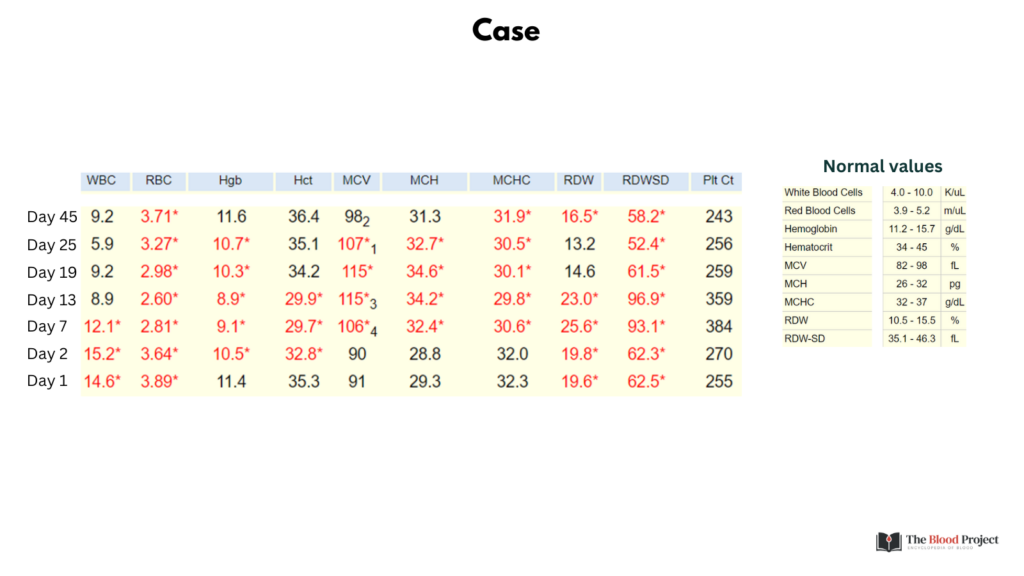
Unknown CBC
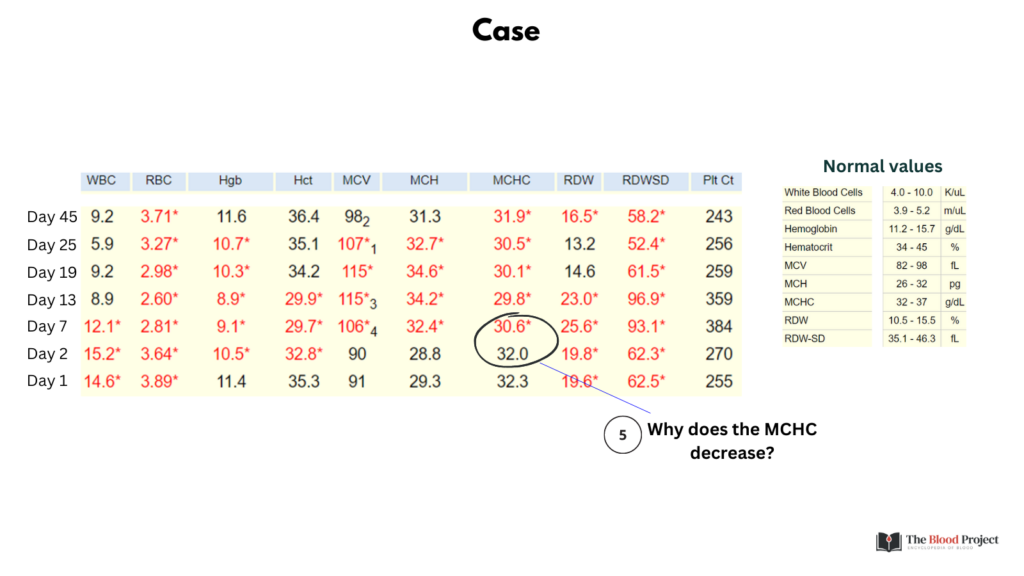
Check out the CBC time series in the graphic. Can you make a spot “diagnosis”, namely the underlying pathophysiological process? If not, refer to the questions on the following slide.
