For larger image, click here.
Overview
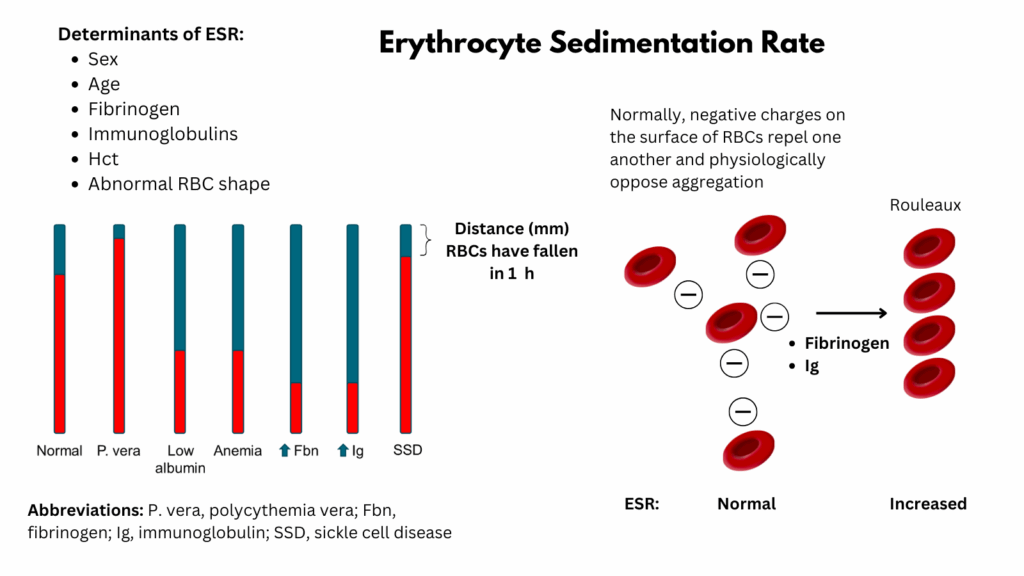
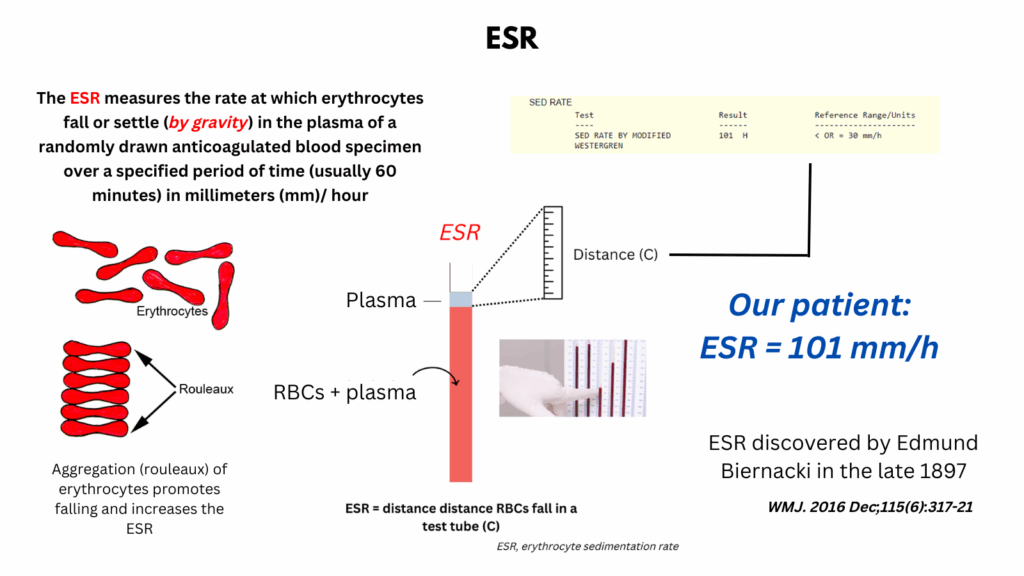
The erythrocyte sedimentation rate (ESR) is a nonspecific laboratory test that measures the rate at which erythrocytes settle in a vertical tube over one hour. An elevated ESR indicates the presence of elevated fibrinogen (acute-phase reactant seen in inflammation) or elevated immunoglobulins (seen in multiple myeloma), which promote red blood cell aggregation, causing them to sediment more rapidly.
