We posted a poll on twitter on 2/9/24 asking the following question:
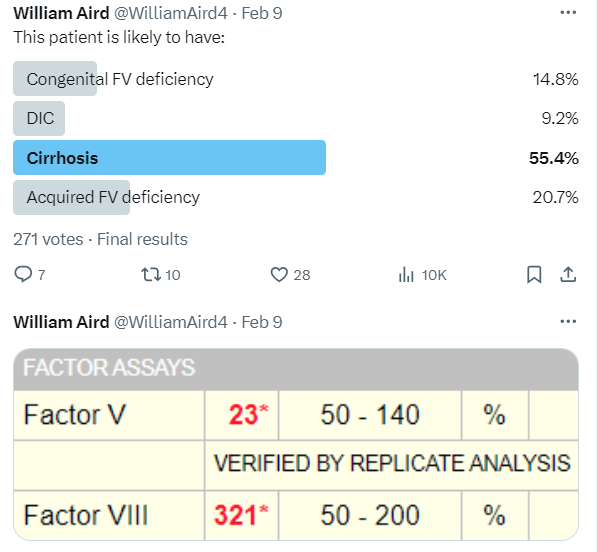
- Cirrhosis was the most popular answer followed by acquired FV deficiency.
- In fact, any one of these conditions might explain the factor assay results:
- Congenital and acquired FV deficiency would explain the low FV, but not the elevated FVIII levels, unless the patient had another cause for the latter, for example underlying inflammation (since FVIII is an acute phase reactant).
- Cirrhosis or disseminated intravascular coagulation (DIC) are both associated with low FV levels. Patients with cirrhosis also have elevated FVIII levels. Contrary to conventional wisdom, DIC is also commonly associated with elevated FVIII levels.
- Cirrhosis is the most likely explanation only because its higher prevalence increases its pretest probability.
Below, we will:
- Examine conflicting expert opinion about the use of FVIII to distinguish between cirrhosis and DIC.
- Address the coagulopathy of DIC
- Discuss the coagulopathy of liver disease
The bottom line is that FVIII cannot be used to distinguish between DIC and cirrhosis!
Expert opinion on using FVIII to distinguish between DIC vs. liver disease
- FVII is helpful in differentiating DIC from cirrhosis:
- “The PT and aPTT are both prolonged in DIC because they contain coagulation factors that have been consumed: factor V, factor VIII, and fibrinogen… factor VIII (made in endothelial cells and not in the liver) may be elevated in liver disease as an acute phase reactant but is consumed and therefore decreased in DIC.”1
- “Factor VIII is high in fulminant hepatic failure and low in disseminated intravascular coagulation (DIC) but this differential diagnosis is seldom an issue in clinical practice.”2
- FVII is not helpful in differentiating DIC from cirrhosis:
- “[In DIC] coagulation proteins with a marked acute phase behavior, such as factor VIII or fibrinogen, are usually not decreased or may even increase… [in liver disease] almost all coagulation factors (except factor VIII and von Willebrand factor) are low.”3
- “The FVIII or von Willebrand factor concentrates are rarely used in patients with sepsis-associated DIC, since these factors are already typically elevated due to the acute-phase reaction.”4
- “The APTT represents the function of the intrinsic coagulation pathway including factor VIII (FVIII), which is known to paradoxically increase in most DIC patients, probably due to the release of von Willebrand factor from the endothelium and the acute phase behavior of FVIII.”5
Disseminated intravascular coagulation (DIC):
- Disseminated intravascular coagulation (DIC) is a hematologic emergency that requires prompt diagnosis and intervention.
- The International Society of Thrombosis and Hemostasis (ISTH) has developed a scoring system to diagnose life-threatening DIC, which includes:
- PT6
- D-dimer
- Fibrinogen
- Platelet count
- Laboratory assays for coagulation factors:
- May be ordered as part of the workup for DIC.
- Are not part of the guideline-based DIC workup.
- Their utility in the evaluation of DIC is not clearly defined.
- Factor VIII:
- Primary data:
- Retrospective study from UChicago Medicine:
- 117 patients were reviewed.
- 47 had complete coagulation data to perform ISTH scoring.
- Of these, 30 met ISTH criteria for DIC (64%).
- The most common underlying diagnosis in those meeting ISTH criteria was sepsis.
- A statistically significant lower FV level was observed in those meeting ISTH criteria.
- No such differences were observed in FVII or FVIII levels
- FVII was reduced in 88 patients
- FVIII was only reduced in 2 of the 117 reviewed patients (2%)
- Retrospective study of 346 patients with DIC:
- Factor VIII:C levels were decreased in only 9% of patients studied; they were increased in the majority of cases.
