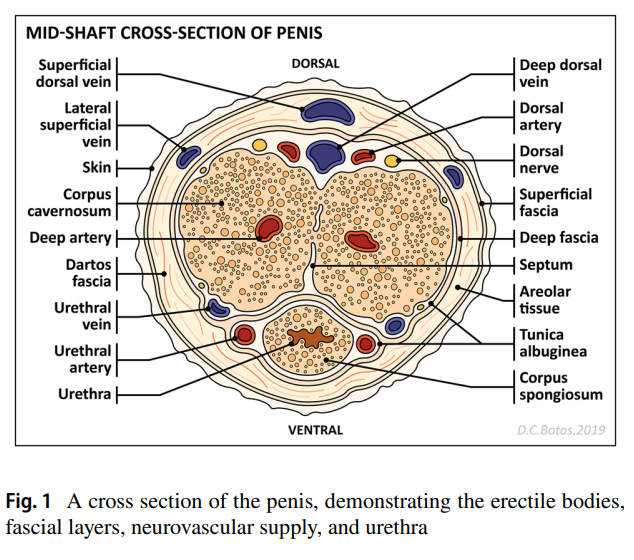
- Penile Mondor’s disease (PMD):26
- SVT involving the superficial dorsal vein of the penis.
- Also known as superficial penile thrombophlebitis
- Physical examination shows a cord-like swelling or thickening on the dorsal side of the penis with a local preputial inflammation without skin retraction.
- Axillary web syndrome (AWS):
- Refers to the development of fibrotic bands or “cords” in the axilla of patients who have undergone axillary lymph node dissection or sentinel node biopsy for breast cancer.27
- Mondor’s disease involving the chest wall:24
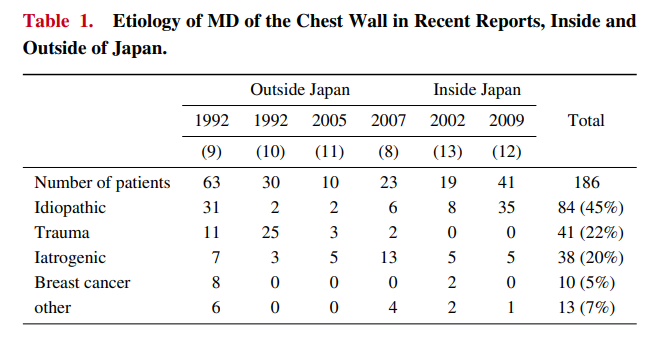
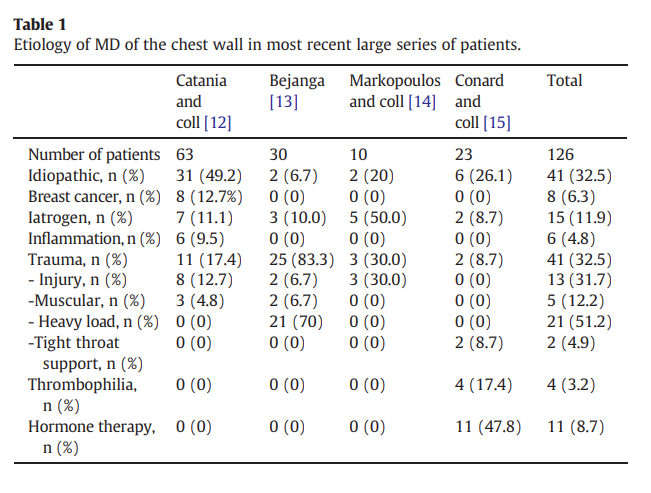
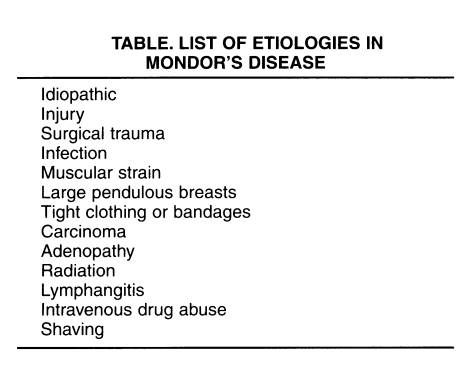
- According to whether or not there is an underlying condition:28:29
- Primary Mondor’s disease (idiopathic):
- 45% of cases
- No underlying disease
- Secondary Mondor’s disease:
- Involves predisposing or underlying factors, the most common causes being:
- Traumatic (22%)
- Iatrogenic (20%)
- Other suspected etiologies include:
- Infection
- Muscular strain
- Large pendulous breasts
- Tight clothing or bandages
- Carcinoma
- Adenopathy
- Radiation
- Lymphangitis
- Intravenous drug abuse
- Shaving
- Involves predisposing or underlying factors, the most common causes being:
- Primary Mondor’s disease (idiopathic):
Epidemiology
- Although Mondor’s disease is rare, it is believed to be more common than reported. Patients may not seek medical care because the disorder is a benign and self-limiting process.
