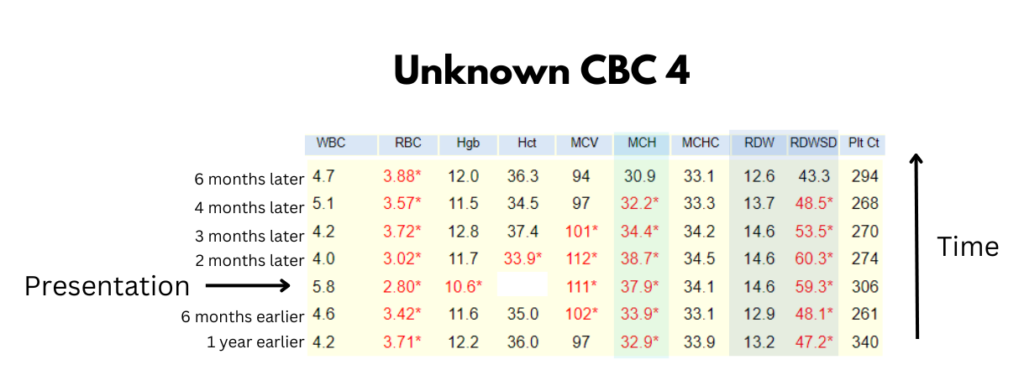
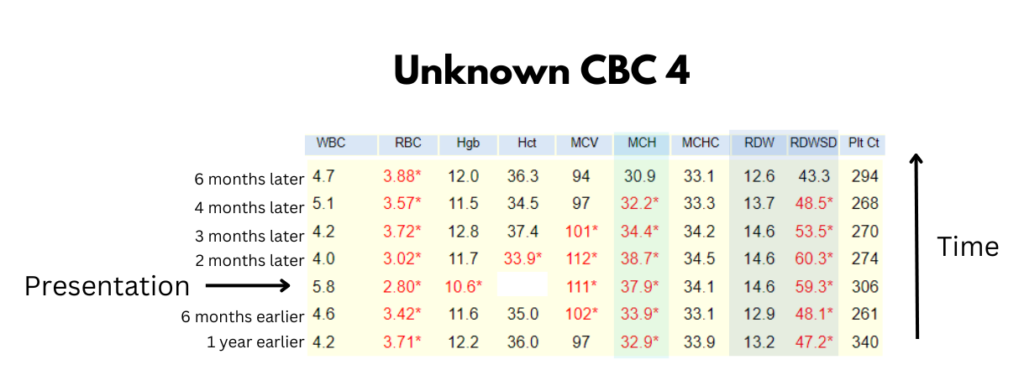
Unknown CBC 4
This case is centered around the following tweet:
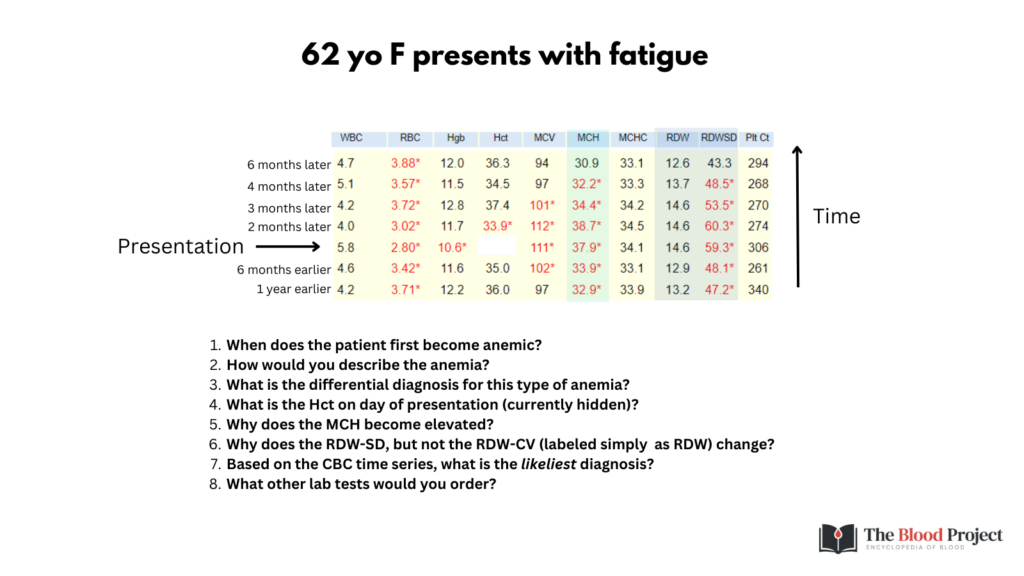
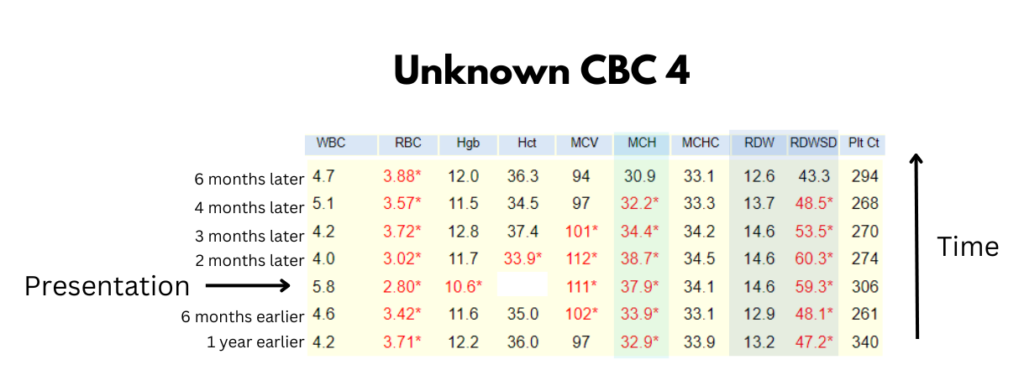
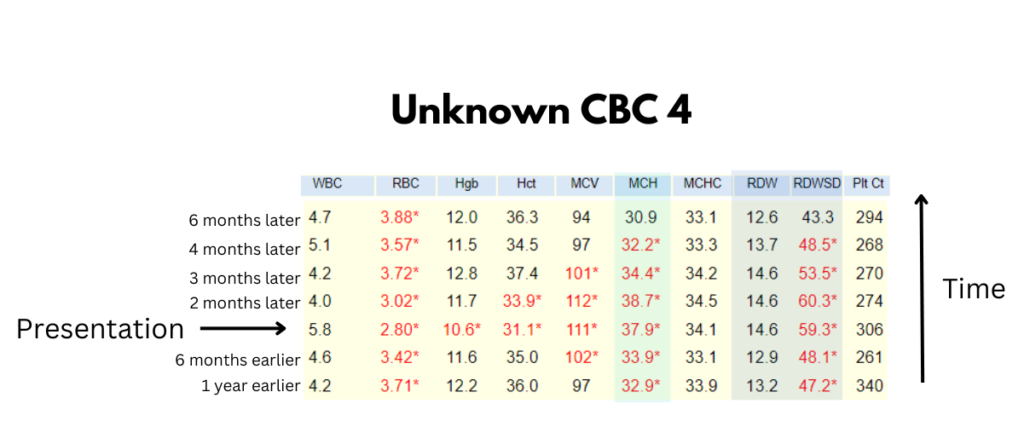
Question 1: When does the patient first become anemic?
