Introduction
- ITP is an acquired immune-mediated disorder associated with a decreased platelet count and may present with bleeding or bruising.
- ITP has several clinical manifestations beyond bleeding, including:
- Fatigue
- Fear of bleeding
- Anxiety or depression
- Headache
- Reduced work productivity
- Paradoxical increased risk of venous thromboembolism
- About 50% of patients with ITP report fatigue as the top symptom they would like to have resolved.1
- Relevant factors that may contribute to fatigue in ITP include sleep disturbances, pre-morbid lack of activity or psychological symptoms, work and career responsibilities, illness beliefs, perceived stress, and mood.2
- To date, the cause of fatigue in patients with ITP is not well understood, but may relate to low grade underlying inflammation. Fatigue is common in other autoimmune disorders.
- Challenges regarding an approach to fatigue in patients with ITP:
- There are many other causes of fatigue.
- Even if fatigue is causally related to ITP there are limited treatment strategies:3
- “Many clinicians acknowledge that improving quality of life, including fatigue, is an important treatment goal for patients with ITP. An intuitive approach to achieve this is to treat the ITP with any of the known ITP-specific treatment options. However, these treatments may also cause side effects and adverse events and may actually increase rather than reduce fatigue.”
- To date, there is no convincing evidence of a beneficial effect on fatigue for any of the existing ITP treatments.
Expert Opinion
- Cooper and Ghanima, 2019: “Irrespective of bleeding problems, patients with ITP often report fatigue and impaired health-related quality of life”.
- Lambert and Gernsheimer, 2017: No mention of fatigue as primary manifestation of ITP, only as an effect of treatment.
- Kelton et al 2018: No mention of fatigue.
- UptoDate:
- “Patients can also experience fatigue and decreased quality of life.”
- “Fatigue is a common symptom among patients with ITP. It often correlates with thrombocytopenia but can occur even when the platelet count is only mildly reduced.”
- “The causes of fatigue in ITP are not well understood. Some experts have suggested that contributing factors may include associated conditions and comorbidities (e.g., systemic lupus erythematosus [SLE], hypothyroidism), activity restrictions, adverse effects of medical therapies (e.g., sleep disturbance from glucocorticoids), older age, higher stress level, autonomic dysfunction, and/or adverse effects caused by proinflammatory cytokines.”
Primary Data
- Sarpatwari et al, 2010:
- ITP Support Association conducted a questionnaire-based survey to identify health-related lifestyle concerns among adults and children with primary ITP in the United Kingdom.
- 790 (44.7%) completed surveys were received from 696 (88.1%) adults and 94 (11.9%) children with primary ITP.
- 12.5% of all patients with primary ITP reported ‘always’ or ‘often’ missing work or school due to fatigue. These absences were not significantly associated with disease severity.
- Newton et al, 2011:
- Cross-sectional survey of 1871 members of the UK ITP Support Association and 93 patients enrolled in the Oklahoma (US) ITP Registry.
- 585 (31%) in the UK ITP Support Association 68 (73%) in the Oklahoma (US) ITP Registry responded to questions about their ITP and with validated symptom assessment scales for fatigue, daytime sleepiness, and orthostatic symptoms.
- Prevalence of fatigue among both UK (39%) and US (22%) patients was significantly greater than expected compared with the 2.5% expected in normal subjects (P<0.0001 and P<0.0001 respectively).
- Fatigue was not associated with age, gender, duration of ITP, or splenectomy status.
- Multivariate analysis of the combined cohorts was stratified for the presence or absence of bleeding symptoms.
- Among 107 patients with bleeding symptoms, fatigue was independently associated with a platelet count <100000/μL and female gender.
- Among 491 patients without bleeding symptoms, fatigue was independently associated with a platelet count <30000/μL, presence of other medical conditions, daytime sleepiness, and orthostatic symptoms.
- Conclusions: Fatigue is a common symptom among patients with ITP.
- Tsukune and Komatsu, 2016:
- Multi-center, questionnaire-based, cross-sectional study.
- Questionnaires from 204 hematologists and 213 patients were collected.
- Fatigue was most frequently experienced by patients (44.6%).
