Unknown CBC 5
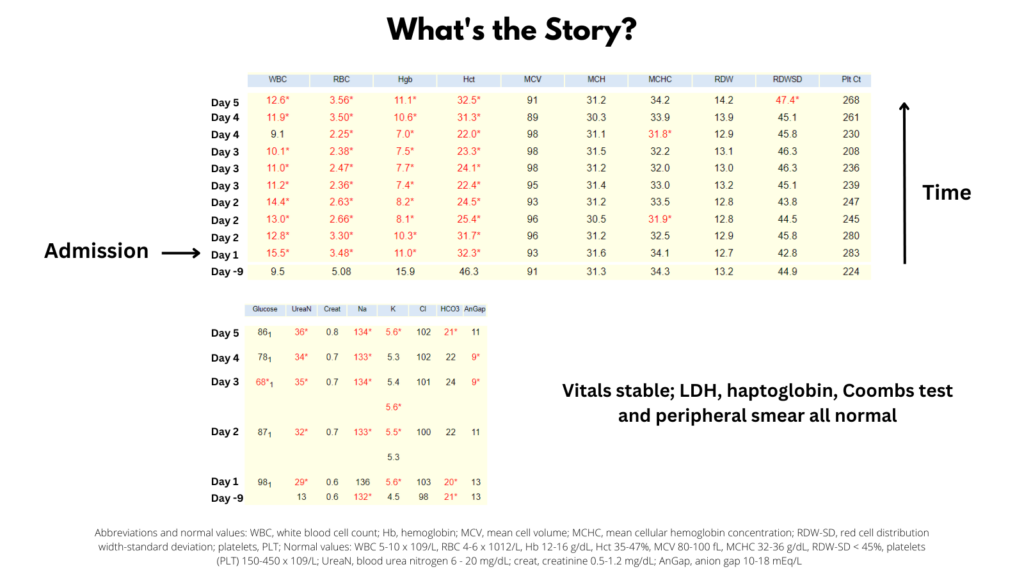
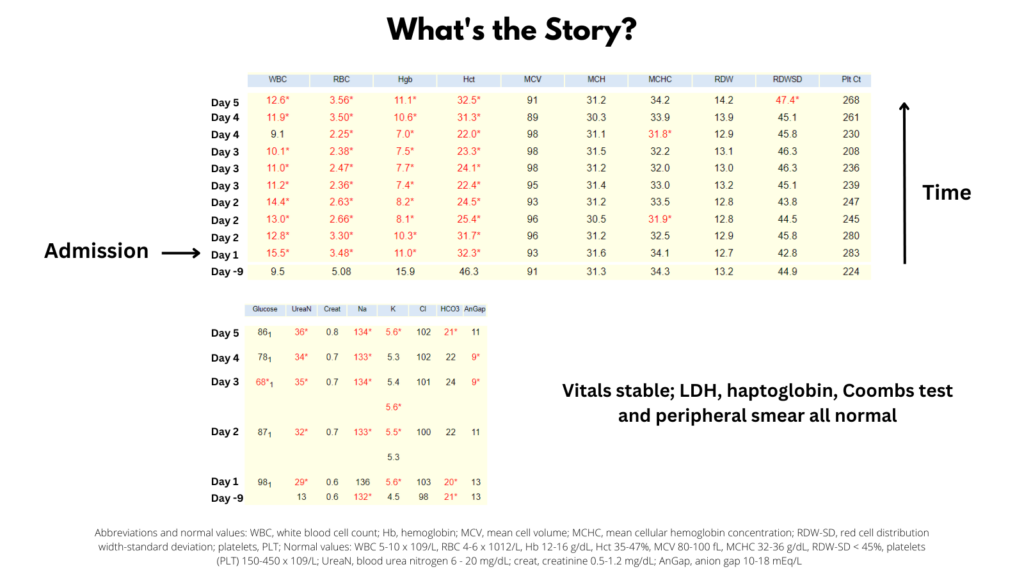
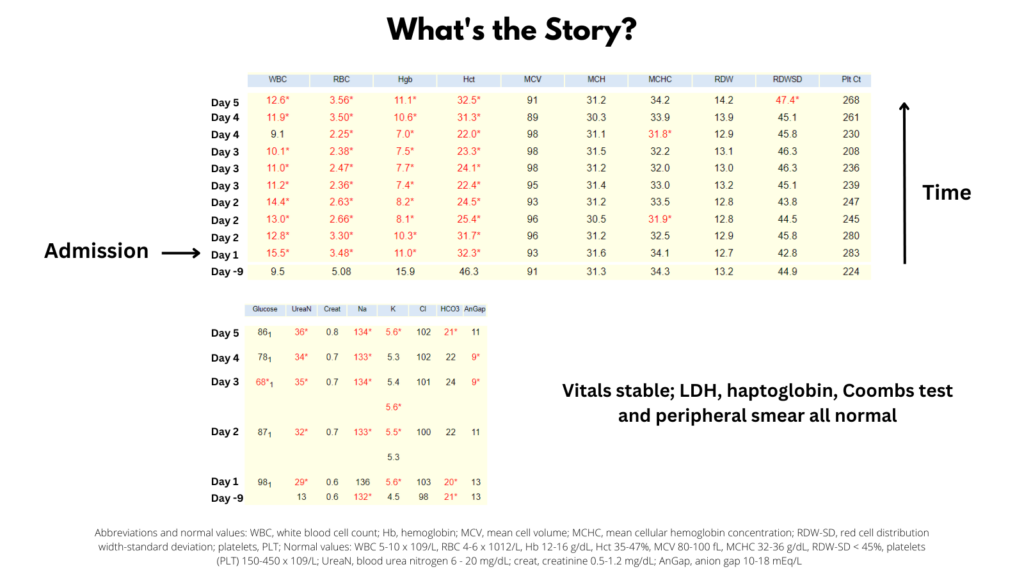
9 days prior to admission, the Hb was 15.9 g/dL. If we assume a complete arrest of erythropoiesis (yet normal red blood cell survival of 120 days), what would you predict the Hb to be on day of admission?
