Definitions:
- Bariatric surgery = weight loss surgery, includes:
- Adjustable gastric band (lap-band):
- How it works: A silicone band is placed around the upper part of the stomach to create a small pouch. The tightness of the band can be adjusted by adding or removing saline through a port under the skin.
- Benefits: Less invasive and reversible, the size of the stomach opening can be adjusted.
- Risks: Less weight loss compared to other methods, risk of band slipping or eroding, and potential need for reoperation.
- Gastric sleeve (sleeve gastrectomy):
- How it works: Around 80% of the stomach is removed, leaving a tube-like “sleeve.” The smaller stomach size limits food intake and reduces hunger by lowering ghrelin hormone production.
- Benefits: Less invasive than gastric bypass, effective long-term weight loss, and no intestinal bypass, so fewer nutrient absorption issues.
- Risks: Permanent removal of part of the stomach, risk of acid reflux.
- Gastric bypass (Roux-en-Y gastric bypass):
- How it works: This procedure involves creating a small pouch at the top of the stomach and connecting it directly to the small intestine, bypassing most of the stomach and part of the intestines.
- Benefits: Results in significant weight loss by reducing the amount of food the stomach can hold and decreasing nutrient absorption.
- Risks: Higher risk of vitamin and mineral deficiencies due to bypassed intestines.
- Others (less common):
- Biliopancreatic diversion with duodenal switch (BPD/DS) – combines a sleeve gastrectomy with an intestinal bypass.
- Intragastric Balloon – A balloon is inserted into the stomach via endoscopy and then inflated. This reduces the stomach’s volume, limiting the amount of food that can be consumed.
- Adjustable gastric band (lap-band):
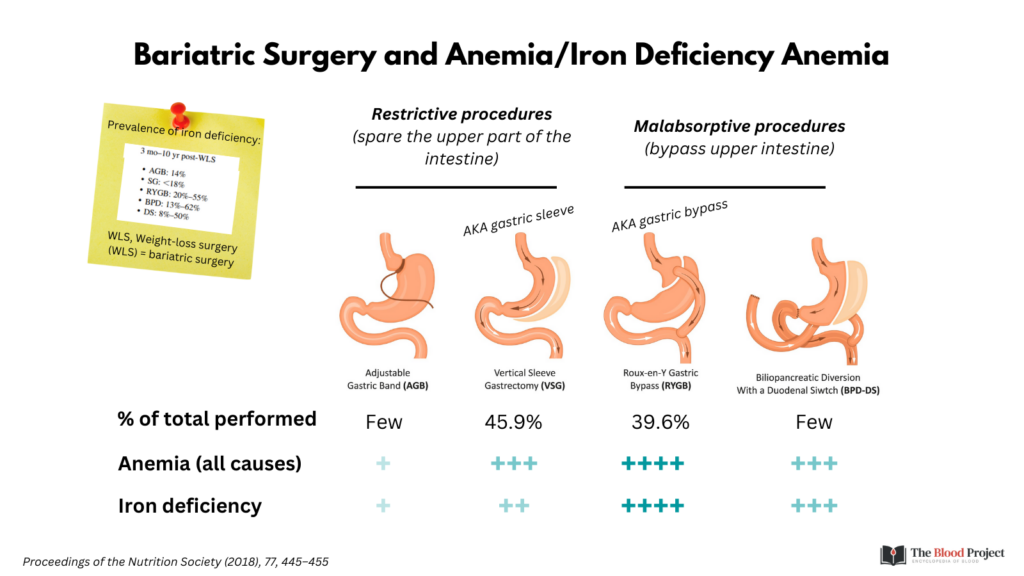
Prevalence of iron deficiency (ID) and iron deficiency anemia (IDA):
- Pre-procedure: 10-15% with IDA, up to 30% with ID
- Post-procedure: Numbers all over the place because of differences in study design, procedure, dietary guidance and other factors. Graphic below shows data from McMaster cohort.
- The following themes emerge:
- Highest prevalence of ID/IDA is with gastric bypass (RYGB).
- Prevalence increases with time post procedure.
- ID/IDA may occur despite Fe supplementation.