- By 1963, only approximately 200 cases had been reported in the literature.30
- By 2012, approximately 500 cases had been described in the literature.31
- Mondor’s disease involving the chest wall:
- Penile Mondor’s disease:
- Axillary web syndrome (AWS):38
- Typically occurs in those who have undergone axillary lymph node dissection or sentinel node biopsy for breast cancer.
- Can occur after axillary node biopsy for malignant melanomas with an incidence of up to 5%.
- It may also occur in patients undergoing surgical excision of axillary skin lesions, even without removal of axillary lymph nodes.
Anatomy
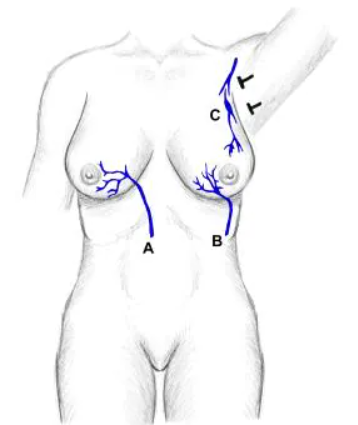
- Mondor’s disease involving the chest wall:
- Typically involves 1 of 3 veins:39
- Lateral thoracic vein:
- The most commonly involved vein.
- Gives rise to the “string-like” cord often described in the upper outer aspect of the breast extending down the anterior axillary line.
- Thoracoepigastric vein
- Superior epigastric vein
- Lateral thoracic vein:
- Typically involves 1 of 3 veins:39
- Penile Mondor’s disease:
- Axillary web syndrome (AWS): Sclerosed veins and lymphatics in the axilla.
Pathogenesis:
- Pathology:44
- Almost all cases of Mondor disease involve thrombophlebitis of the superficial vein, though some cases also involve lymphangitis.45
- In early stages, the venous lumen becomes occluded with fibrin and inflammatory cells. Subsequently, the connective tissue gathering in the vessel forms a hard, cord-like induration. Thereafter, recanalization occurs over several weeks.46
- Mondor’s disease involving the chest wall:47
- 45% of cases are idiopathic.
- 20% of cases are iatrogenic, including:
- Chest surgical operation
- Radiation
- Hormone therapy
- 22% of cases are traumatic (including excessive physical activity and a tight bra).
- 5% of cases are related to breast cancer.
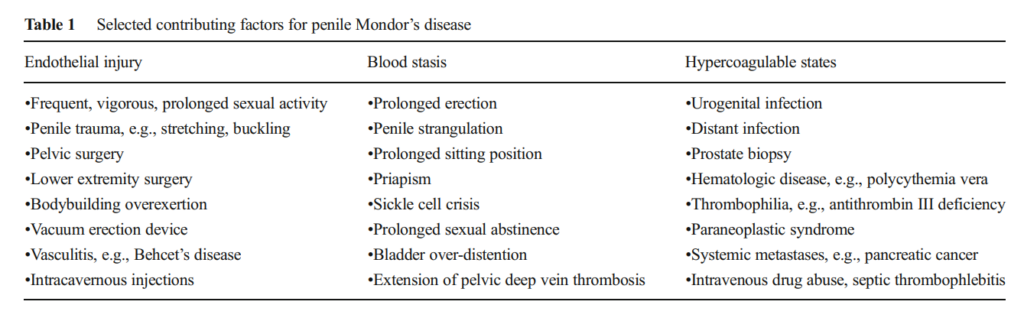
- Penile Mondor’s disease:48
- Risk factors according to Virchow’s triad:
- Vessel wall damage due to:
- Vigorous sexual activity
- Vacuum erection device
- Penile trauma
- Blood stasis, such as:
- Prolonged erection (including with the use of a PDE5 inhibitor)
- Prolonged sitting position
- Bladder overdistension
- Priapism
- Compression of pelvic vasculature by belts
- Hypercoagulation, such as:
- Urogenital infection
- Prostate biopsy
- Hematological disease
- Vessel wall damage due to:
- The most common triggering factor is prolonged and intensive sexual intercourse, with most patients presenting within 1–7 days of such activity. The micro-trauma associated with such sexual encounters is sufficient to trigger clot formation.49
- Other triggering factors include:50
- Trauma from stretching or buckling forces
- Vacuum erection device use
- Intracavernosal injections
- Pelvic or lower extremity surgery such as inguinal hernia and varicose vein surgery
- Overexertion while bodybuilding
- Vasculitides such Bechet’s
- Pathologic analysis of thrombectomy specimens in PMD reveals:51
- Vein obliteration
- Endothelial cell enlargement
- Blood vessel wall thickening with connective tissue proliferation
- Mixed lymphocytic and histiocytic perivascular infiltrate
- Occasional venous and arterial sclerosis
- Risk factors according to Virchow’s triad:
- Axillary web syndrome (AWS):
- Disease increases with the complexity of surgery:52
- 6-20% incidence with a sentinel lymph node biopsy
- 72% with complete axillary dissection
- The risk factors for AWS include:53
- Advanced-stage breast cancer