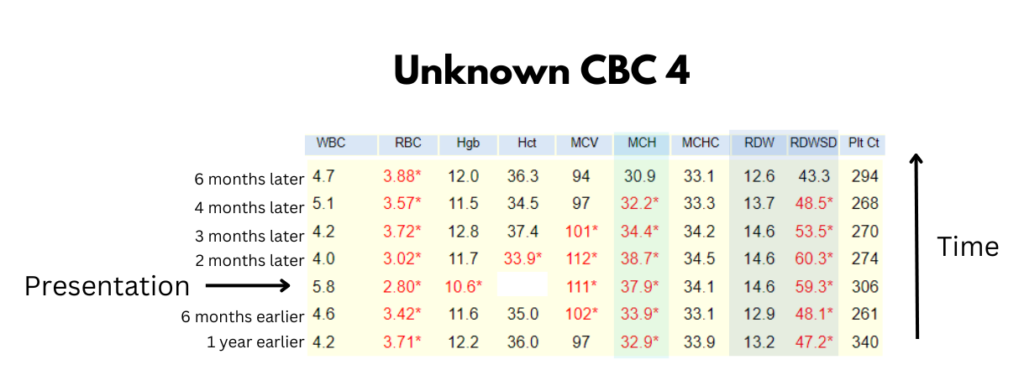
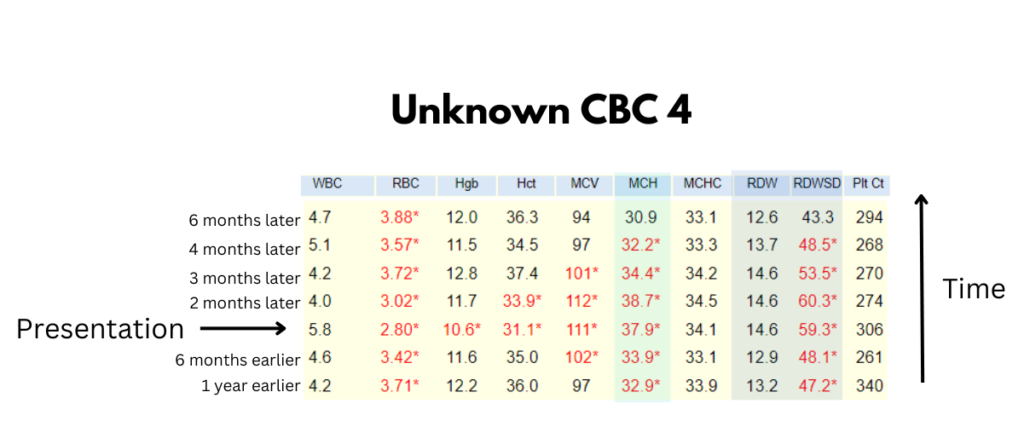
Despite proposals for new lower limits of normal Hb values based on ethnicity, gender, and age, current-day definitions of anemia are still based on a World Health Organization (WHO) report from 1968. Our patient is female, so anemia is defined as Hb <12 g/dL.