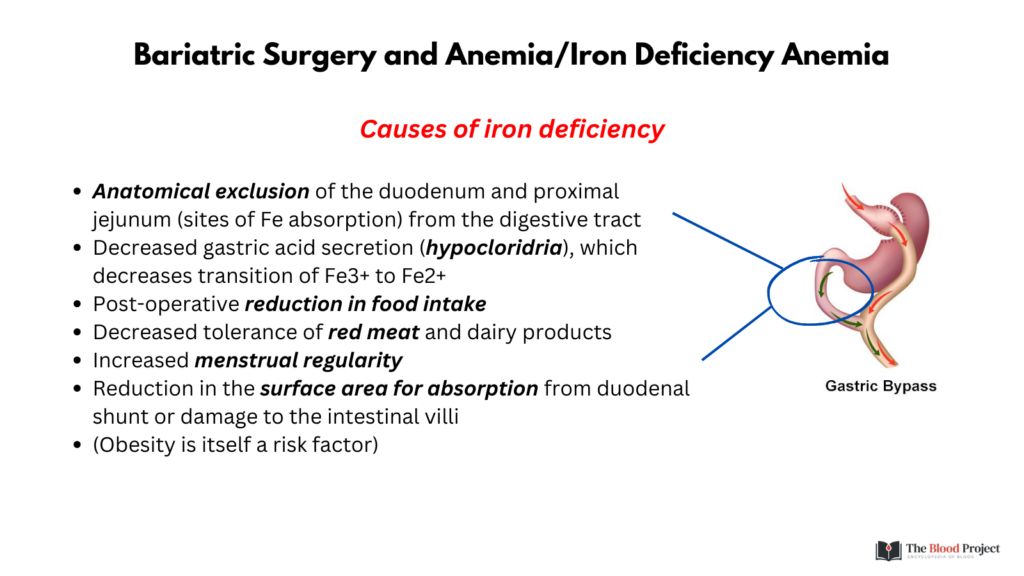
Causes of iron deficiency in bariatric patient:
- Bypass of duodenum (site of Fe absorption)
- Reduced stomach acid
- Reduced food intake/tolerance of red meat
- Increased menstrual regularity
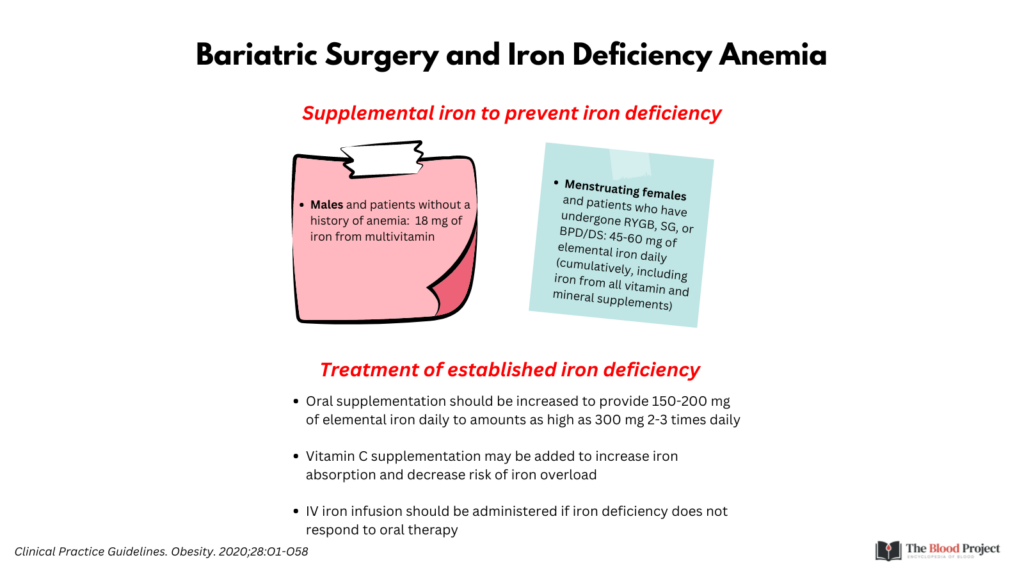
Clinical guideline recommendations:
- Prevention of ID/IDA: 18-60 mg elemental Fe per day
- Treatment of ID/IDA:
- 150-200 mg elemental iron/day
- IV iron infusion should be administered if iron deficiency does not respond to oral therapy
References:
