Michaelis sign
- Named after Hans Michaelis, a gynecologist from Prussia.
- Low grade fever without other cause.1
- Michaelis described the relationship between temperature and thrombosis:
- “If I were asked, how do you explain these small temperature increases? The expression of what kind of process should they be attributed? I would say it is a sign that a thrombus is there, which is not organized in the normal way, but is perhaps in the process of dissipating from which even the smallest particles are already crumbling and circulating in the blood. However, without any bacterial involvement the softening can be explained by the increase in temperature. (…) I do not claim that any unexplained occurrence of subfebrile temperatures indicates an embolic risk, but I must say again according to my observations puerperal postoperative thromboses and embolisms do not occur out of the blue; there is a premonitory symptom in the form of subfebrile temperature. If this occurs, one must think of the possibility of thrombosis or embolism and act accordingly.”
- According to Michaelis the increase in temperature occurs prior to thrombosis and embolism. According to Michaelis “not every subfebrile temperature is an index of the onset of thrombosis, but anything over 37.5 °C suggests the necessity for caution and close supervision of the patients, guarding them against any violent movement, any excitement or fright, and keeping the bowels loose with oil injections, a mild laxative, and suitable diet.”
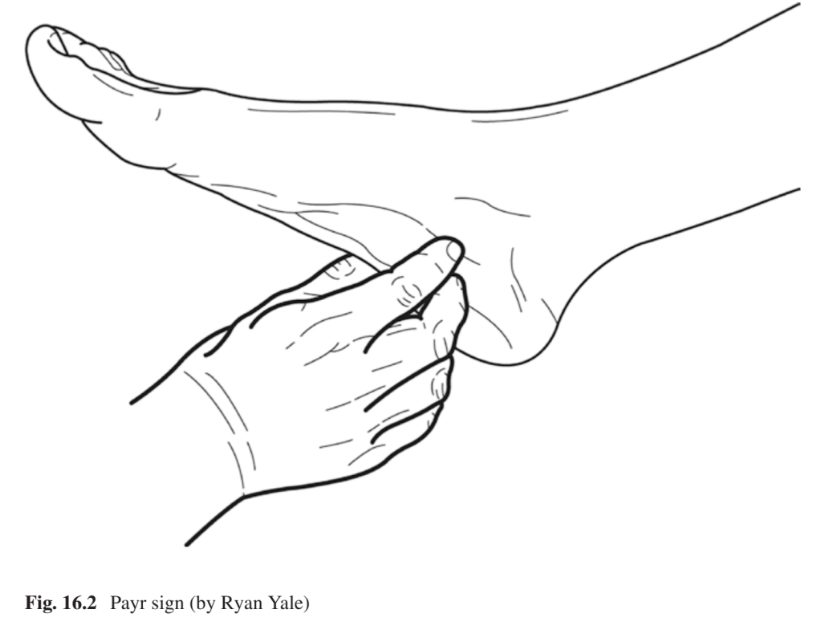
Payr’s sign
- Named after Erwin Payr (1871-1946), a surgeon from Austria.2
- Strong pressure is exerted on the soles of the patient’s feet with both thumbs along the medial plantar surface. Clear pressure pain is a possible sign of DVT.
- Payr Reported that in 152 postoperative cases, 21 (13%) had thrombosis:3
- 5 had pain in the sole of the foot as first sign.
- 11 had pain in the sole of the foot simultaneous with the appearance of mild subjective or objective signs of thrombosis.
- 5 cases had no pain in the sole of the foot.
- In the description of the physical finding, Payr stated:
Mahler sign
- Named after Richter A. Mahler (1863–1941), who was from Budapest.
- Increased pulse disproportionate to the temperature; after an initial increase, the temperature falls while the pulse steadily increase.4
- 1908 translation of Mahler’s work:
- “In a typical thrombosis the pulse rises and continues to rise while the temperature remains perfectly normal. If there is edema, a thrombotic strand may be palpable, or, if pulmonary symptoms arise the pulse beat reaches its highest point and occasionally the temperature goes up at the same time. While the temperature will be found to fall during the next few hours, the pulse will remain rapid for several days. Sometimes the recognition of thrombosis is made more difficult by a gradual increase in the pulse rate simultaneous with a slight rise in temperature at the very commencement of the process. In such cases however, the diagnosis is pretty certain when there is a marked divergence between the pulse and temperature curves. On the other hand, there are cases where the gradual increase in the pulse rate is not marked, the temperature is normal, and then, again, there may be a small and very rapid pulse. In these cases one should also take into consideration the possibility of a thrombosis.”