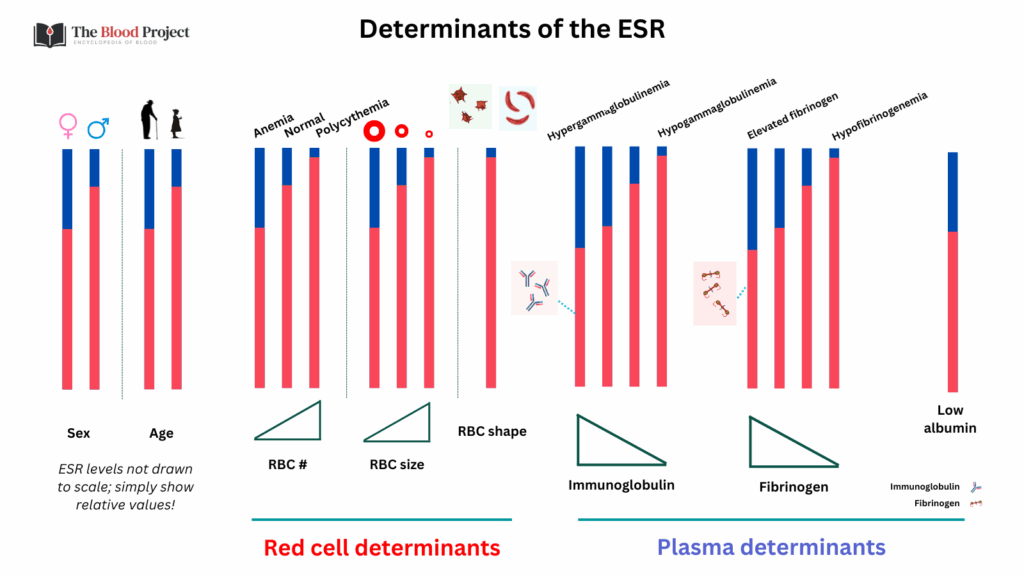
ESR is influenced by multiple factors, including age, sex, anemia, pregnancy, and certain metabolic and lifestyle factors such as obesity, smoking, and physical activity. It is higher in females and increases with age. While ESR is commonly used to support the diagnosis and monitoring of inflammatory, infectious, and neoplastic conditions, it lacks specificity and should not be used in isolation to diagnose any particular disease. Markedly elevated ESR values are most strongly associated with serious underlying conditions such as infection, autoimmune disease, or malignancy.
The test is most clinically useful in the diagnosis and monitoring of specific conditions such as temporal arteritis, polymyalgia rheumatica, and some rheumatologic diseases, as well as in tracking disease activity or response to therapy. However, normal or mildly elevated ESR values do not exclude significant pathology, and abnormal results should always be interpreted in the context of the clinical scenario.
What is it?
- The ESR is a simple, nonspecific blood test that measures how quickly red blood cells (RBCs) settle at the bottom of a vertical tube of anticoagulated blood over 1 hour.
How is it measured?
- A blood sample is placed in a Westergren tube (or Wintrobe tube).
- After 1 hour, the distance (in mm) that RBCs have fallen is measured.
