I posted a Twitter poll asking whether you would provide a patient with newly diagnosed warm autoimmune hemolytic anemia with prophylaxis for Pneumocystis jiroveci pneumonia with bactrim and/or peptic ulcer disease with a proton pump inhibitor (PPI). There were not enough room in the poll to entertain the possibility of prophylaxis against osteoporosis.
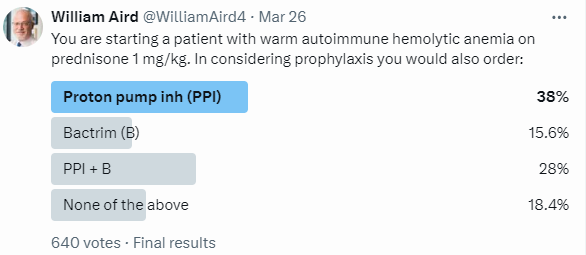
The most popular answer was PPI alone followed by both bactrim and PPI. Evidence for the risk-benefits of prophylaxis for Pneumocystis jiroveci pneumonia in patients with autoimmune disease is poor as it is for the prevention of peptic ulcer disease (PUD) in any patient taking high dose, long-term corticosteroids. The strength of evidence for preventing osteoporosis and hip fractures (not covered in the poll) in patients taking steroids is stronger.
The correct answer to the question depended on data I did not provide 😊:
- Regarding prophylaxis for Pneumocystis jiroveci, does the patient have an additional cause of immunodeficiency?
- Regarding prophylaxis for peptic ulcer disease, is the patient otherwise at high risk for PUD, e.g. are they taking NSAIDS?
Bottom line:
Overview
- Corticosteroids are an effective treatment option for several diseases spanning many specialties. It is estimated that 1% of the US population is treated with long-term corticosteroids.1
- Long-term corticosteroid treatment is associated with a number of dose-dependent side effects including:
- Hypertension
- Hyperglycemia
- Weight gain
- Adrenal suppression
- Osteoporosis2
- GC doses ≥ 2.5mg/day increase fracture at both the spine and hip
- GC doses <2.5 mg/day increase the risk of spinal fractures
- Both high daily (≥30 mg/day) and high cumulative (≥5 g/year) doses of GCs further increase the risk of fragility fractures
- Peak incidence of fractures is at 12 months
- The highest rate of bone loss occurs within the first 3 to 6 months of GC treatment, due to early osteoclast activation followed by decreased osteoblast proliferation and increased apoptosis of osteoblasts and osteocytes.
- Infections
- Possibly peptic ulcer disease
- The most common targets of prophylaxis are:
- Pneumocystis jiroveci pneumonia
- Peptic ulcer disease
- Osteoporosis
Pneumocystis
- Pneumocystis jirovecii is an opportunistic fungal pathogen that causes life-threatening pneumonia in immunocompromised patients.
- PCP can be prevented by:
- Reducing immunosuppression
- Using chemoprophylaxis
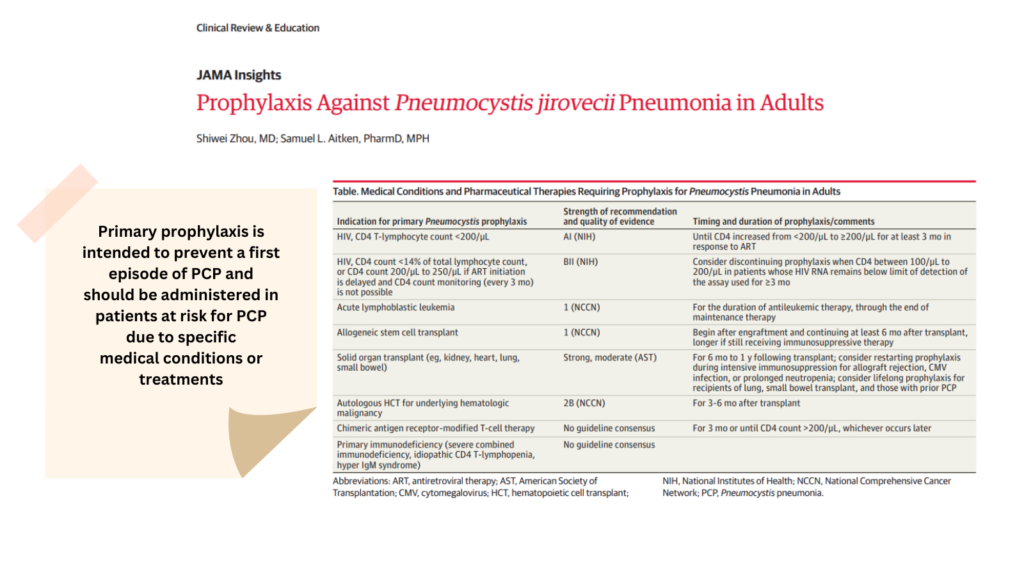
- Primary prophylaxis for PCP is recommended:34
- For patients with HIV/AIDS:
- Who have CD4 T-lymphocyte count less than 200/μL
- Whose CD4 cell percentage less than 14% or CD4 lymphocyte count between 200/μL and 250/μl and whose ART is delayed or who cannot receive CD4 monitoring at least every 3 months.