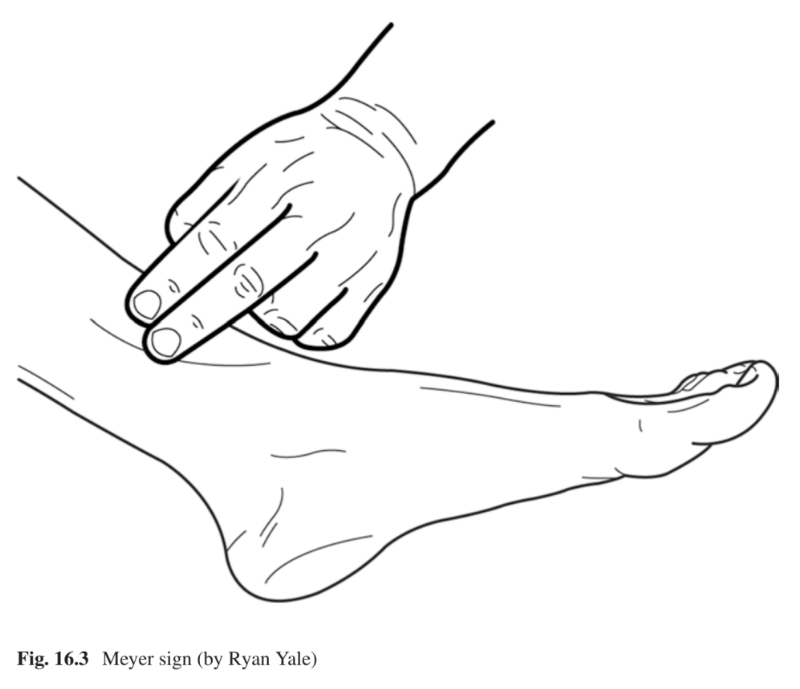
Myer sign
- Named after Otto Meyer (1896-?) who practiced medicine in New York City.
- Refers to compression of the posterior tibial vein at the lower third of the leg against the medial side of the tibia.5
- Published a book entitles Phlebitis: The Hidden Cause of Most Leg and Foot Ailments (1940).
- In 1932, he described in a paper:
- “The most precise tender point on the posterior tibial vein is located at the lower third of the leg when pressure is applied pushing the vein against the medical surface of the tibia.”
Pratt sign
- Named after Gerald Hilary Pratt (1906–1979), a surgeon who was born in Montello, and practiced in New York City.
- The slightly bent knee is grasped forward from below by both hands and pressure is applied with the fingertips to the veins running in the hollow of the knee. Any pressure pain elicited is a possible sign of thrombosis.
- In 1948, Pratt reported on the presence of three dilated veins over the tibia as an early sign of thrombosis of the deep veins of the leg.
- In his 1949 paper on “An early sign of femoral thrombosis” he stated that: “Since then, this phenomenon has been observed so consistently that the term ‘sentinel’ veins has been coined for this finding”. He found that the sign was present in 84 of 109 patients with thrombosis of the leg and that it is present earlier than Homans’ sign
- He attributed the pathogenesis to “These three small veins over the tibia empty into the saphenous and the anterior tibia vein system are superficial and unsupported but musculature and therefore dilate very early.”
Sigg sign
- Named after Dr. Karl Sigg (1912–1986), who was born in Basel, Switzerland
- Refers to pain in the popliteal fossa on passive extension of the knee.
- The outstretched leg is lifted gently with one hand while the other hand pushes down on the patella, thus overstretching the knee joint. Pains in the hollows of the kneed are considered a sign of thrombosis.