- Normal values:
- Men: 0–15 mm/hr
- Women: 0–20 mm/hr
- (Values increase slightly with age and in pregnancy)
Mechanisms
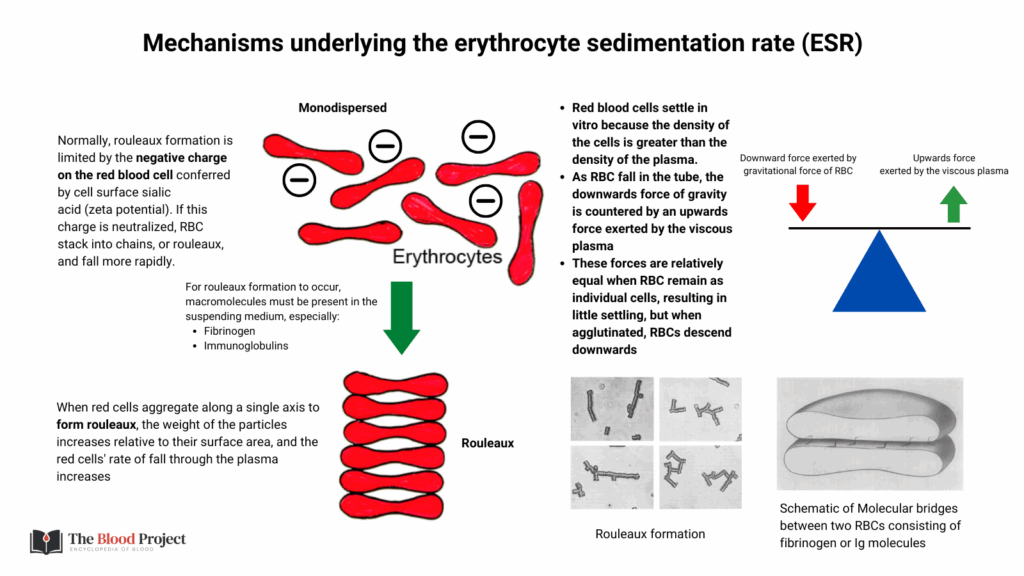
- Plasma proteins:
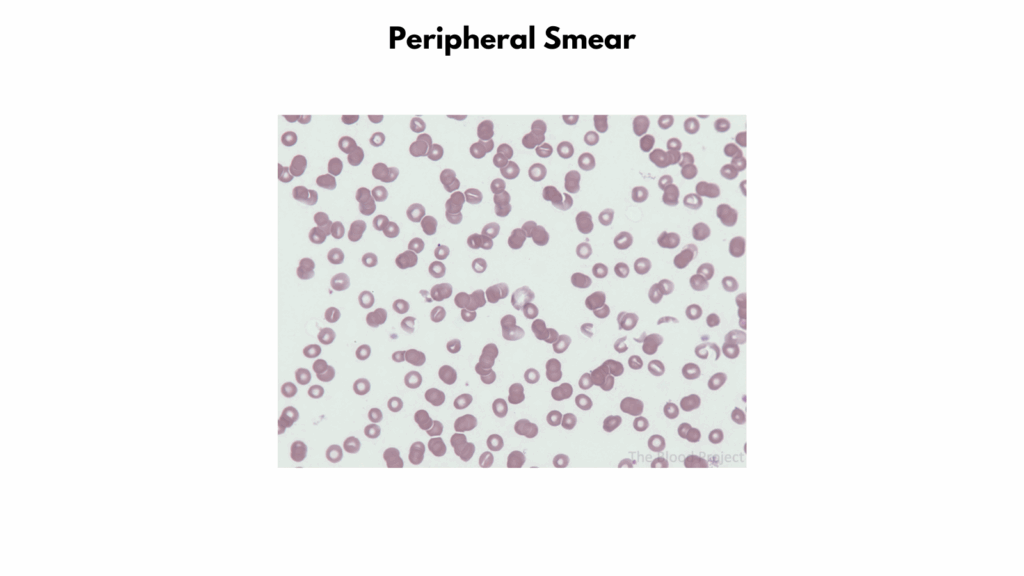
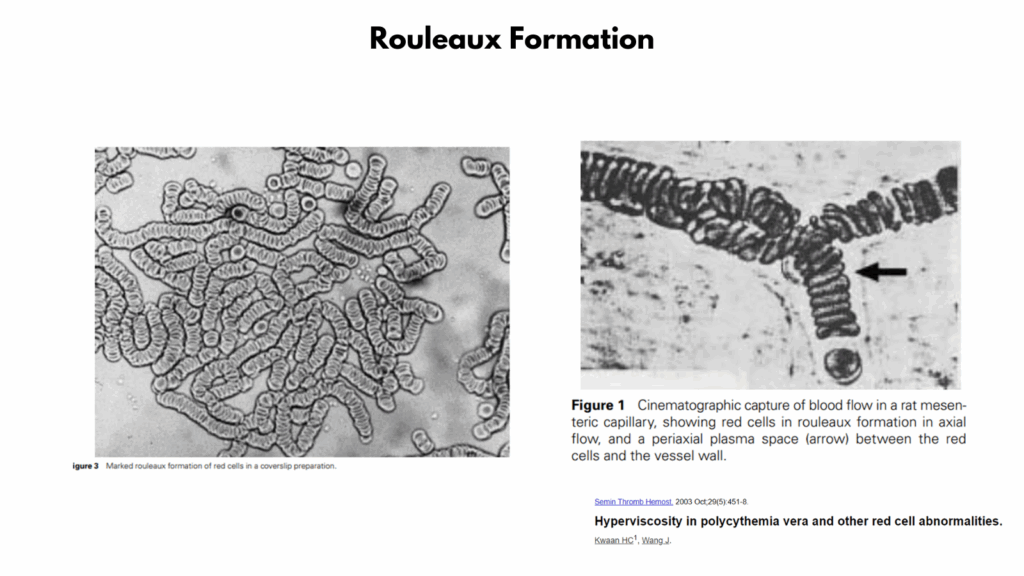
- ESR is increased when red blood cells (RBCs) aggregate into stacks called rouleaux. Normally, RBCs repel each other due to their negative surface charge (zeta potential). Certain plasma proteins reduce this repulsion, allowing stacking and faster sedimentation, including:
- Fibrinogen:
- Fibrinogen is a large, positively charged protein.
- It neutralizes the RBC surface charge, decreasing zeta potential.
- This promotes rouleaux formation, which sediment faster due to increased mass and density.
- Fibrinogen levels rise in inflammation, infection, trauma, and malignancy.
- Immunoglobulins (e.g. IgM, IgG):
- Elevated levels of immunoglobulins (especially IgM, due to its pentameric structure) can also bridge RBCs together.
- They act as molecular crosslinkers between negatively charged RBCs.
- Seen in conditions like:
- Multiple myeloma (IgG, IgA)
- Waldenström macroglobulinemia (IgM)
- Chronic inflammatory states
- Fibrinogen:
- ESR is decreased when plasma viscosity is high. In very high concentrations, especially monoclonal IgM (e.g., Waldenström macroglobulinemia), the resulting hyperviscosity may actually slow down red cell settling, reducing the ESR despite rouleaux-promoting properties.