- Extensive surgery (mastectomy or axillary lymph node dissection)
- Young age
- Low body mass index
- Hypertension
- African-American ethnicity
- Healing complications
- Men who play squash
- The “cords” in AWS represent sclerosed veins and lymphatics with surrounding fibrosis.54
- Disease increases with the complexity of surgery:52
Clinical presentation
- General:
- Typically present with cord-like lesion.
- Other symptoms may include:
- Pain
- Tightness
- Erythematous skin change
- Fever
- Discomfort during movement.
- In addition, some patients experience anxiety because of its unfamiliar appearance, especially when the lesion occurs on the penis.55
- When MD occurs secondary to an underlying cause, such as giant-cell arteritis or other vasculitis, concomitant symptoms, including a high-grade fever or malaise, may be present.56
- Mondor’s disease involving the chest wall:
- Typically unilateral in the left or right breast and/or upper abdominal region. 3% of cases occur bilaterally.57
- Clinical findings are usually found in the mammary area, radiating from the region of the areola towards the axilla, epigastrium, or subcostal margin.
- Often diagnosed in women at breast clinic.58
- Typical findings:
- Palpable subcutaneous cord-like indurations beneath the skin.59
- Indurations commonly appear longitudinally on the anterolateral thoracoabdominal wall because of its rich, vertically oriented superficial vein network.60
- The overlying skin is freely mobile
- The skin shows limited or no inflammatory changes/signs.6162
- Although the lesions are typically asymptomatic, some patients experience pain or discomfort, especially on palpation or during twisting and stretching movements.63
- Other manifestations may include:64
- Tenderness
- Tension sensation
- Erythema
- Ecchymosis
- Pruritus
- Arthralgia
- Rarely fever
- Penile Mondor’s disease:6566
- Often diagnosed at urology clinics.
- Tends to develop in men between 20 and 40 years old typically in 24 hours following prolonged sexual intercourse. It probably develops secondarily to vascular endothelial trauma. The patients present with a palpable lesion as a thick cord occurring 24 to 48 hours after a prolonged sexual intercourse.
- Patients with the disease consult a physician usually because of fear of a malignancy, venereal disease or possibility of impotence.67
- Patient presents with induration on the dorsal and dorsolateral aspects of the penis.6869
- Other manifestations may include:
- Episodic or continuous pain and throbbing.
- Pain typically exacerbated during erection
- Erythema and edema on the penile skin
- Irritative voiding symptoms
- Cohort of 25 patients with penile MD
- No patient reported any pain.
- In 2 cases, the disease was noted in relation to erectile dysfunction.
- No signs of acute inflammation could be detected in any patient.
- Thrombosis occurred at the dorsal penis shaft in all patients.
- Thrombosis occurred:
- After prolonged sexual intercourse in 1 patient
- after application of a vacuum erection device in one patient
- For 20 patients idiopathic penile vein thrombosis was diagnosed
- In 23 patients, the findings showed significant regression after a few days of conservative therapy which consisted of a dressing with heparin ointment and oral application of an antiphlogistic (indomethacin).
- Even after 4 weeks of conservative treatment, idiopathic superficial penile vein thrombosis persisted in 2 patients who had not shown any signs of resolution Therefore, they underwent surgery.