The following graphic includes 6 questions. We will address each in turn on the following slides.
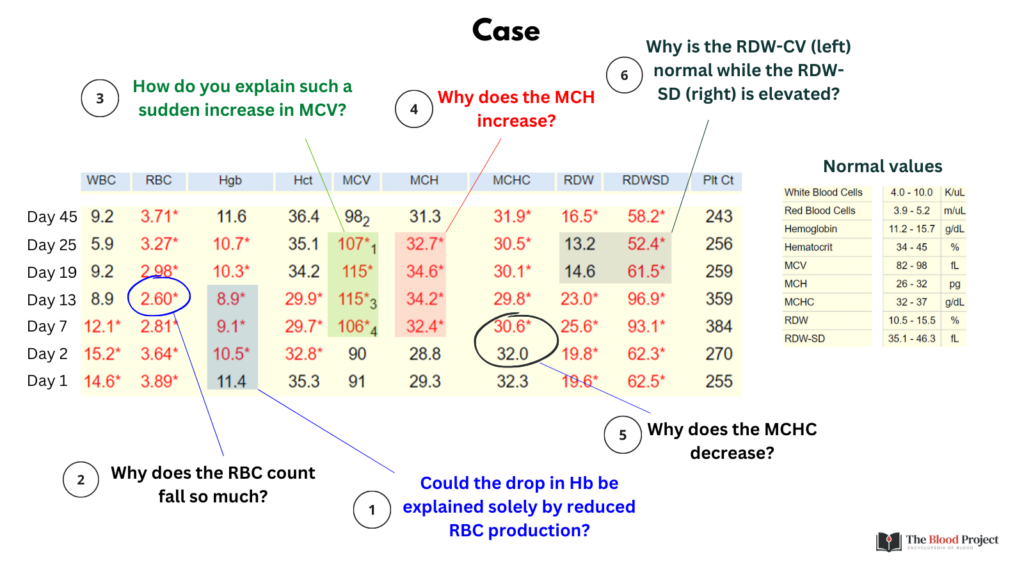
Question 1: Could the reduction in Hb over the first 13 days be attributed to decreased erythropoiesis alone?
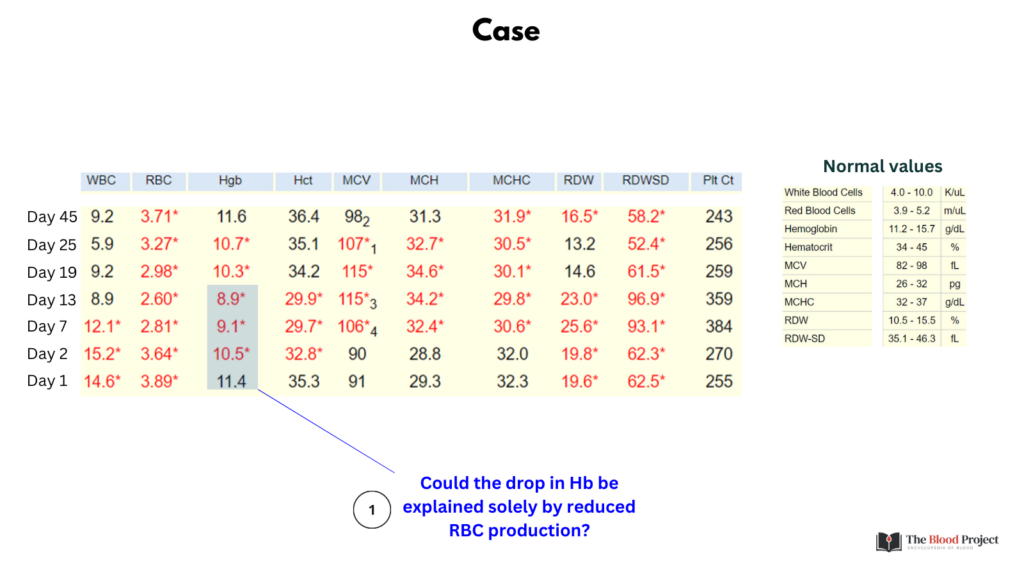
Answer 1: No. Given the long lifespan of a red blood cell (about 120 days), complete cessation of erythropoiesis would lead to a reduction in Hb of about 0.1 g/dL/day. So, with a starting of Hb of 11.4 g/dL, by day 13 one would expect a Hb of 11.4 – (0.1 g/dL/day x 13 days) = 10.1 g/dL. Therefore, the patient is either bleeding and/or has shortened red blood cell survival (i.e., hemolysis). (We cannot rule out an effect of dilution from IV fluids early in the time course).