Let’s return to the CBC:
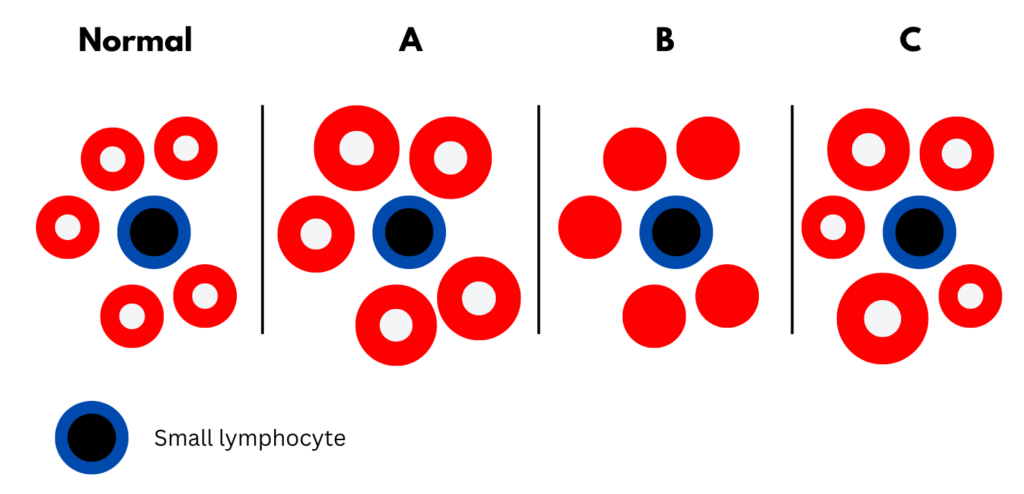
Which of the following schematic of peripheral blood smear best fits the patient?
Question 2: How would you describe the anemia?
In this case, the reticulocyte count was inappropriately low.
Question 3: What is the differential diagnosis for this type of anemia?
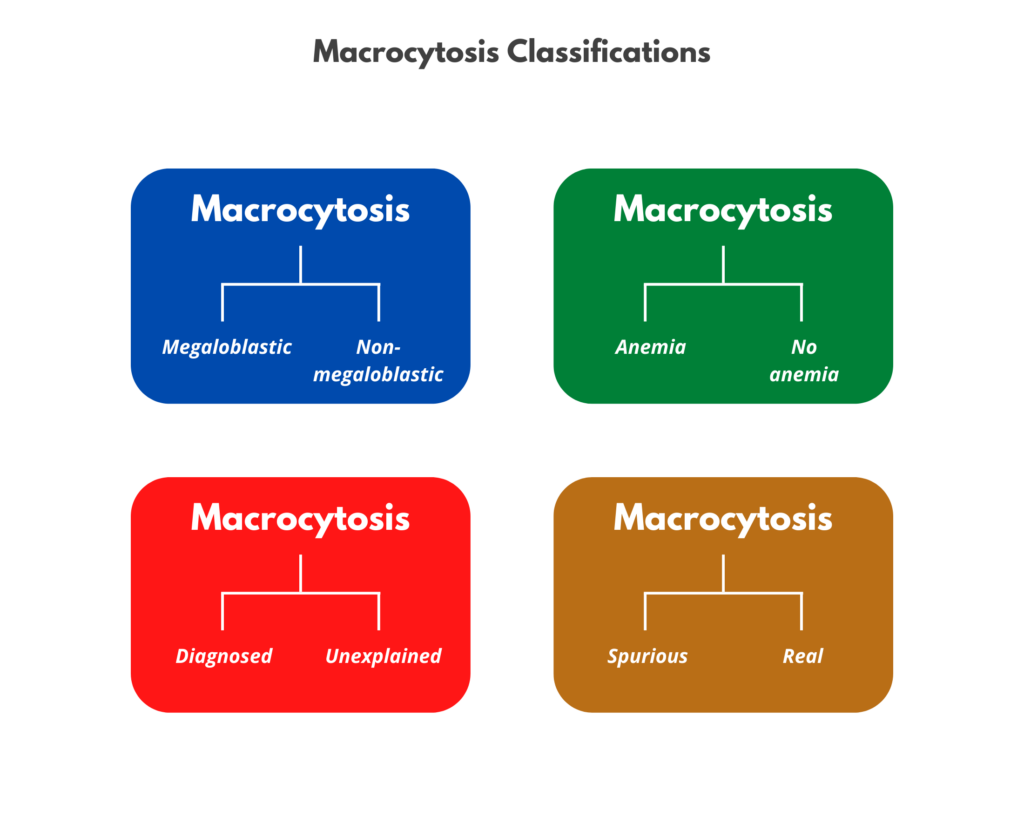
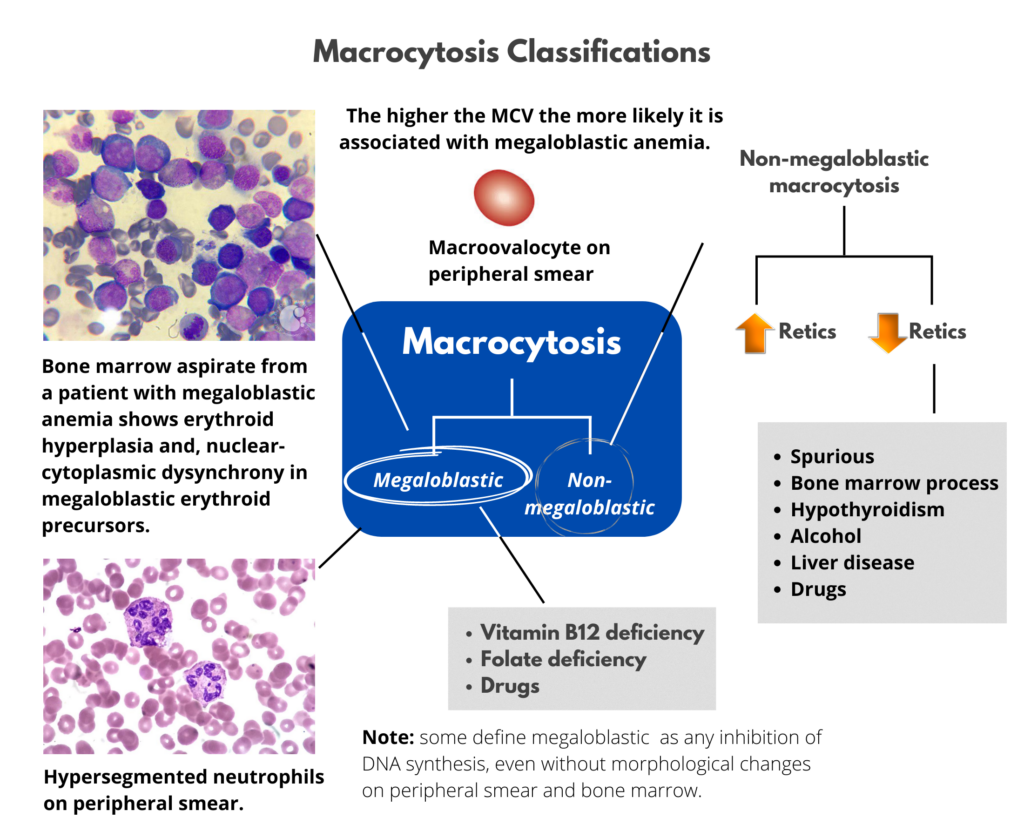