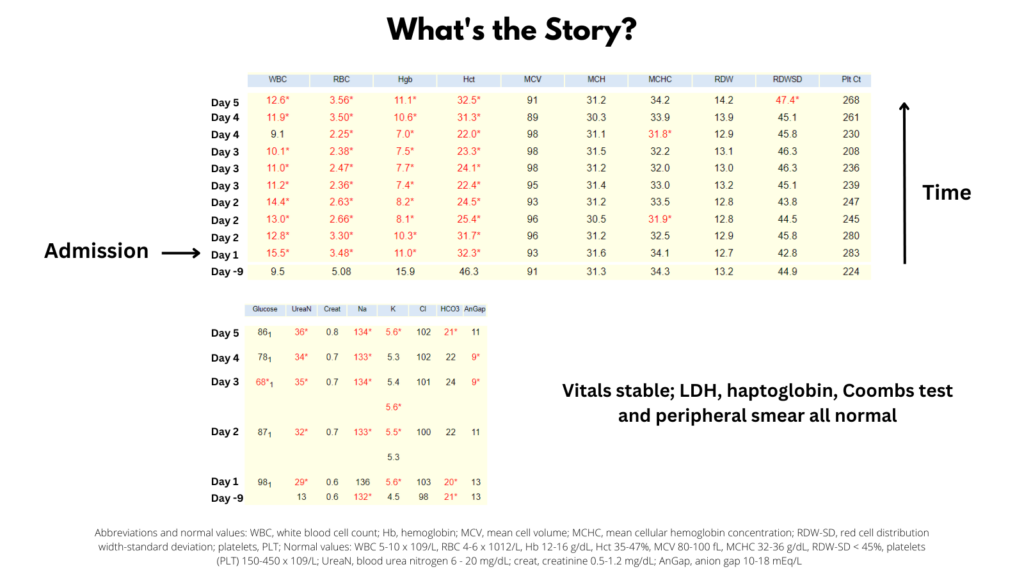
So, even with complete absence of red blood cell production (say from parvovirus B19), the numbers do not add up. There has to be more than a production problem (in other words, factors such as iron deficiency, vitamin B12 deficiency, and inflammatory block cannot by themselves explain the patient’s anemia).

What 2 processes might explain the drop in Hb (which continues during hospitalization)?
Click for Answer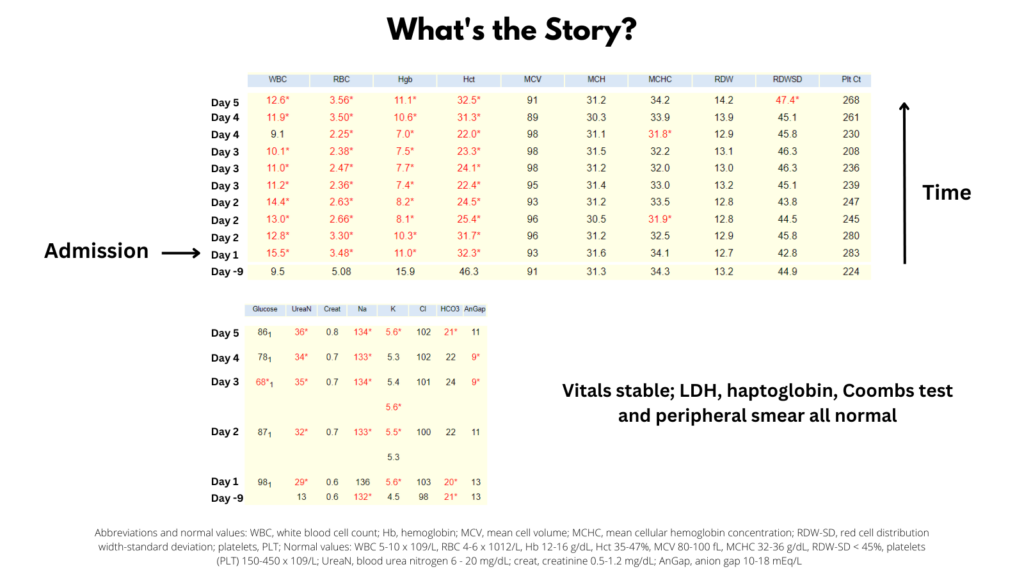
Would a reticulocyte count help differentiate between hemolysis and blood loss?
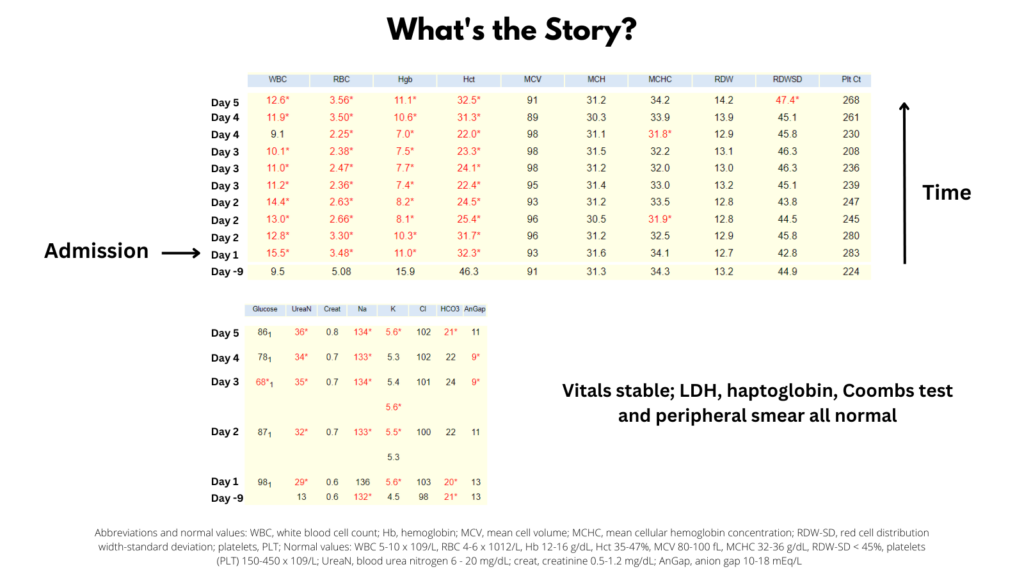
We are provided with the information that the LDH, haptoglobin and peripheral smear are normal. That takes hemolysis off the table and leaves bleeding as the most likely cause. What is the most likely source of blood loss:
If the patient has GI blood loss, it might be upper (proximal to the ligament of Treitz) or lower (distal to the ligament of Treitz). Which is most likely and why?