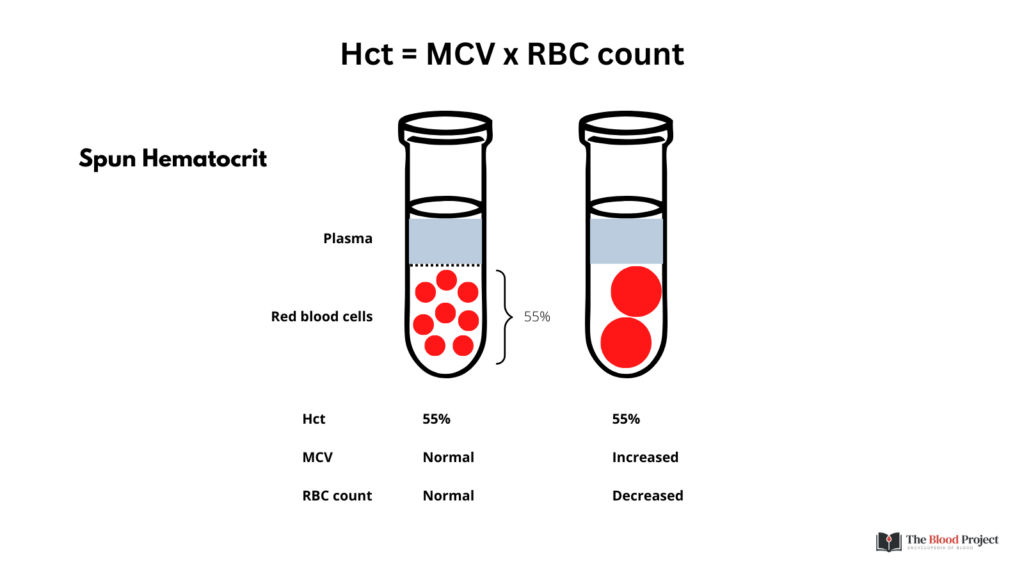
Question 2: Why does the red blood cell (RBC) count drop more than the Hb or Hct between days 1 and 13?