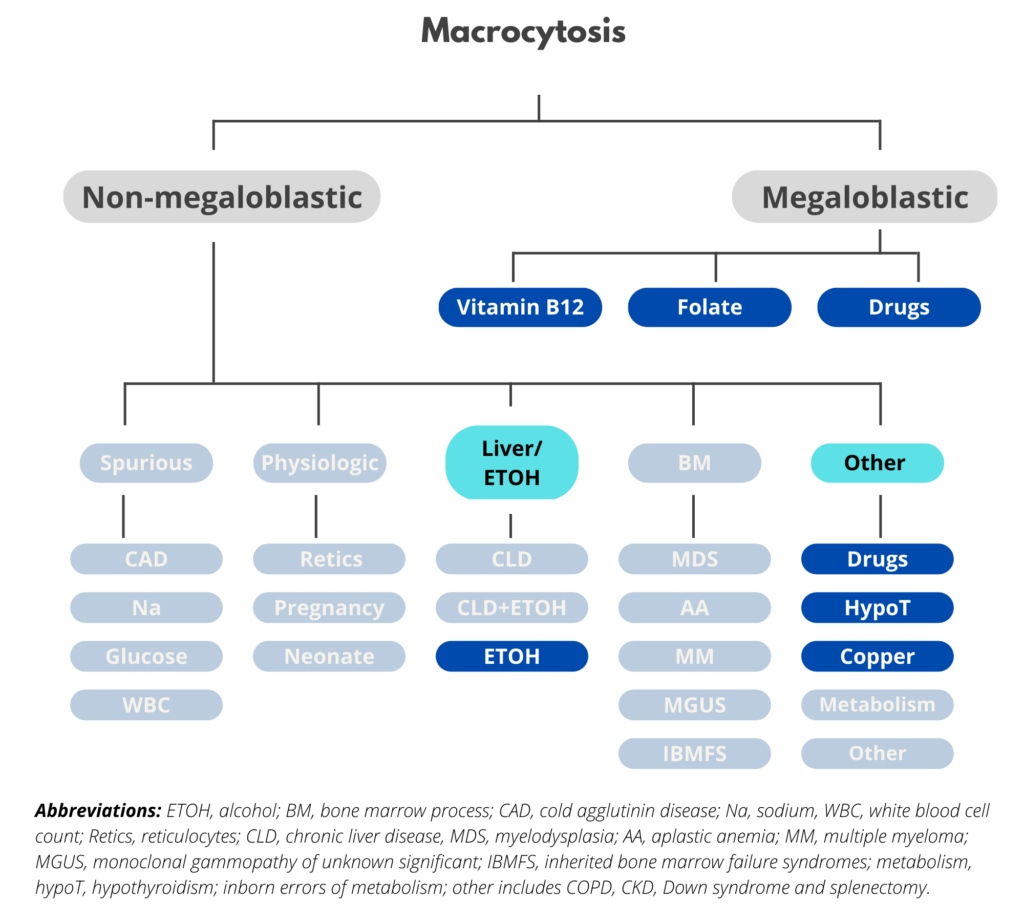
The differential diagnosis for macrocytic anemia is outlined in the following schematic:

On the previous slide, macrocytosis was categorized according to whether the condition is megaloblastic or non-megaloblastic. There are other ways to categorize macrocytosis:


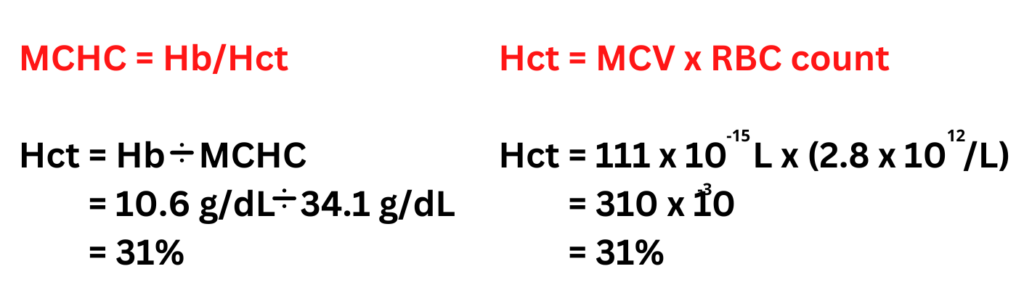
Question 4: What is the Hct on day of presentation (currently hidden)?