- ESR is increased when red blood cells (RBCs) aggregate into stacks called rouleaux. Normally, RBCs repel each other due to their negative surface charge (zeta potential). Certain plasma proteins reduce this repulsion, allowing stacking and faster sedimentation, including:
- RBC deformability:
- When RBCs are stiff or rigid, they:
- Do not form rouleaux easily
- Settle more slowly in plasma
- Result in a lower ESR than expected, even in the presence of inflammation
- This may be seen in sickle cell disease, hereditary spherocytosis and thalassemia
- When RBCs are stiff or rigid, they:
- RBC shape:
- Abnormally shaped RBCs interfere with rouleaux formation.
- ↓ ESR in:
- Sickle cell disease
- Spherocytosis
- Elliptocytosis
- Thalassemia (due to microcytosis and poikilocytosis)
- RBC size:
- Microcytic cells (e.g., in iron deficiency) sediment more slowly → ↓ ESR
- Macrocytic cells (e.g., in megaloblastic anemia) may sediment faster → ↑ ESR
- Hematocrit:
- Lower hematocrit
- = less viscous blood
- Fewer RBCs in the column = less crowding and less resistance to sedimentation.
- This allows RBCs to fall more rapidly, even if no inflammation is present.
- Also, in anemia, a higher ratio of plasma proteins to RBCs increases the effect of rouleaux-promoting proteins, which neutralize this repulsion. Lastly, with fewer RBCs, plasma proteins like fibrinogen and immunoglobulins have more space and time to act.
- Higher hematocrit (i.e., polycythemia)
- Increased hematocrit = crowding
- When there are too many RBCs (as in polycythemia vera or relative polycythemia), the cells become tightly packed in the blood column.
- This hinders the formation of rouleaux (RBC stacks), which are needed for rapid sedimentation.