- provoking pain in the same region by extension in the knee, PMID: 22959541
- Wupperman described a sign of pain in the knee-joint during hyperextension for diagnosing DVT that he dedicated in gratitude to his revered teacher Karl Sigg. The maneuver is performed as follows: Pressure is applied to the patella with one palm and simultaneously, the heel is lifted with the other hand, and causes a strong pain in the popliteal fossa. This pain can also be provoked by vigorous pressure on the patella with the leg stretched out on a firm support [51]. In patients with phlebographically proven thromboses, a mean positive accuracy of 0.83 and a mean specificity of 0.56 was found for Sigg sign [51]. They found that Sigg sign, compared to Lowenberg, Bisgaard, Payr, Homans, Deneke, and Pratt signs, as well as pressure pain in the calf, showed the highest observed overall mean positive postoperative accuracy (0.57), while the overall specificity did not differ from the other signs of thrombosis (0.62)
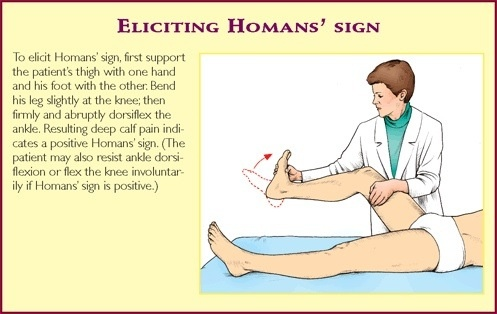
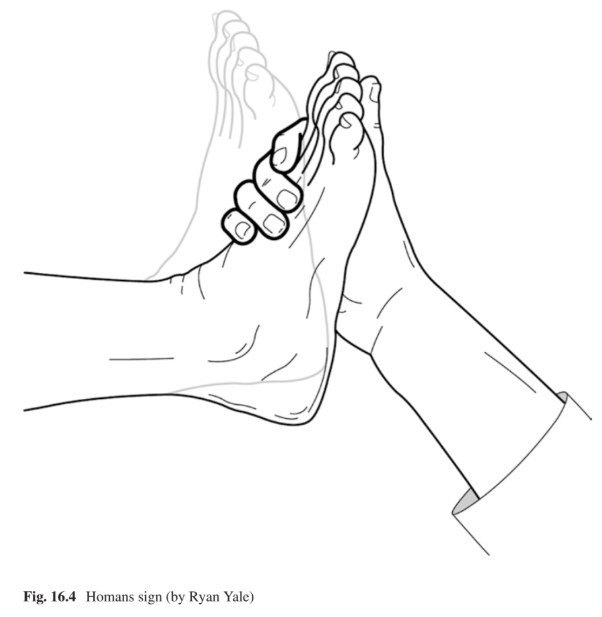
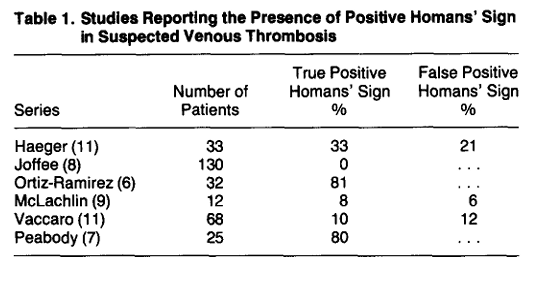
Homans sign
- Named after John Homans (1877-1954), a surgeon who graduated from Harvard Medical School and trained at the Massachusetts General Hospital.
- With one hand, the lower leg is grasped above while the forefoot is grasped by the other hand from the medial and plantar side. Sudden dorsiflexion of the ankle joint with the knee flexed to 30° produces discomfort in the upper part of the calf.67.
- Homans described the dorsiflexion sign in 1941 in his paper “Exploration and division of the femoral and iliac veins in the treatment of the thrombophlebitis of the leg” as a “discomfort behind the knee on forced dorsiflexion of the foot.”
- In describing the course of disease, he wrote: “The swelling and cyanosis, if any, always disappear in a few days, but the dorsiflexion sign usually lasts for a week or more. (…) If, on the other hand, when the patient first gets up, the discomfort, edema and especially the dorsiflexion sign reappear, the superficial femoral vein is at once exposed and divided.”
Lowenberg test
- The sign is named after Robert I. Lowenberg (1917–2000), a vascular surgeon in the Department of Surgery, General Service at Grace-New Haven Community Hospital, Connecticut.
- Lowenberg test is an attempt to quantify Homan’s sign by inflating a pneumatic cuff around the calf muscles and measuring the pressure that provokes pain PMID: 229595418
- Lowenberg described the sign in 1954. Lowenberg, R. I. (1954). “Early Diagnosis of Phlebo Thrombosis with Aid of a New Clinical Test”. JAMA: The Journal of the American Medical Association. 155 (18): 1566–70, He wrote:
- “A pneumatic cuff is distended over the calf or thigh slowly to 180 mmHg pressure. If pain is elicited before this, the end point has been reached, and the cuff is deflated. A positive cuff test is indicated by pain beneath the inflated cuff at 80, 100, or 120 mmHg. A negative test that becomes positive a few days post-operatively or several days after a patient has been put to bed with a myocardial infarction is presumed evidence of intravascular clot and should be treated as such [181, p. 883].”