- Axillary web syndrome (AWS):
- Non erythematous induration arises at the distal parts of the axially surgical scar forming fibrotic bands or “cords” in the axilla and extending for any length from the mid-upper arm to the base of the thumb.70
- Other manifestations may include:
- Pain in the axilla that can radiate down the arm.
- Tender fibrotic bands that become more prominent, taut and painful during shoulder abduction.72

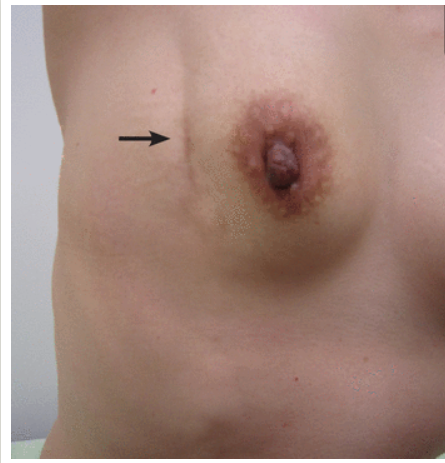
A 43-year-old woman presented to the outpatient breast clinic with a 2-week history of pain and skin tightness over the right breast. She had no history of breast-related surgeries or trauma and was not on any regular medication. Physical examination revealed a subcutaneous cord-like, fibrous, tender lesion running diagonally from the upper outer quadrant of the right breast to the right flank, causing skin retraction and a groove over the outer half of the right breast when the right arm was stretched upward Doppler ultrasonography revealed a noncompressible, dilated, subcutaneous vein without flow, supporting the diagnosis of Mondor disease of the breast, which commonly presents superficially in the lateral part of the breast. Cleve Clin J Med. 2022 Jul 1;89(7):371-372 
Male patient presented with dull aching pain below right nipple. Physical examination revealed a tender subcutaneous cord that began below the right anterior axillary fold and continued toward the right hypochondrium. Lifting of the right arm above the head accentuated the appearance of the cord. Doppler ultrasonography revealed a noncompressible right thoracoepigastric vein containing echogenic material, a finding that was consistent with superficial venous thrombosis N Engl J Med. 2017 Jun 8;376(23):e47. 
A 30-year-old man presented with recurrent, painful swelling of the penis. He credibly denied self-manipulation or the
use of sex toys. Clinical and duplex ultrasonographic examination revealed thrombosis of the dorsal penile vein. Thrombosis at this site is designated as penile Mondor’s disease. Dtsch Arztebl Int. 2018 Jun 29;115(26):452.Diagnosis
- Diagnosis is usually based on history and physical examination alone and can be confirmed with ultrasound if necessary.
- Physical examination typically reveals:73
- A cord-like lesion a few centimeters in length readily observed upon inspection.
- A hard induration can be palpated beneath the skin.
- Skin retraction when the inflammation of the tissue around the affected vein is severe
- Owing to its association with breast cancer, a thorough breast evaluation including diagnostic imaging is recommended.74
Treatment
- General principles:
- Typically self-limited with resolution within 4–8 weeks of initial presentation.
- Treatment is conservative and symptomatic.
- Anticoagulants are not indicated.
- Surgical intervention is rarely indicated.
- Prophylactic antibiotics are not necessary.
- Mondor’s disease involving the chest wall:75
- Local application of heat
- Rest of the arm
- Breast support
- Conventional analgesics, for example nonsteroidal anti-inflammatory drugs.
- Penile Mondor’s disease: efn_note]PMID 25530373[/efn_note]
- Some authors recommend that patients abstain from sexual intercourse until the symptoms resolve, though no evidence this is helpful.
- Conventional analgesics, for example nonsteroidal anti-inflammatory drugs.
- In case of acute pain, a local anesthetic (0.5% bupivacaine hydrochloride) may be injected subcutaneously in the in the region surrounding the affected vein.
- Heparin ointment has been recommended by some authors.
- Vein stripping may be necessary for severe, persistent cases of Mondor’s disease.
- Eliminate risk factors to help prevent recurrent episodes.76
- Axillary web syndrome (AWS):
- Physical therapy
- Range of motion exercises
- Conventional analgesics, for example nonsteroidal anti-inflammatory drugs.
- Manual axial distraction77
Prognosis
- Benign, self-limited disease that resolves spontaneously in four to eight weeks.78