- Polycythemia increases blood viscosity, which:
- Slows down sedimentation
- Prevents RBCs from moving freely through the plasma to settle
- There is less plasma relative to red cells, so there are fewer plasma proteins like fibrinogen and immunoglobulins available to:
- Neutralize zeta potential (RBC surface charge)
- Promote rouleaux formation
- Lower hematocrit
- White cell count:
- Leukocytosis can lower the ESR by physically interfering with red cell sedimentation, especially at very high WBC counts.
When is ESR elevated?
- Infections (e.g. endocarditis, TB)
- Autoimmune diseases (e.g. lupus, rheumatoid arthritis, vasculitis)
- Malignancies
- Chronic kidney disease
- Anemia
- Pregnancy
When is ESR low?
- Polycythemia (high RBC mass)
- Sickle cell disease (abnormal RBC shape)
- Extreme leukocytosis
- Hypofibrinogenemia
Summary
- ESR is a nonspecific marker of inflammation. Think of it as a blunt instrument—useful for tracking disease activity over time (like in temporal arteritis or RA), but not for diagnosis alone.
- ESR is not just a reflection of plasma proteins; it’s also influenced by RBC characteristics, including shape, size, and flexibility.
- So, in sickle cell disease or hereditary spherocytosis, you may see unexpectedly low ESR even during active inflammation.
Food for thought
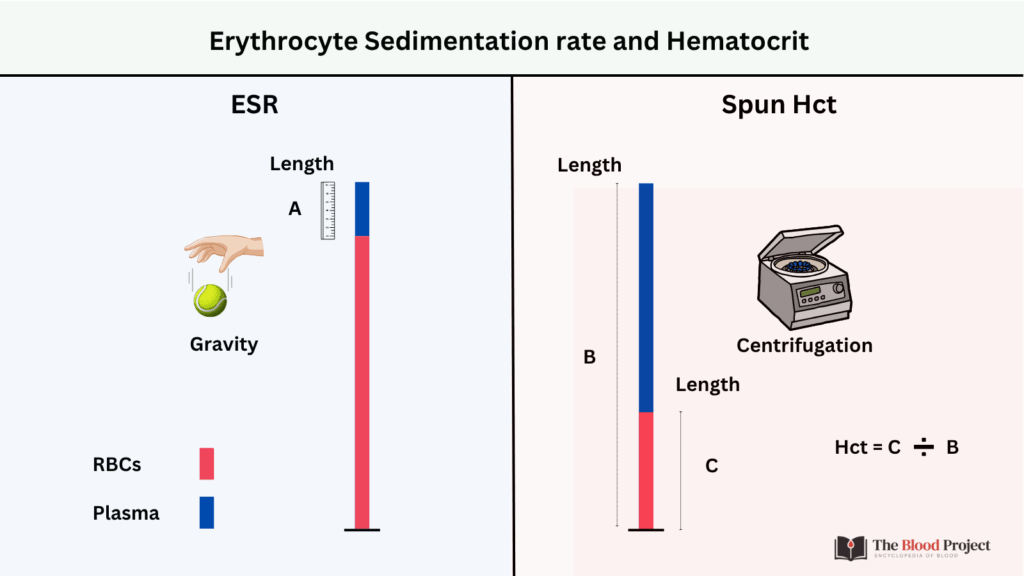
The Erythrocyte Sedimentation Rate (ESR) and the spun Hematocrit (Hct) test both rely on the principle of gravitational settling of red blood cells (RBCs), but they differ in purpose, method, and interpretation.
Similarities:
- Both measure how RBCs settle over time
- Both use a narrow tube (Westergren or capillary)
- RBCs settle downward in both
- Both visually separate plasma from RBCs
Differences:
- Hct measures RBC volume fraction (i.e., % of blood that is RBCs), ESR measures inflammation (indirectly)
- Hct uses a centrifuge to spin red cells down, ESR uses gravity
- Hct is measured as %, ESR as mm/hour
- Hct takes < 5 min, ESR takes 1 hour
- Hct is not affected by rouleaux, fibrinogen or immunoglobulin levels, ESR is