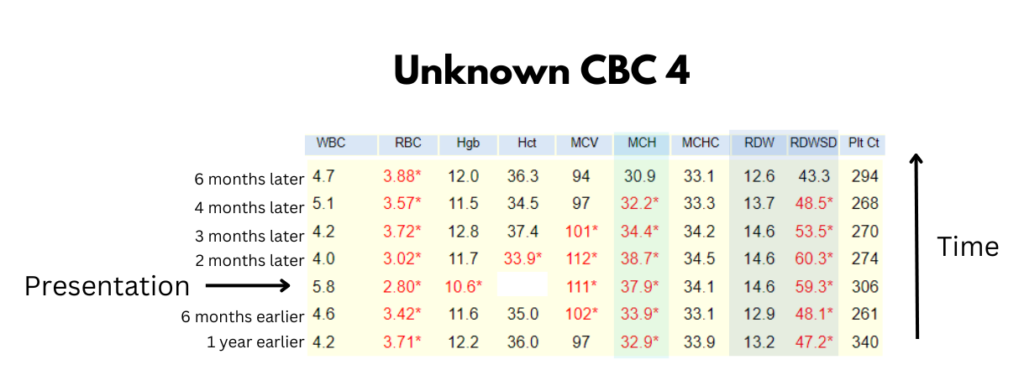
Question 4: What is the Hct on day of presentation (currently hidden)?

Question 5: Why does the MCH become elevated?
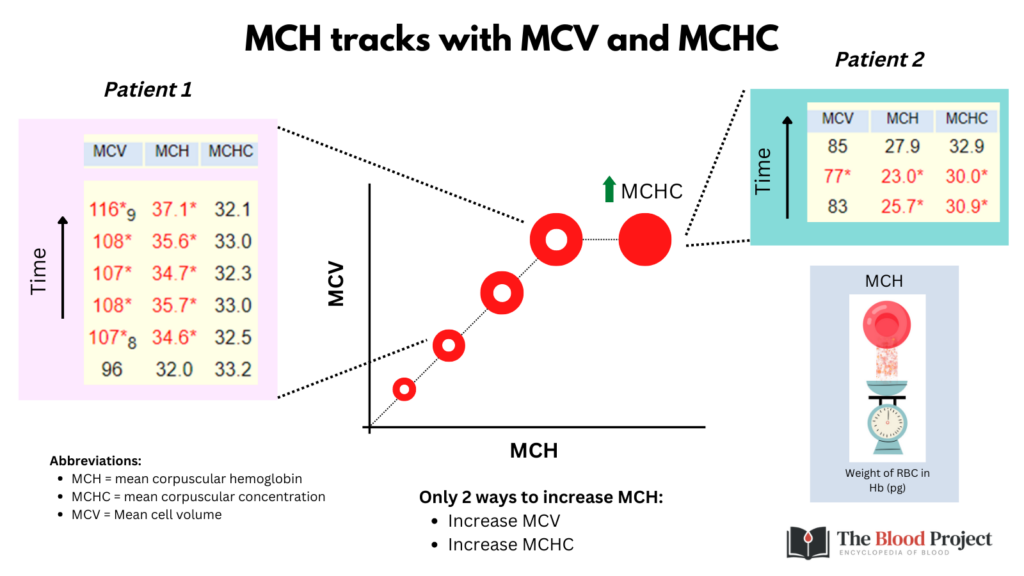
The MCH adds little to the rest of the CBC and can for all intents and purposes be ignored!
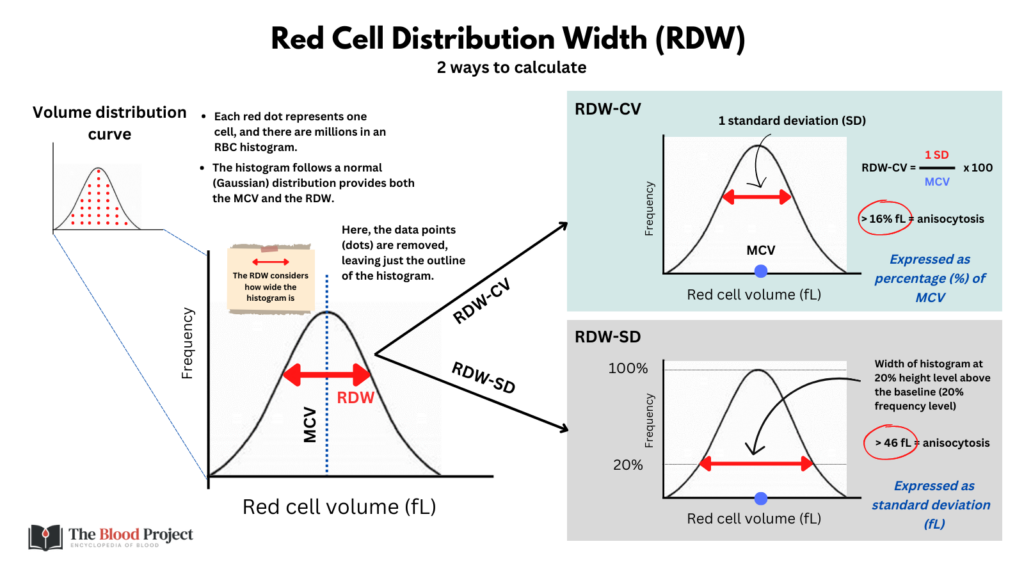
Question 6: Why does the RDW-SD, but not the RDW-CV (labeled simply as RDW) change?