- Patients also experienced psychological symptoms (feeling of anxiety or depressive mood: 29.1%, labyrinthitis: 23.5%).
- QOL was impaired in 34.3% of patients.
- Conclusions: A substantial gap which exists between hematologists and their patients highlights a need for better understanding of potential conflicts for establishing effective strategies for ITP management.
- Grace et al, 2020:
- Observational cohort of 120 children and adolescents receiving second-line therapies for ITP.
- Assessed reports of fatigue using the Hockenberry Fatigue Scale.
- Children and adolescents with ITP reported a similarly high level of fatigue with 54% (29/54) of children and 62% (26/42) of adolescents reporting moderate-to-severe fatigue.
- There was no correlation between fatigue and age or gender.
- Adolescents with newly diagnosed and persistent ITP had higher mean fatigue scores than those with chronic ITP (P = 0.03).
- Fatigue significantly improved in children and adolescents by 1 month after starting second-line treatments, and this improvement continued to be present at 12 months after starting treatment.
- Fatigue scores did not correlate with bleeding symptoms, platelet count, or platelet response to treatment.
- Conclusions: Fatigue is common in children and adolescents with ITP and may benefit from ITP-directed treatment even in the absence of bleeding symptoms.
- Cooper et al, 2021:
- ITP World Impact Survey (I-WISh) study.
- Cross-sectional survey designed to establish the multifaceted impact of ITP on patients’ lives.
- 1507 patients and 472 physicians from 13 countries.
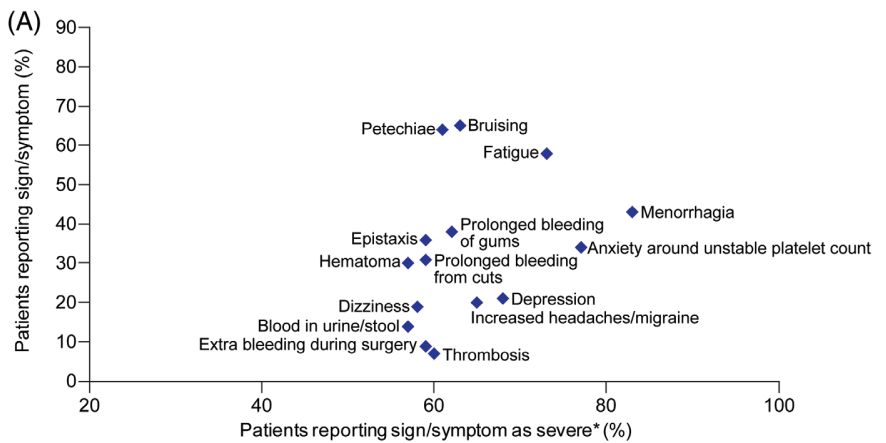
- Patients rated fatigue among the most frequent, severe symptom associated with ITP at diagnosis (58% most frequent; 73% most severe), although physicians assigned it lower priority (30%).
- Fatigue was one of the few symptoms persisting at survey completion (50% and 65%, respectively) and was the top symptom patients wanted resolved (46%) (along with bleeding and unstable platelet counts).
- Conclusions: “Physicians believed fatigue would decrease as platelet count increased, and thus that fatigue was intrinsically related to disease activity. However, fatigue persisted, despite amelioration of other components of ITP between diagnosis and survey completion, suggesting that increasing platelet count and reducing bleeding is not sufficient to abrogate fatigue. The best approach to treating fatigue remains unresolved but, if present, attempts at amelioration should certainly be made. Among many options, raising platelet count (ideally without using steroids), antidepressants and/or anti-inflammatories could be considered. Clinical trials in this area are needed.”