- For patients without HIV who are immunocompromised, including:
- Those with acute lymphoblastic leukemia receiving antileukemic therapy
- Recipients of allogeneic hematopoietic cell transplant
- Recipients of solid organ transplant
- Patients treated with the anti-CD52 antibody alemtuzumab, phosphatidylinositol 3-kinase inhibitors (eg, idelalisib, duvelisib), or temozolomide with concurrent radiotherapy
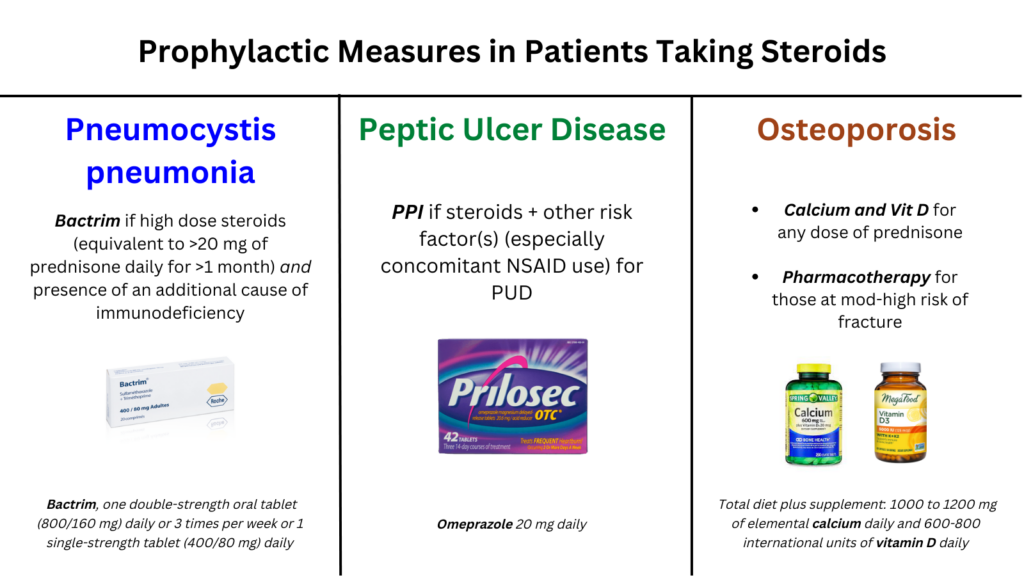
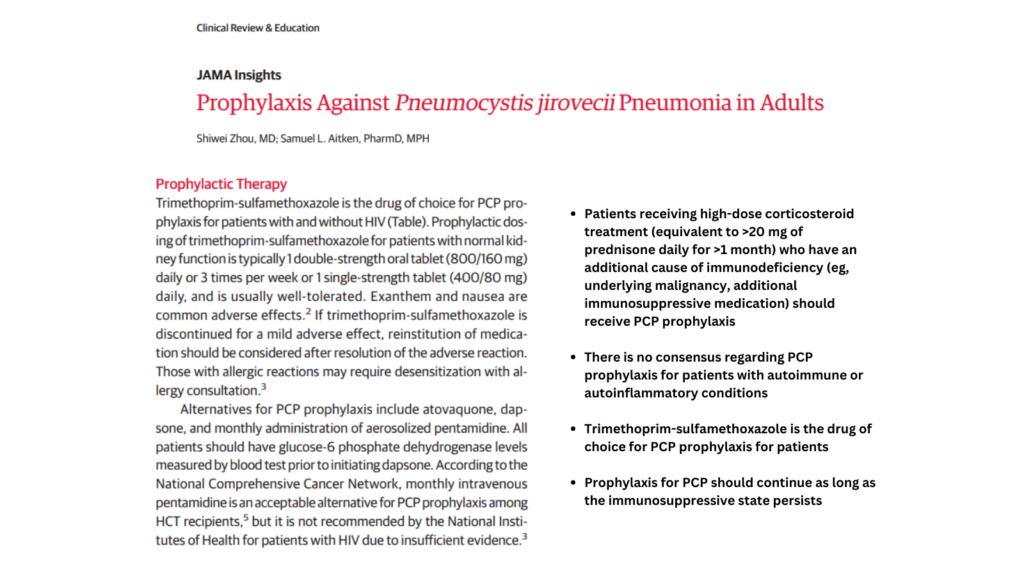
- Patients receiving high-dose corticosteroid treatment (equivalent to 20 mg of prednisone daily for 1 month) who have an additional cause of immunodeficiency (eg, underlying malignancy, additional immunosuppressive medication).5
- For patients with HIV/AIDS:
- UpToDate: We recommend PCP prophylaxis for patients receiving a glucocorticoid dose equivalent to ≥20 mg of prednisone daily for one month or longer who also have another cause of immunocompromise (eg, certain hematologic malignancies or a second immunosuppressive drug).