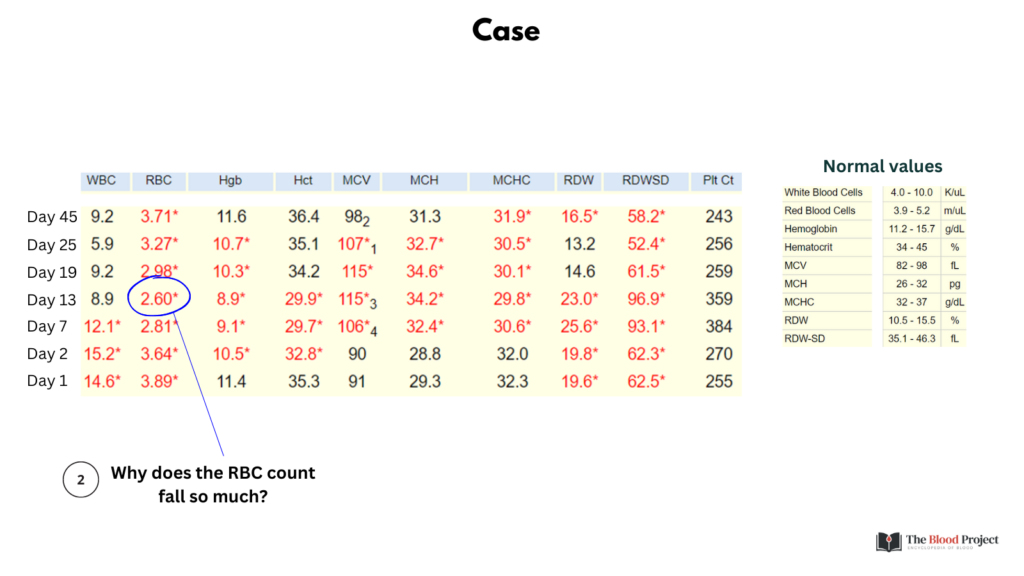
Answer 2: The RBC count drops more relative to the Hct/Hb because the MCV increases during this time. Hct = MCV x RBC count. Therefore for a given Hct, if the MCV increases, the RBC count decreases. The disproportionate reduction in RBC count is consistent with new onset macrocytosis.
Question 3: How do you explain such a sudden increase in the mean cell volume (MCV)?
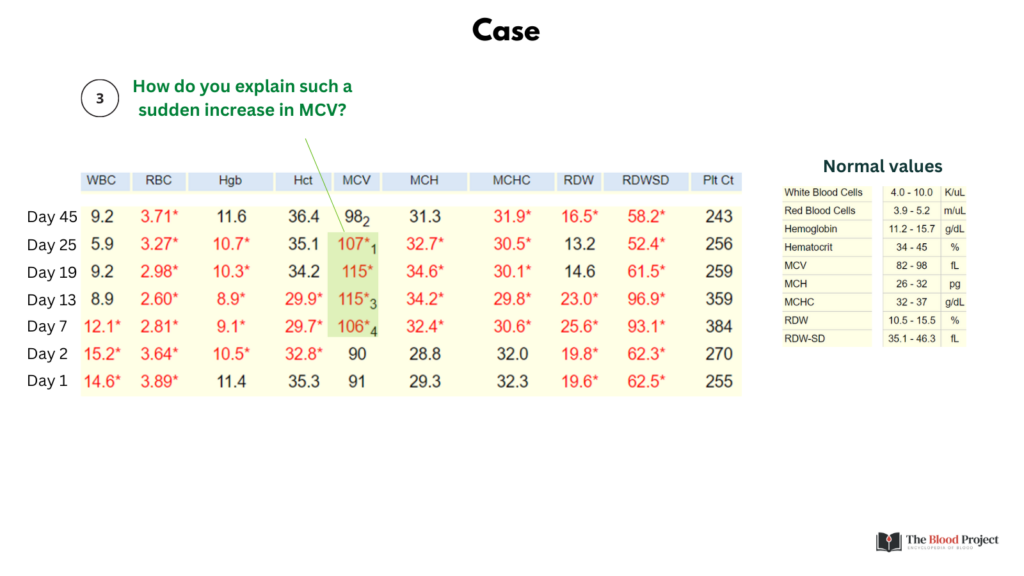
Answer 3: Any factor that changes the size of the red blood cell (RBC) at the level of the erythroid progenitor cell (for example, vitamin B12 deficiency) will take weeks to manifest an elevated MCV because of the slow turnover of the pre-existing circulating mass of normal RBCs. Rapid changes in MCV may be caused by:
- Reticulocytosis
- In vitro artifacts (spurious macrocytosis), including:
- Hyperglycemia
- Hypernatremia
- Cold agglutin disease
- Transfusion
- Liver transplant in a patient with cirrhosis-associated macrocytosis (MCV normalizes within days of transplant).