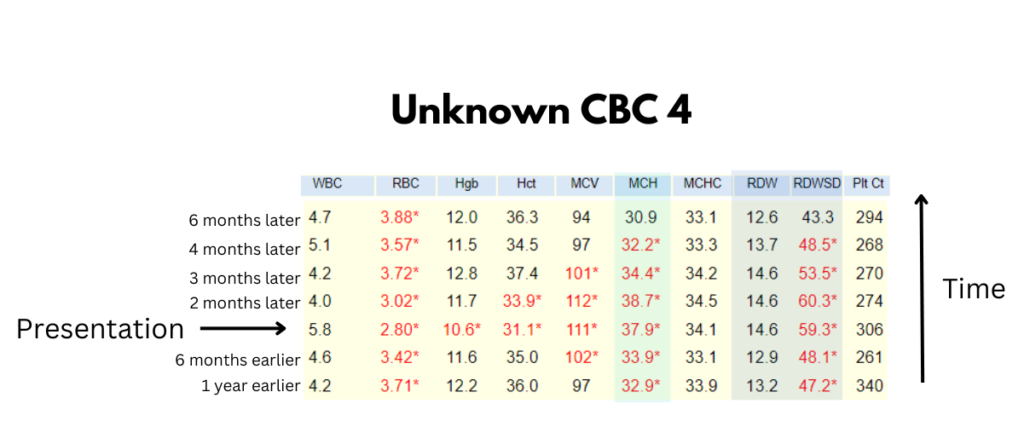
Question 7: Based on the CBC time series, what is the likeliest diagnosis?
| Cause | Comment |
|---|---|
| Spurious | Would expect macrocytosis to more transient. |
| Reticulocytosis | As discussed, this patient’s reticulocyte count was low. |
| Pregnancy | Macrocytosis would not persist for this long. |
| Neonate | Macrocytosis would not persist for this long. |
| Chronic liver disease | Would not expect correction of macrocytosis. |
| Alcohol | Possible, depending on how much and when. |
| Primary bone marrow process | Would not expect such rapid normalization of MCV. |
| Inborn errors of metabolism | Would not expect normal MCV prior to and following macrocytosis. |
| Drugs (non-megaloblastic, e.g., hydroxyurea) | Possible |
| Hypothyroidism | Possible, presuming it was treated. |
| Copper | Cannot formally exclude but rare. |
| Vitamin B12 | Possible |
| Folate | Possible, but rare in era of food fortification. |
| Drugs (megaloblastic) | Possible |
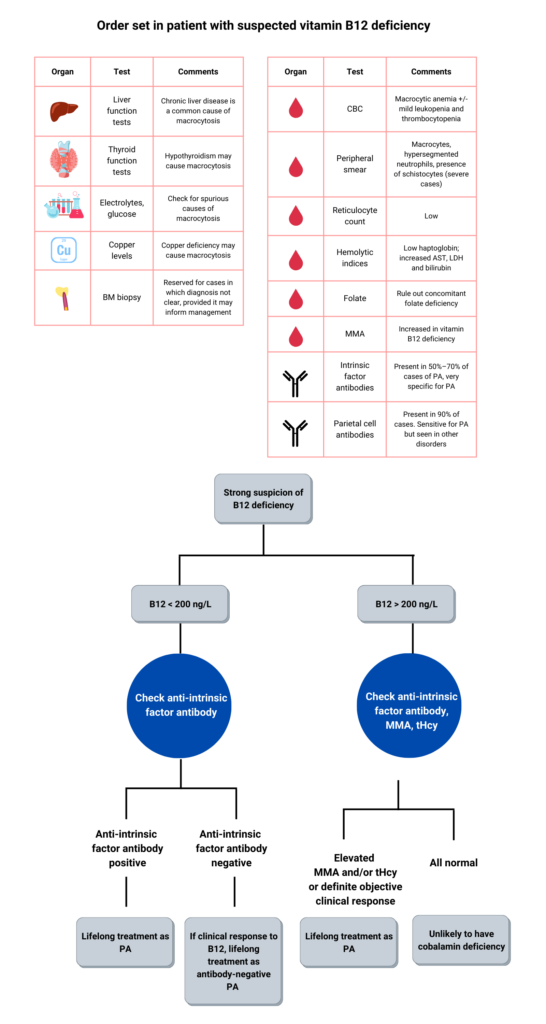
Question 8: What other lab tests would you order?