- Trimethoprim-sulfamethoxazole is the drug of choice for PCP prophylaxis for patients with and without HIV.6
- Prophylactic dosing of trimethoprim-sulfamethoxazole for patients with normal kidney function is typically 1 double-strength oral tablet (800/160 mg) daily or 3 times per week or 1 single-strength tablet (400/80 mg) daily.7
- Alternatives for PCP prophylaxis include:8
- Atovaquone
- Dapsone
- Aerosolized pentamidine
- Prophylaxis for PCP should continue as long as the immunosuppressive state persists.9
Peptic ulcer disease
- There is a theoretical benefit of reducing gastric pH with agents such as proton-pump inhibitors (PPIs) to prevent steroid-induced peptic ulcers.
- However, there is limited data:
- To show that corticosteroids actually cause peptic ulcers in the first place:
- In 1976, a meta-analysis of about 3600 patients from 26 prospective, randomized, double-blind, placebo-controlled trials found no difference in ulcer risk over placebo with an absolute risk of about 1%.
- A meta-analysis in 1983 challenged these findings and found a relative risk (RR) of 2.3 (CI 1.4 – 3.7).
- In 1991, a nested case-control study of 1415 patients found that ulcer risk was only increased in concurrent users of non-steroidal anti-inflammatory drugs (NSAIDs): RR 1.1 for corticosteroid alone, RR 4.4 for corticosteroid use in patients already on NSAIDs, RR 14.6 for corticosteroid and NSAIDs compared to controls.
- In 2001, a similar nested case-control study from the UK of 2105 cases looking at upper gastrointestinal complications found odds ratios (OR) of 1.8 for users of corticosteroids alone, 4.0 for users of NSAIDs alone, and 8.9 for users of both.
- To show that reducing gastric pH with agents such as proton-pump inhibitors (PPIs) prevents steroid-induced peptic ulcer, if there is such an association.
- To show that corticosteroids actually cause peptic ulcers in the first place:
- Unlike corticosteroids, a significant evidence base shows a direct causal relationship between NSAID use and new ulcer formation.10
- When used with NSAIDs, corticosteroids increase the risk of GI bleeding due to poor ulcer healing.11
- Incidence risk ratio of GI bleeding with the concomitant use of corticosteroids and nonspecific NSAID or low‐dose aspirin is 12.82 and 8.37, respectively, the highest of any drug combination.12
- Expert opinion:13
- The literature suggests no benefit from PPI prophylaxis in patients taking systemic corticosteroids without concomitant NSAID use.
- PPIs have been linked to numerous adverse events including:
- Renal disease
- Clostridium difficile infection
- Skin rash
- Expert opinion:14
- Arguments for not routinely ordering PPI prophylaxis for patients on high‐dose corticosteroids:
- Corticosteroids are not fundamentally ulcerogenic.
- PPIs cause harm.
- The inappropriate use of PPIs significantly increase healthcare costs.
- Treat patients who:
- Concomitantly use NSAIDs along with corticosteroids with prophylactic PPIs.
- Concomitantly use antiplatelet agents or anticoagulants.
- Have a prior history of peptic ulcer disease.
- Arguments for not routinely ordering PPI prophylaxis for patients on high‐dose corticosteroids:
- Expert opinion:15
- Glucocorticoid therapy with concomitant nonsteroidal anti-inflammatory drug use in creases the risk of peptic ulcer disease and gastrointestinal bleeding
- Proton pump inhibitors are an effective means of gastrointestinal prophylaxis, but they are not without side effects.