Reticulocytosis
- Reticulocytes are larger than mature RBCs, so a sudden increase in the release of reticulocytes can cause a rapid elevation in the MCV.
- Reticulocyte size follows a spectrum as the cell matures.
- The heterogeneity makes it difficult to correlate changes in reticulocyte count with changes in the MCV.
- Macrocytosis from reticulocytosis may be associated with a decrease in MCHC (larger cells but with same weight in Hb as they differentiate into mature RBCs).
- The effect of an absolute reticulocyte count on the MCV is more pronounced in patients with severe anemia because of their disproportionate representation among the total red cell population.
Causes of spurious macrocytosis have unique signatures in the hemogram:
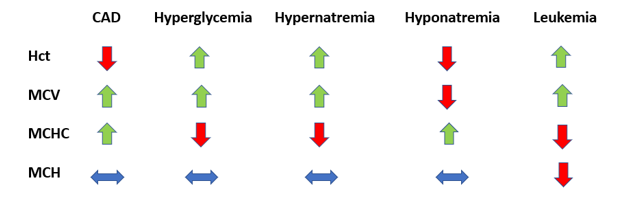
The closest profile that our case matches is the one associated with hyperglycemia/hypernatremia. However, rather than staying constant, the MCH increases, arguing against an artificial increase in blood glucose or serum sodium.
Transfusion
- Donor cells expected to have normal MCV
- If recipient has microcytosis, transfusion may lead to increase (but not normalization) of MCV (RDW should increase)
- If recipient has macrocytosis, transfusion may lead to decrease (but not normalization) of MCV (RDW should increase)
In summary, reticulocytosis appears to be the most likely explanation for the sudden increase in MCV (as we will discuss shortly [question 4], the finding of reduced MCHC supports this explanation).
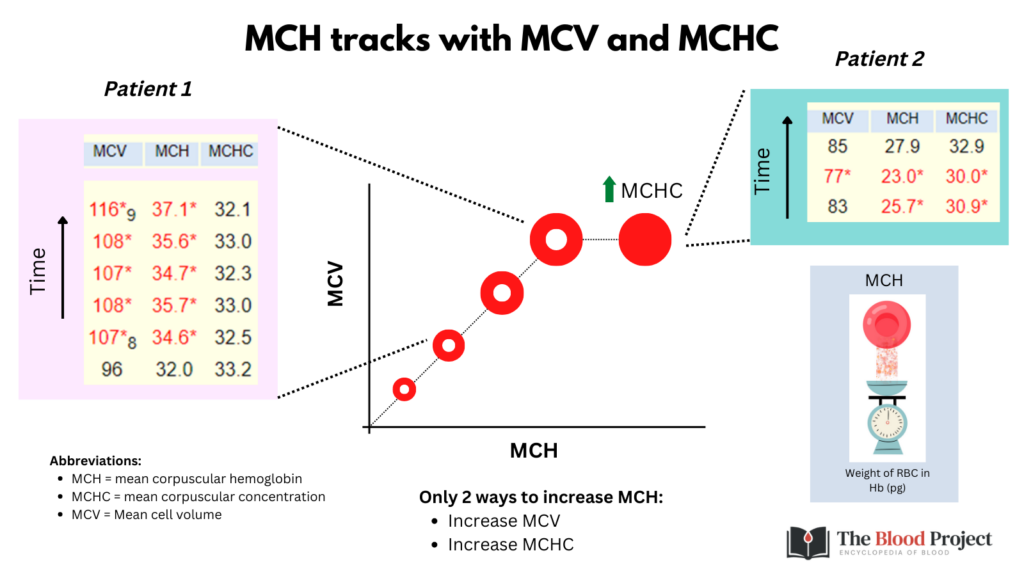
Question 4: Why does the mean corpuscular hemoglobin (MCH) increase?