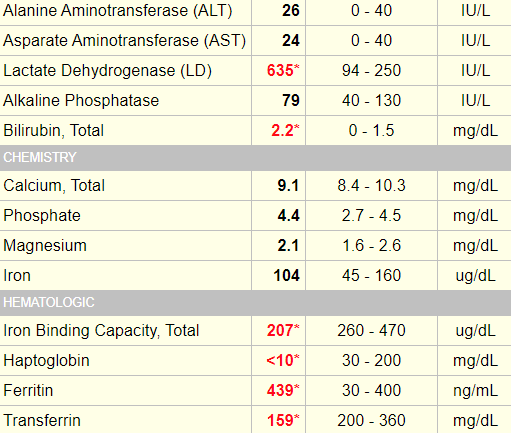
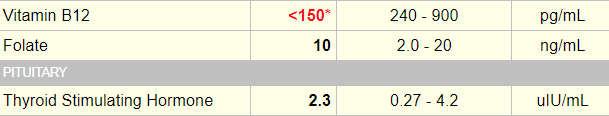
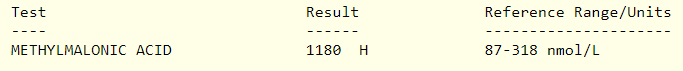
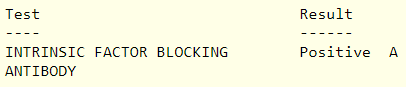
The following are the relevant labs from this patient:
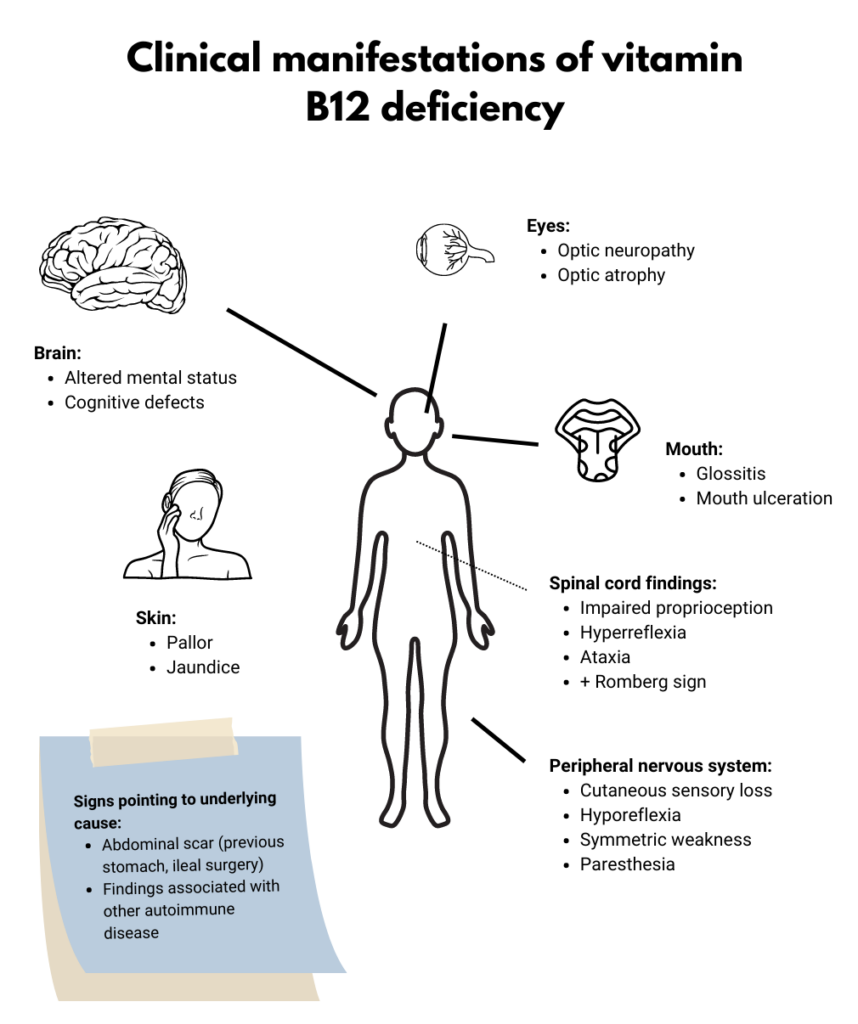
This was a 62 yo F who presented with a several month history of fatigue. She denied any other symptoms and her physical exam was negative for the findings outlined below. She was diagnosed with pernicious anemia and received vitamin B12 1000 mcg IM weekly for 6 weeks, followed by monthly injections at the same dose.
Let’s look at another case of vitamin B12 deficiency:

Description/definition:
Pernicious anemia is an autoimmune disorder characterized by antibody-mediated destruction of parietal cells in the stomach, leading to atrophic gastritis and reduced production of intrinsic factor, important for vitamin B12 absorption by the terminal ileum.
It is the most common cause of vitamin B12 deficiency and is present in up to 2% of persons over 60 years of age in the United States.
Pernicious anemia is associated with:
- Other autoimmune diseases
- Iron deficiency anemia
- An increased risk of stomach cancer.
The terms vitamin B12 and cobalamin are generally used interchangeably.

Pathophysiology:
- Vitamin B12 absorption:
- Vitamin B12 is a water-soluble vitamin.
- Vitamin B12 is obtained from dietary sources (restricted to food of animal origin) including meat, eggs, and dairy products.
- 50%-60% of consumed vitamin B12 is absorbed.
- Absorption depends on an acid pH and on binding of vitamin B12 to intrinsic factor, produced in the parietal cells of the stomach.
- 1%-5% of free vitamin B12 is absorbed passively without the need for intrinsic factor (this is the rationale for providing oral vitamin B12 as therapy).
- Vitamin B12 function:
- vitamin B12 is a cofactor for only 2 enzymes:
- Methionine synthase, which converts homocysteine to methionine.
- Mitochondrial enzyme L-methylmalonyl-coenzyme A mutase, which catalyzes the conversion of L-methylmalonylCoA (remnant of odd-numbered fatty acids) to succinylCoA.