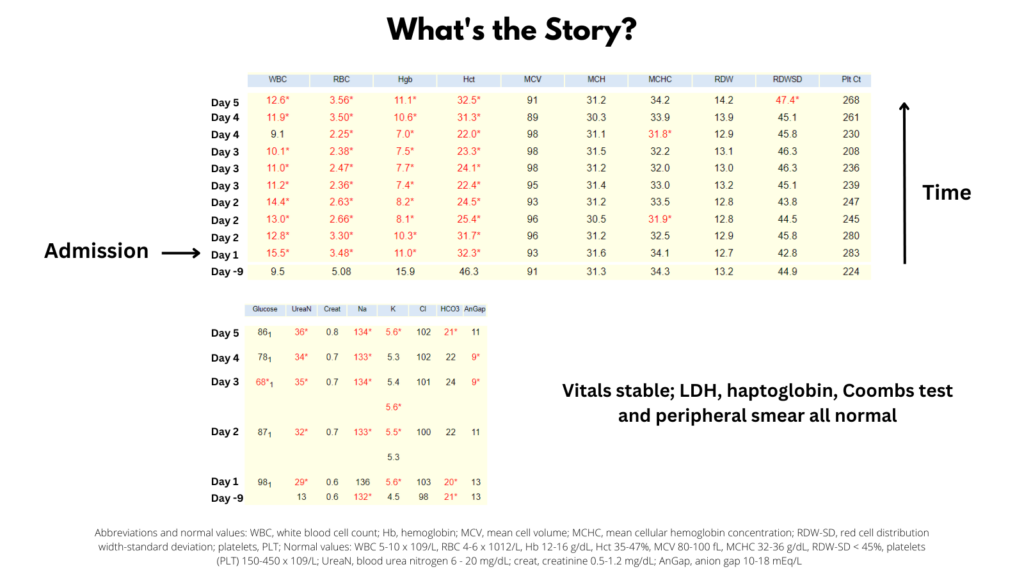
What about the leukocytosis? How would you explain it?
Summary of Case:
This was a 58 year-old man who presented to the ED on the day of admission complaining of fatigue and melena. He denied any hematemesis. There was no history of previous GI bleed. His other medical problems included hypertension and hyperlipidemia. He was taking lisinopril and atorvastatin. He had no known allergies. Vitals showed tachycardia, but no postural change in blood pressure. Abdominal exam was unremarkable. His CBC revealed leukocytosis and normocytic anemia. His BUN was elevated. His liver function tests were normal (not shown). He underwent upper endoscopy the day following admission. This showed a bleeding peptic ulcer for which he underwent primary endoscopic hemostasis. He was transfused 2 units of packed red blood cells on day 4. He was discharged on day 10 without evidence of further bleeding.