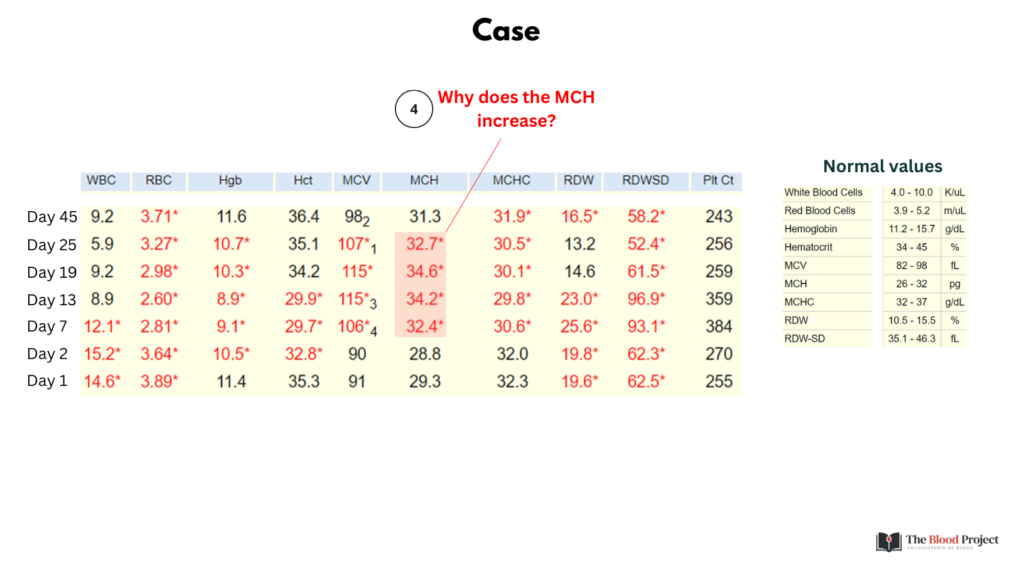
Answer 4: The MCH (the weight of red blood cell in hemoglobin) tracks with the mean cell volume (MCV) and mean corpuscular hemoglobin concentration (MCHC). In this case, the MCH increases because the MCV increases. (Important caveat: see answer to Question 5, which addresses the question of MCH change in the context of reticulocytosis).
Question 5: Why does the mean corpuscular hemoglobin concentration (MCHC) decrease?
Answer 3: This is a hint that the sudden elevation in mean cell volume (MCV) is caused by an elevated reticulocyte count. As reticulocytes mature, their volume decreases, but their total weight in Hb does not change. Thus, the MCHC in reticulocytes is low relative to that of the mature RBC.
Note: Assuming that the hemoglobin content (weight) in reticulocytes does not change as the cell matures to a red blood cells, then the MCH should not change when the number of reticulocytes is increased. However, in our experience, the MCH often increases in this setting (as it did in this case). For example, the following is a CBC time series from a patient with hemolytic anemia. Note that similar to our case, the MCH increases as the reticulocyte count increases:
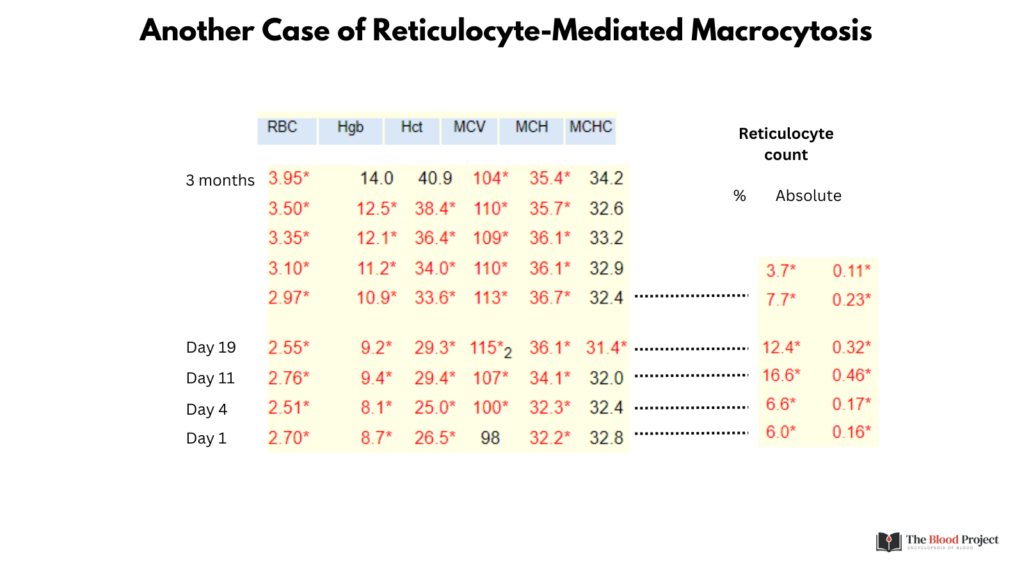
The reason for this increase in MCH is not clear.