Rieländer sign
- Named after Wilhelm August Rieländer (1875–1926), a German gynecologist/midwife.
- Rieländer reported that “pain in the groin, especially under Poupart’s ligament” along with “pain to pressure on the corresponding side of the abdomen” is a symptom found in thrombosis of the leg during the puerperium period.9
Other eponymic signs10
| Sign | Named After | Description |
|---|---|---|
| Ducuing Sign | Joseph Ducuing (1885–1963) | Pain elicited with gentle palpable pressure under the inguinal ligament, iliac fossa, popliteal fossa or calf. |
| Denecke Sign | Kurt Denecke (1903–1991) | Sharp pain located in the posterior region of the plantar arch in the sole of the foot occurring upon standing after prolonged bedrest. |
| Olow Sign | John Olow (1883–1948) | Calf is grasped between the knee, lower and middle third of the leg (where the triceps surae forms the Achilles tendon). Sign is positive if pain is felt when forward moderate pressure is applied anteriorly toward the tibia. |
| Krieg Sign | Erich Krieg (1902–1970) | Pain upon pressure over the vein in the adductor canal, groin, lower leg, calf, or sole of the foot. |
| Westermark Sign | Nils Johan Hugo Westermark (1892–1980) | Absent vascularity on chest radiograph in pulmonary embolism. |
| Pilcher Sign | Robin Sturtevant Pilcher (1902–1994) | In patients with an unexplained rise in temperature, uncover both legs for 10 minutes. If thrombus is present, the leg is warmer on the affected compared to the unaffected leg. |
| Bisgaard Sign | Holger Ove Bisgaard (1880–1943) | Infiltration of the calcaneo-malleolar region causing a deep pressure pain. |
| Bauer Sign | Gunnar Bauer (1895–1970) | Restlessness of the leg and transitory aching of the calf. |
| Bancroft Sign | Frederic Wolcott Bancroft (1880–1963) | Both knees are semi-flexed with the feet resting on the bed. Palpation of the affected leg reveals edema. Pain is elicited when the gastrocnemius muscle is compressed against the posterior surface of the tibia. |
| Moses Sign | William Russell Moses (1916–2005) | Three-part test |
| Neuhof Sign | Harold Neuhof (1884–1964) | Patients’ heels on bed, knees flexed, and calf muscle relaxed. Palpation reveals thickening and infiltration deep to the gastrocnemius muscle. |
| Bailey Sign | Henry Hamilton Bailey (1894–1961) | Fingertip pressure is applied over each saphenous opening. Using a stroking motion, the finger in the other hand moves inferiorly following the course of the femoral vein. A positive sign is the presence of unilateral segment of localized tenderness. |
| Lawrence Sign | Elias D. Lawrence (1905–1994) | Coughing, sneezing, or laughing increases pain in an inflamed area in the lower extremity. In cases of either early DVT or in proximal thrombosis, compression of the greater saphenous vein close to the saphenofemoral junction causes pain to disappear when coughing. In case of DVT below the knee, this same maneuver causes the pain to disappear in 50% of cases. |
| D’Alessandro Sign | Arthur Joseph D’Alessandro (1911–1983) | Marked diminution or absence of the femoral pulse. |
| Louvel Sign | Jacques Louvel (1898–1983) | Pain in an inflamed superficial venous segment in the lower extremity induced by coughing. |
| Ortiz-Ramírez Sign | Teófilo Ortiz-Ramírez was born in 1901 | Patient recumbent and extremity slightly flexed. A sphygmomanometer cuff is applied above the knee and inflated to 40 mmHg. Pain most commonly occurring in the popliteal region is a positive test and disappears with the deflation of the cuff. |
| McLachlin Sign | John Adams McLachlin (1915–2004) | Unilateral swelling of the left ankle. |
| Peabody Sign | Charles Newton Peabody (1925–2011) | Patient supine and examiner places the thumb against the second metatarsals on the plantar surface of the feet. Using pressure, raise the feet approximately 20 inches off the bed. The examiner observes for evidence of plantar flexion by noting the relative position of the first metatarsals medially. |