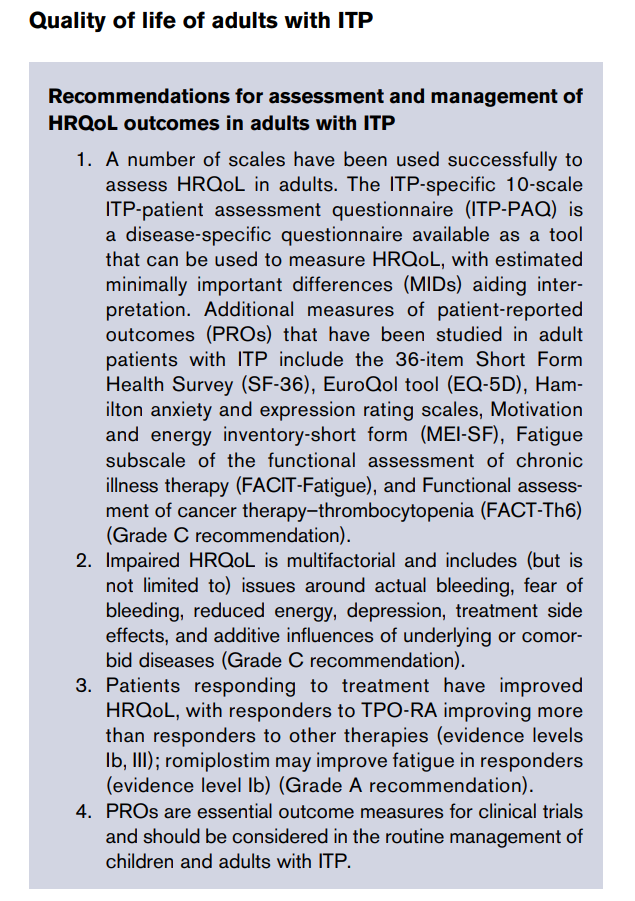
Clinical practice guidelines
- 2019 American Society of Hematology guidelines for immune thrombocytopenia
- “Fatigue is common and reported in 22% to 45% of patients with ITP.”
- “Reported studies show that the effect of treatment on HRQoL and fatigue may vary by treatment, but this area requires further study.”
- 2019 Updated international consensus report on the investigation and management of primary immune thrombocytopenia.4
- Fatigue may be part of the ITP syndrome
- ITP leads to impaired HRQoL across emotional, functional, reproductive, and health domains, and it impacts daily living, in turn affecting mental health
- The most difficult ITP symptom to treat is severe fatigue, reported in 39% to 59% of adult patients with ITP.
- Treatment should always be tailored to the patient, because many factors contribute to treatment decisions, yet it is underrecognized by health care practitioners.
- Platelet counts remain a focus for health care practitioners, whereas fatigue and mental health aspects are the major concerns of patients.
- Impacting management decisions are the extent of bleeding, age, comorbidities predisposing to bleeding, complications of specific therapies, activity and lifestyle, fatigue (see “Quality of life of adults with ITP”), tolerance of side effects, need for interventions with a bleeding risk, accessibility of care, patient expectations, patient worry or anxiety, and patient need for non-ITP medications that may create a bleeding risk.
- Patients’ complaints of fatigue should be respected if not offset by increased toxicity of treatment.
- Responders to romiplostim and standard of care showed an improvement in fatigue above MIDs
- Improvements with etrombopag were significantly associated with eltrombopag-mediated increases in platelet count and decreases in bleeding (World Health Organization scale).
Impact of ITP Treatments on Fatigue
- Medical therapy may influence fatigue, either negatively through toxicity, or positively through disease control.5
- Splenectomy: little data on the impact on fatigue.
- Corticosteroids:
- Multiple side effects that could contribute to fatigue, including sleep disturbance, a range of psychiatric reactions, fluid retention, acne, muscle weakness, proximal myopathy and susceptibility to infection.
- Fatigue has been shown to be associated with steroid treatment.
- Rituximab:
- In a randomized control trial (RCT) of first line rituximab versus rituximab and dexamethasone for primary ITP, fatigue was the most frequently reported adverse event (c. 40%) and was not significantly more common with the addition of steroids.6
- In a placebo-controlled RCT of patients with primary ITP, 22% (7/32) complained of fatigue after receiving rituximab compared with 8% (2/26) receiving placebo, although the difference was not tested for significance.7
- Thrombopoietin receptor agonists:
- In trials of romiplostim and eltrombopag, fatigue was not reported as an adverse event more frequently than in patients receiving placebo.
- Despite a reduction in bleeding events and an overall improvement in HRQoL with romiplostim and eltrombopag, neither treatment was able to show a consistent and clinically significant improvement in fatigue.