- Vitamin B12 is necessary for:
- DNA and RNA synthesis, important for rapidly dividing cells such as those of the hematopoietic system.
- Myelination of the central nervous system.
- vitamin B12 is a cofactor for only 2 enzymes:
- Pathogenesis of pernicious anemia:
- Autoimmune destruction of parietal cells in the stomach.
- Anti-parietal cell antibodies target the gastric enzyme H+/K+ATPase proton pump in parietal cells.
- Loss of intrinsic factor leads to reduced vitamin B12 absorption in the terminal ileum.

Diagnosis:
Suspect diagnosis of pernicious anemia in a patient with:
- Macrocytic anemia
- Neurological findings suggesting demyelination
- Low vitamin B12 levels (standard cutoff <200 ng/L)
- Elevated methylmalonic acid levels
Confirm diagnosis:
- Presence of anti-intrinsic factor
- Biopsy consistent with atrophic gastritis (not necessary for diagnosis)
Other labs that may be helpful in a patient with vitamin B12 deficiency:
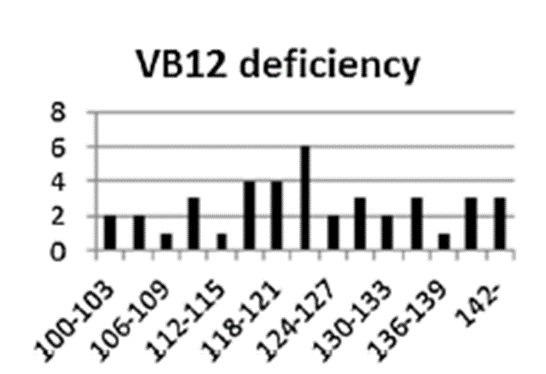
- Complete blood count showing additional cytopenias; in one study of 201 patients with documented vitamin B12 deficiency, frequency of cytopenias was:
- Anemia in 37%
- Leukopenia in 13.9%
- Thrombocytopenia in 9.9%
- Pancytopenia in 5%
- Hypersegmented neutrophils in 32%
- Peripheral smear, showing presence of:
- Macro-ovalocytes
- Fragmented red cells (in severe cases)
- Hypersegmented neutrophils
- Low reticulocyte count
- Serum folate to rule out folate deficiency
- Hemolytic indices (positive from ineffective erythropoiesis):
- Low Haptoglobin
- Elevated LDH (often out of proportion to other markers)
- Elevated indirect bilirubin
- Elevated AST
Diagnosis of atrophic gastritis
- Anti-parietal cell antibodies
- Gastric mucosa biopsy
Notes:
- Macrocytosis reported to be absent in about 30% of patients with pernicious anemia.
- Some patients with pernicious anemia may present with non-anemic macrocytosis for several months prior to diagnosis.
- Neurological symptoms may occur, even in absence of macrocytosis or anemia.
- The higher the MCV the greater the pre-test probability that the macrocytosis is caused by B12 (+/- folate) deficiency.

Treatment:
Replace vitamin B12:
- Vitamin B12 may be given by the following routes:
- Oral
- Sublingual
- Intranasal
- Intramuscular
- Deep subcutaneous
Dosing protocols:
- Highly variable
- Typical dosing schedule for intramuscular cyanocobalamin for replacement therapy is 1,000 mcg/day or every other day for 1 week, then weekly for 4 weeks, and then monthly for life.
- Parenteral vitamin B12 favored for initial treatment.
- Oral vitamin B12 acceptable for maintenance therapy.
- Patients with pernicious anemia require life-long treatment with vitamin B12.
In one study, the time for MCV to return to normal with B12 therapy was 25 to 78 days.

Screening
Gastric cancer:
- Reported annual incidence of gastric cancer range from 0.1% to 0.5% among patients with pernicious anemia.
- The British Society of Gastroenterology guideline recommendations:
- We suggest that a baseline endoscopy with biopsies should be considered in individuals aged ≥50 years, with laboratory evidence of pernicious anaemia, defined by vitamin B12 deficiency and either positive gastric parietal cell or intrinsic factor antibodies. As GA affects the corpus in pernicious anaemia, biopsies should be taken from the greater and lesser curves (evidence level: low quality; grade of recommendation: weak; level of agreement: 93%).
- We recommend endoscopic surveillance every 3 years should be offered to patients diagnosed with extensive [atrophic gastritis], defined as that affecting the antrum and body (evidence level: low quality; grade of recommendation: strong; level of agreement: 100%).
| Reference | Comment |
|---|---|
| Review articles | |
| Nat Rev Dis Primers. 2020;6:56 | A review on autoimmune gastritis |
| Arch Pathol Lab Med. 2019;143:1327-1331 | Another review on autoimmune Gastritis |
| Autoimmun Rev. 2014;13:565-8 | Diagnosis and classification of pernicious anemia |
| Clinical practice guidelines | |
| BCSH guidelines for Guideline for the diagnosis and British Committee for Standards in Haematology. Guidelines for the diagnosis and treatment of cobalamin and folate disorders | Published in 2014 |
| AGA Clinical Practice Update on the Diagnosis and Management of Atrophic Gastritis: Expert Review | Published in 2021 |
| Online evidence-based resources | |
| DynaMed | A rigorous evidence-based point-of-care tool, can access overview and recommendations section without subscription |
| UpToDate | Relies heavily on expert opinion. Not accessible without subscription |