- Retrospective study of 9 shock patients with suspected DIC and in 5 patients with uncomplicated acute myocardial infarction:
- DIC score based on six routine coagulation and fibrinolysis parameters.
- All shock patients showed high levels of FVIII antigen and activity (average 3-6-fold above normal level).
- There were significant negative correlations between the DIC score on the one hand and ratios of VIII:C/VIIIR:Ag.
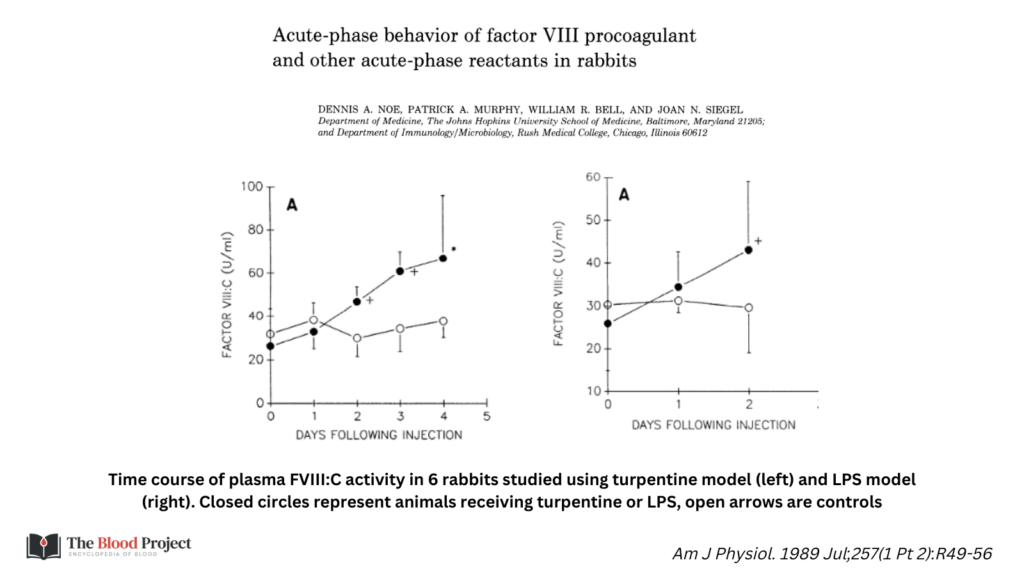
- Study of laboratory models of inflammation in rabbits:
- Retrospective study from UChicago Medicine:
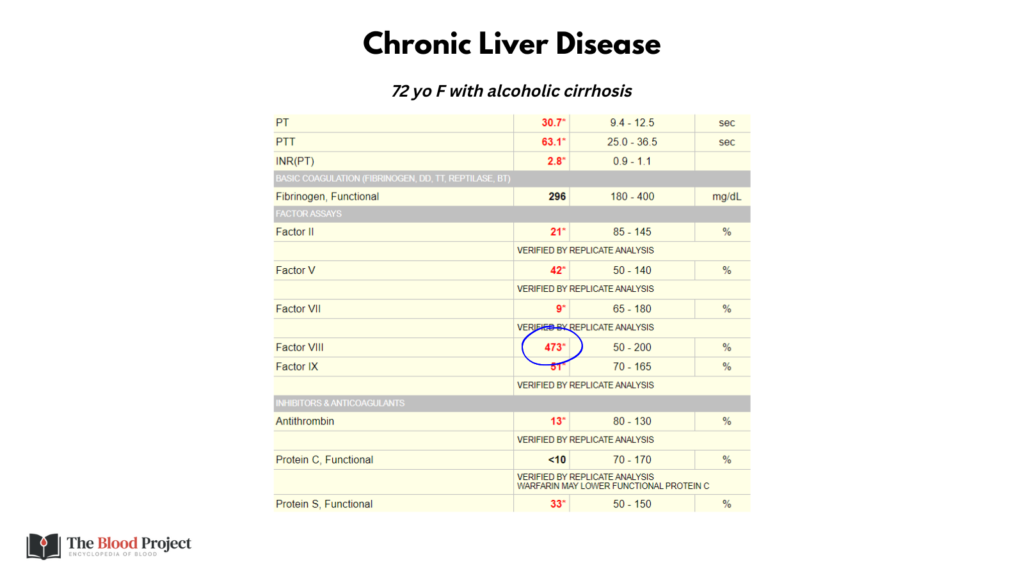
Chronic liver disease:
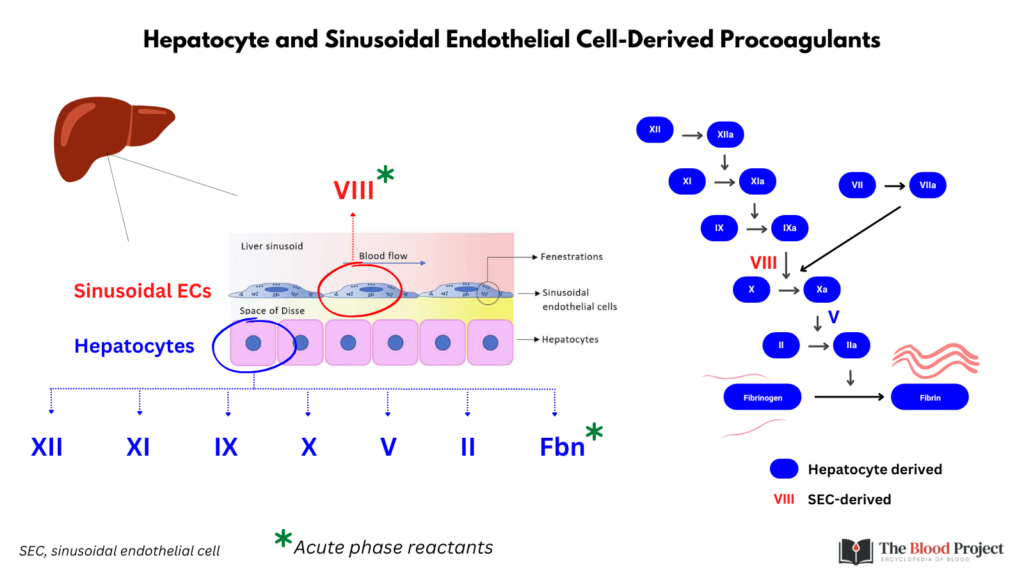
- Liver synthesizes all coagulation factors involved in the generation of a fibrin clot (except factor VIII [FVIII] which is synthesized in endothelium), natural anticoagulants (except thrombomodulin and tissue factor pathway inhibitor), as well as several fibrinolytic proteins.
- Chronic liver disease (CLD):
- Associated with global reduction in the synthesis of numerous procoagulant factors and their inhibitors.9
- Procoagulant and anticoagulant levels usually fall in parallel with the progression of liver disease, although levels vary considerably.
- Fibrinogen levels are normal or increased in most patients with stable cirrhosis. An acquired dysfibrinogenemia develops in 50%-78% of patients with chronic liver disease.10
- Natural anticoagulant protein levels fall progressively with increasing severity of liver disease Antithrombin, protein C and protein S levels range from 10% to 65% of normal, similar to the range of values found in patients with inherited deficiencies.11
- Tissue factor pathway inhibitor (TFPI) is synthesized by endothelial cells. TFPI levels are normal or elevated in patients with chronic liver disease.12
- Acute liver failure (ALF):
- Factor VIII (FVIII):
- Synthesized primarily by liver sinusoidal endothelial cells.
- Often increased several-fold in patients with stable cirrhosis, especially during the advanced/late stages of cirrhosis.
- Increased levels caused by:
- Increased stabilization and half-life owing to elevated von Willebrand factor (vWF).
- Increased synthesis in response to cytokine release from necrotic tissue of cirrhotic liver.
- Reduced clearance due to decreased expression of lipoprotein receptor-related protein.15
- Primary data:
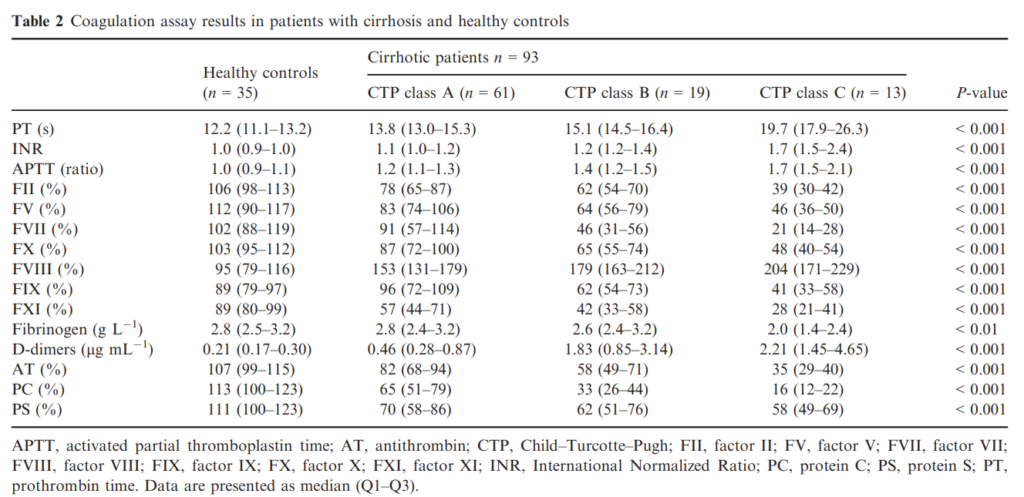
- Prospective study of 35 healthy controls and 93 patients with cirrhosis:
- FVIII levels were > 150% in 48 patients; increase was related to cirrhosis severity:
- 153% [131–179] for CTP-A
- 179% [163–212] for CTP-B
- 204% [171–229] for CTP-C
- Levels of other clotting factors were decreased.
- FVIII levels were > 150% in 48 patients; increase was related to cirrhosis severity:
- Prospective study of 35 healthy controls and 93 patients with cirrhosis:
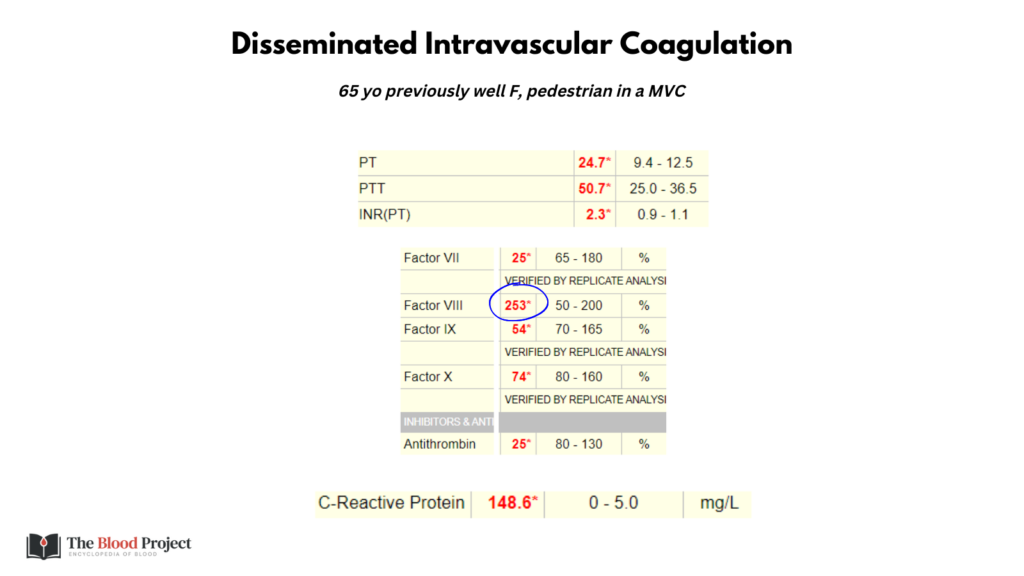
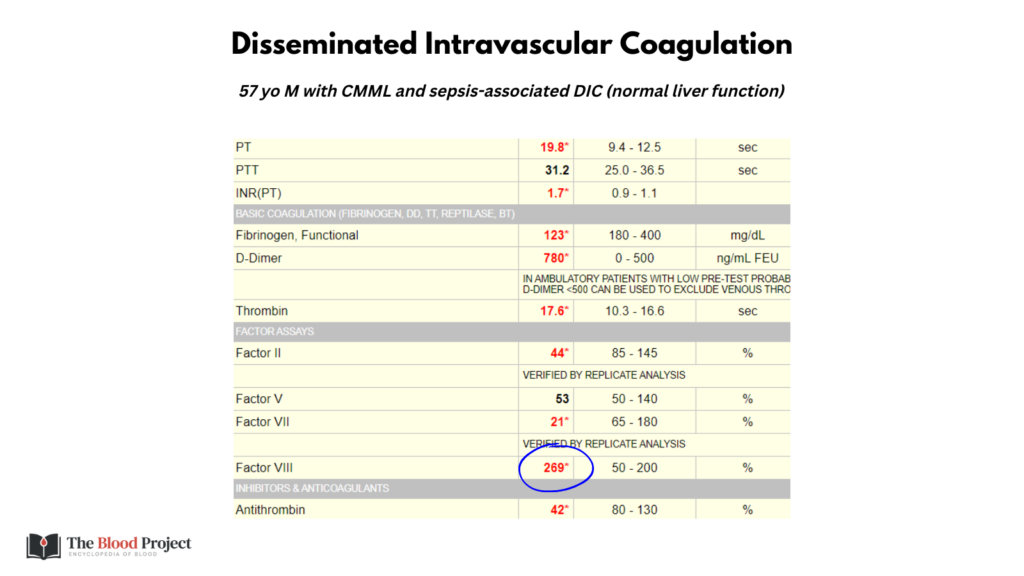
Examples of cases:
.
.