Back to our case.
Question 6: Why is the RDW-CV (labeled “RDW” in CBC below) normal on days 19 and 25 while the RDW-SD is elevated (> 46 fL)?
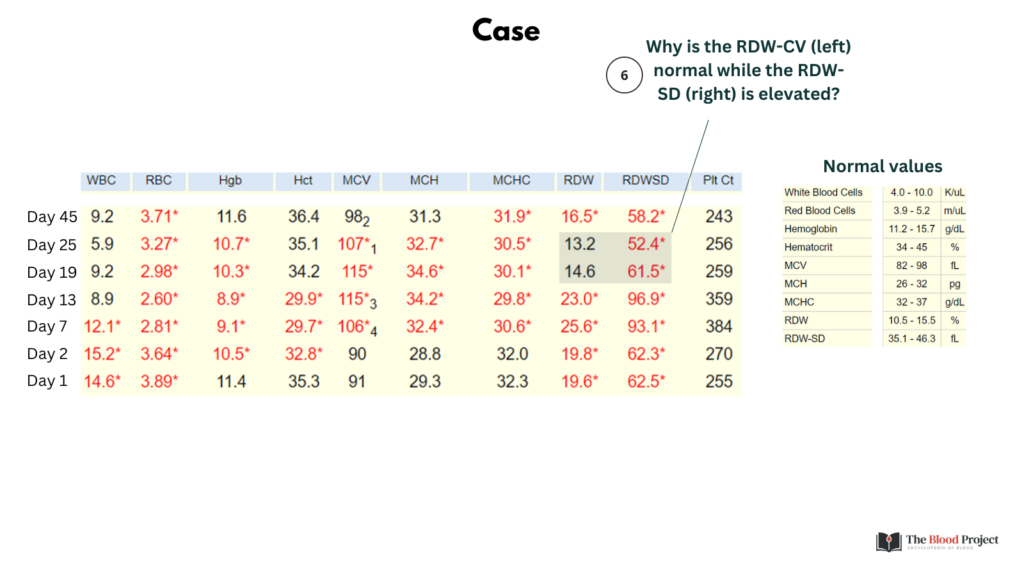
Answer 6: Because the RDW-CV is inversely correlated with the MCV, while the RDW-SD is not affected by the MCV. That is one reason why the RDW-SD is preferred over the RDW-CV.
So, putting it altogether:
- New onset macrocytic anemia
- Ddx = spurious vs. reticulocytosis
- Concomitant reduction in MCHC favors reticulocytosis
- The reticulocytosis results in widening of the RDW, as measured by RDW-SD
Case summary detailed on next slide.
56 yo M with G6PD deficiency who presented with hemolytic flare (fatigue, back pain, jaundice, dark urine) following ingestion of dapsone. The patient was treated conservatively and the hemolytic episode resolved without complications.