- Patients who must take a combination of glucocorticoids and nonsteroidal anti-inflammatory drugs should be prescribed prophylaxis with a proton pump inhibitor (PPI).
- In patients with other risk factors for PUD, including those with previous peptic ulcer disease, heavy smokers, heavy alcohol users, patients [65 years of age, and patients taking other medications that may increase the risk of PUD, such as bisphosphonates, clinicians may choose to prescribe PPIs.
- For those taking glucocorticoids alone, without other risk factors, routine use of a PPI is not recommended.
- Options include:16
- Esomeprazole 20 mg and 40 mg
- Pantoprazole 20 mg and 40 mg
- Lansoprazole 15 mg and 30 mg
- Omeprazole 20 mg and 40 mg
- Rabeprazole 20 mg
- AGA Clinical Practice Update on De-Prescribing of Proton Pump Inhibitors: Expert Review:17
- Proton pump inhibitors are not indicated for long-term use in those taking steroids in the absence of ASA/NSAID use.
- PPIs should not be de-prescribed in those at high risk for upper GI, for example those:
- With a history of upper GI bleeding.
- Taking multiple antithrombotics (including both anticoagulants and antiplatelet agents.
- Taking aspirin or a nonsteroidal anti-inflammatory drug with an additional risk factor for upper GI bleeding, for example:
- Older than 60 years
- Severe medical comorbidity
- Using second nonsteroidal anti-inflammatory drug or aspirin
- Taking an antithrombotic
- Taking an oral corticosteroid
Osteoporosis
- Agents available for prophylaxis include:
- Calcium
- Vitamin D
- Bisphosphonates
- Teriparatide (an analogue of parathyroid hormone)
- UpToDate: “Calcium and vitamin D – For all patients receiving any dose of chronic glucocorticoid therapy or initiating glucocorticoids with an anticipated duration of ≥3 months, we suggest calcium and vitamin D supplementation (Grade 2B). Most adults require 1000 to 1200 mg of elemental calcium daily, total diet plus supplement, and 800 international units of vitamin D daily“.
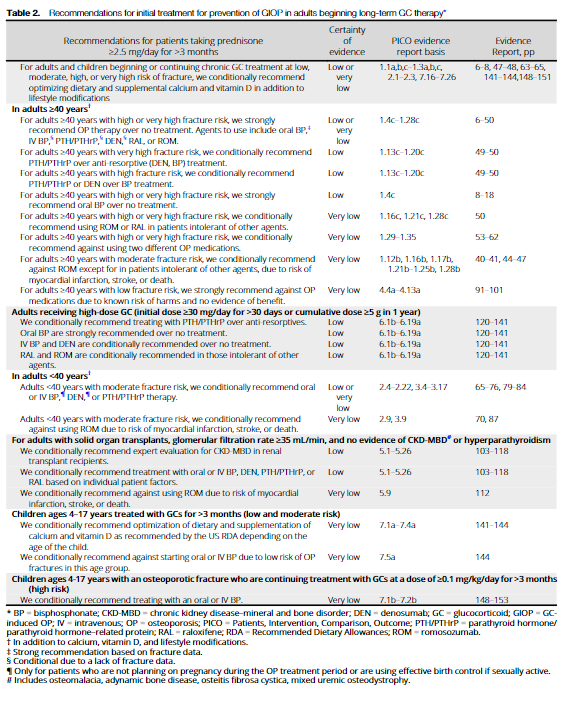
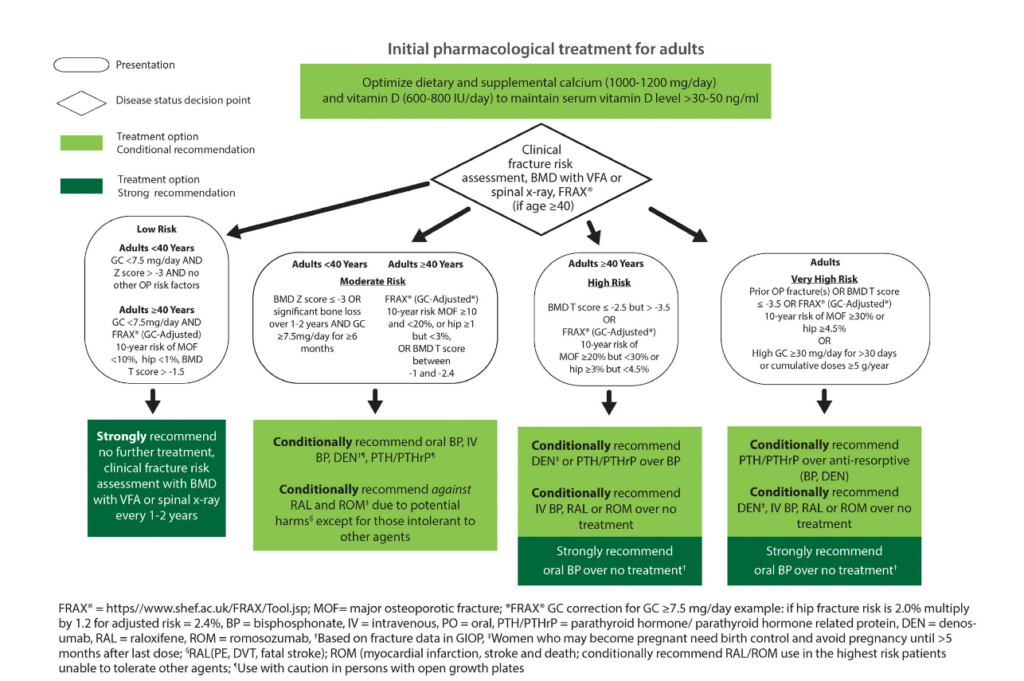
- American College of Rheumatology (ACR) Guideline for the Prevention and Treatment of Glucocorticoid-Induced Osteoporosis:
- Screening recommendations:
- For all adults (≥18 years old) initiating or continuing glucocorticoid therapy ≥2.5 mg/day for >3 months, screen for fracture risk:
- ≥40 years of age:
- Assess with:
- FRAX
- BMD using dual-energy x-ray absorptiometry (DXA) with vertebral fracture assessment (VFA) testing or spinal x-ray
- Assess with:
- <40 years of age:
- Assess with BMD with VFA testing or spinal x-ray.18
- Risk categories:
- Low, moderate, and high risk categories are based on DXA and/or FRAX assessments.
- Very high risk category based on:
- Prior osteoporotic fractures
- Very low BMDs
- Very high FRAX risks
- High daily dose or high cumulative doses of glucocorticoid
- ≥40 years of age:
- For all adults (≥18 years old) initiating or continuing glucocorticoid therapy ≥2.5 mg/day for >3 months, screen for fracture risk:
- Recommendations for initial treatment:
- All patients
- For all adults and children beginning or continuing chronic glucocorticoid at a dose of ≥2.5 mg/day for >3 months, we conditionally recommended optimizing age appropriate dietary and supplemental calcium and vitamin D, in addition to life-style modifications.
- In adult patients with:
- Low fracture risk, we strongly recommend against adding oral or IV oral bisphosphonates (BP), PTH/PTHrP, raloxifene (RAL), denosumab (DEN), or romosozumab (ROM).
- Moderate fracture risk:
- We condition-ally recommend oral or IV BP, parathyroid hormone (PTH)/PTH-related protein (PTHrP), or DEN over no treatment.
- We conditionally recommend against ROM and RAL therapies except in those intolerant of other OP medications, due to possible life-threatening harms, including thrombosis, fatal stroke, major cardiovascular events, and death.
- High or very high fracture risk, we strongly recommended treatment with OP therapy overtreatment with calcium and vitamin D alone.
- For adults≥40 years with:
- Low fracture risk:
- We strongly recommend against OP medications due to known risk of harms and no evidence of benefit.
- Moderate fracture risk:
- We conditionally recommend against ROM except in patients intolerant to other agents.
- High or very high fracture risk:
- We strongly recommended treatment with OP therapy over treatment with calcium and vitamin D alone. Agents to use include:
- oral BP
- IV BP
- PTH/PTHrP
- DEN
- RAL
- ROM
- We strongly recommended oral BP over no treatment.
- We conditionally recommend using ROM or RAL in patients intolerant of other agents.
- We strongly recommended treatment with OP therapy over treatment with calcium and vitamin D alone. Agents to use include:
- For adults≥40 years with high fracture risk:
- We conditionally recommend PTH/PTHrP or DEN over BP.
- Very high fracture risk, we conditionally recommend PTH/PTHrP over anti-resorptives (BP or DEN).
- Low fracture risk:
- For adults <40 years with:
- Moderate fracture risk:
- We conditionally recommend oral or IV BP, DNE or PTH/PTHrP therapy.
- We conditionally recommend against using ROM due to risk of AMI, stroke or death.
- Moderate fracture risk:
- All patients
- Screening recommendations: