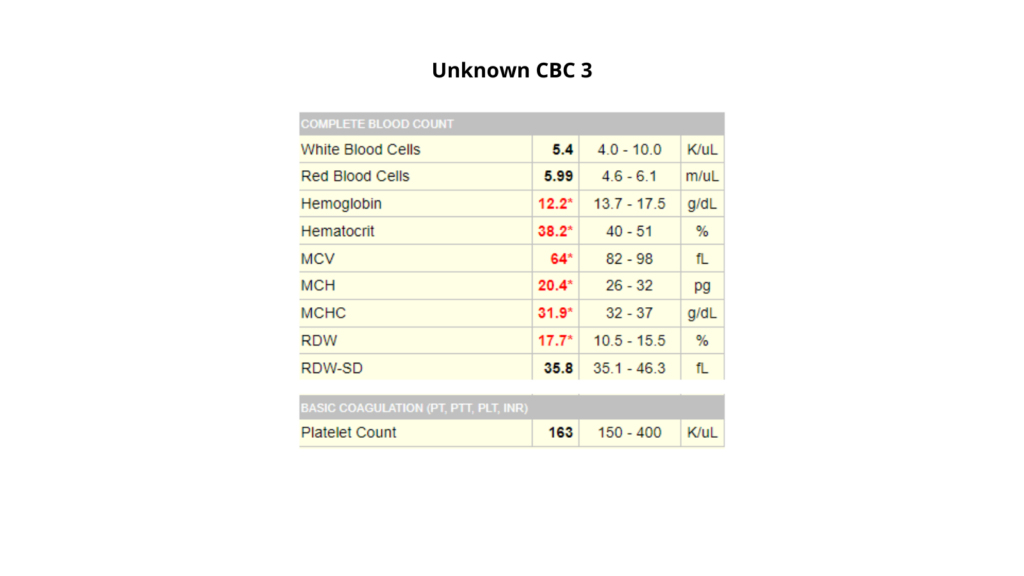
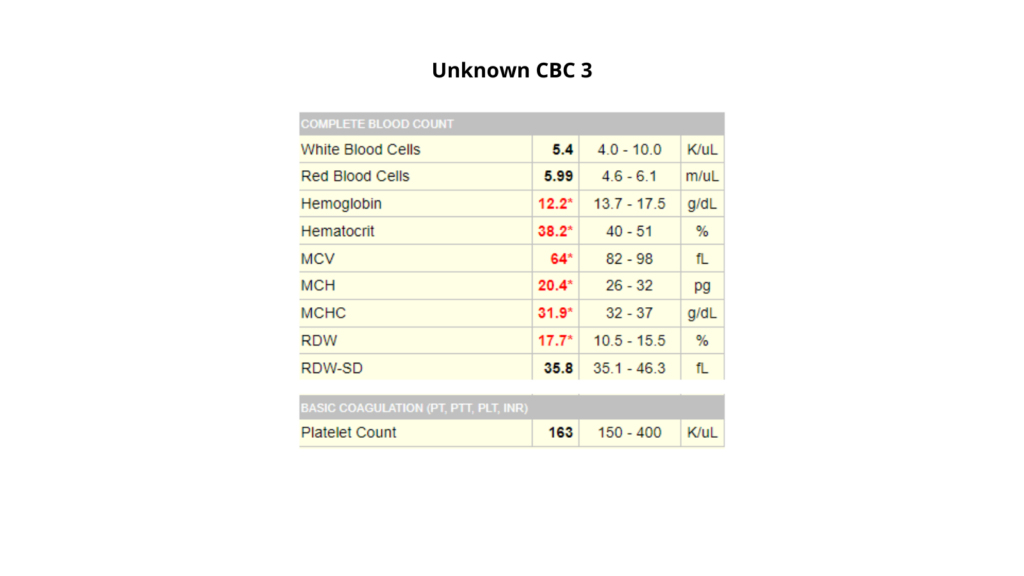
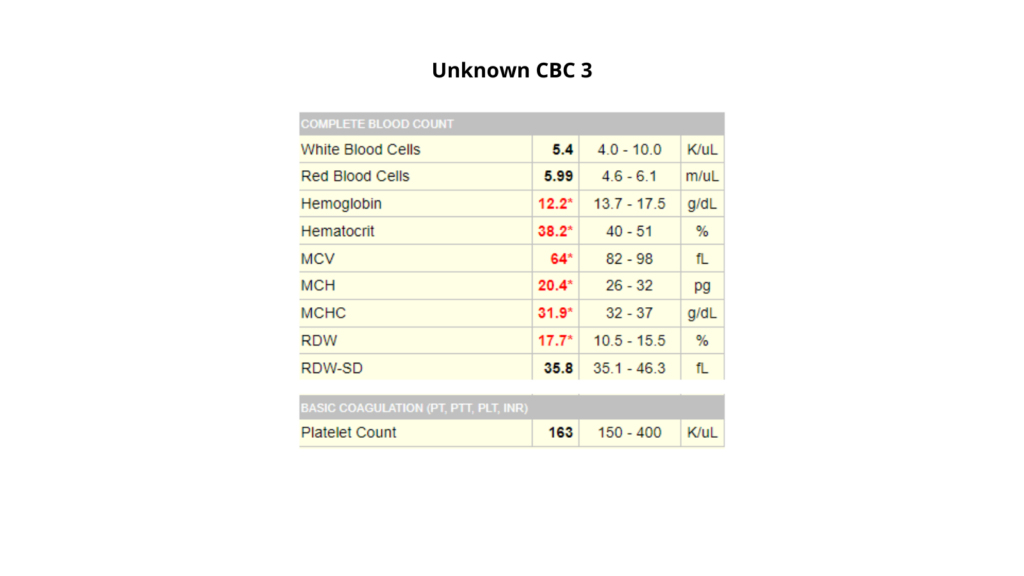
Unknown CBC 3
This case is centered around the following twitter thread:
- QUESTIONS:
- How would you describe the complete blood count (CBC)?
- What is the differential diagnosis?
- What is the most likely diagnosis?
- Why is the RDW-CV (labeled RDW) increased, but not the RDW-SD?
Question 1: How would you describe the complete blood count (CBC)?
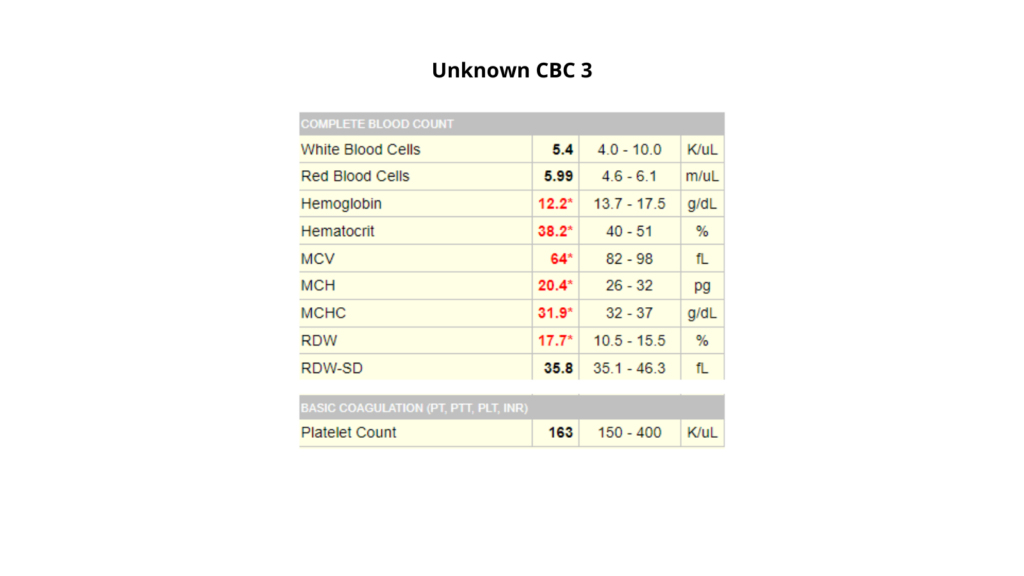
- If male, microcytic anemia
- If female, isolated microcytosis
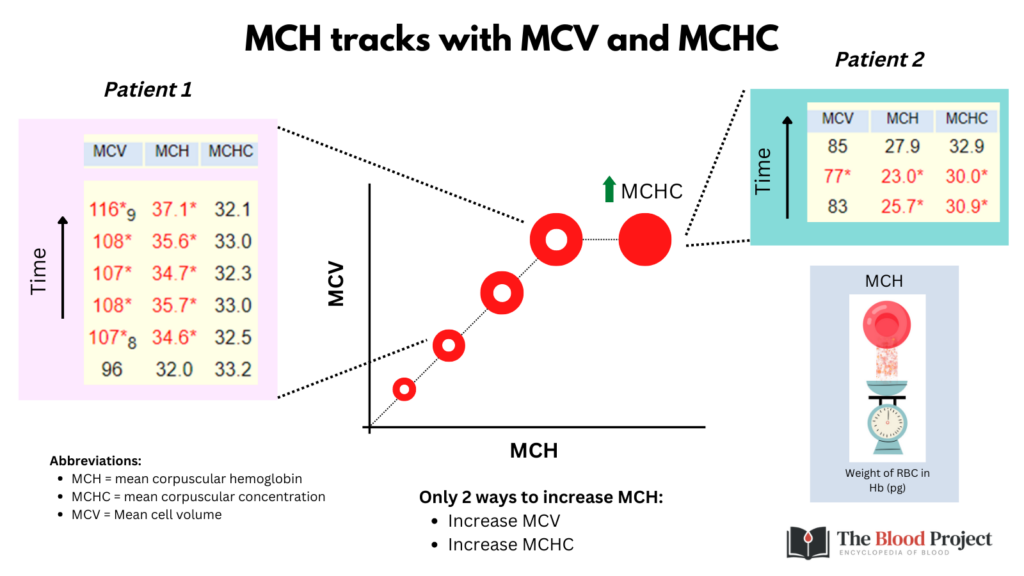
The MCH adds little to the rest of the CBC and can for all intents and purposes be ignored!
Let’s return to the CBC:
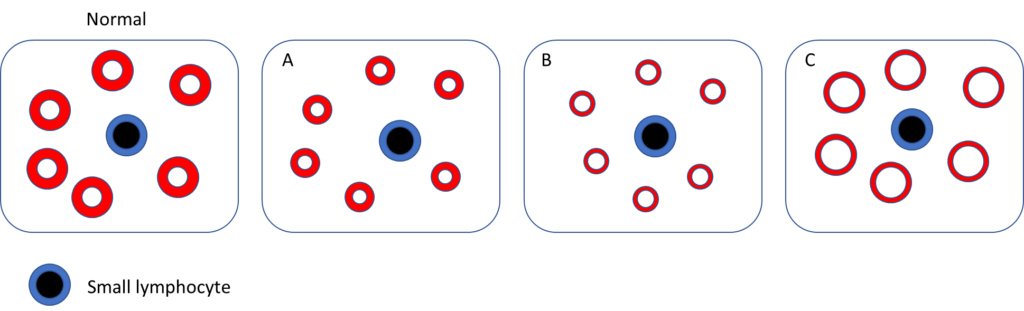
Which of the following schematic of peripheral blood smear best fits the patient?
Question 2: What is the differential diagnosis?
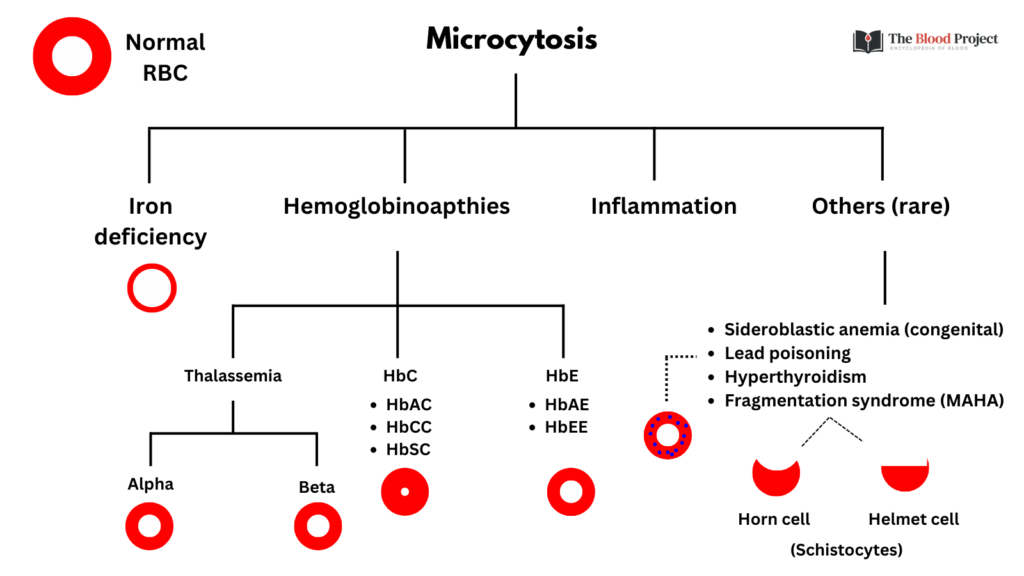
About 10-20% of patients with anemia of inflammation have microcytic, hypochromic indices. However, the mean cell volume is almost always > 70 fL. Thus, even without any other information about our patient, we can more or less rule out inflammation as the sole cause of the microcytosis. That leaves us with iron deficiency and thalassemia as the most likely possibilities.
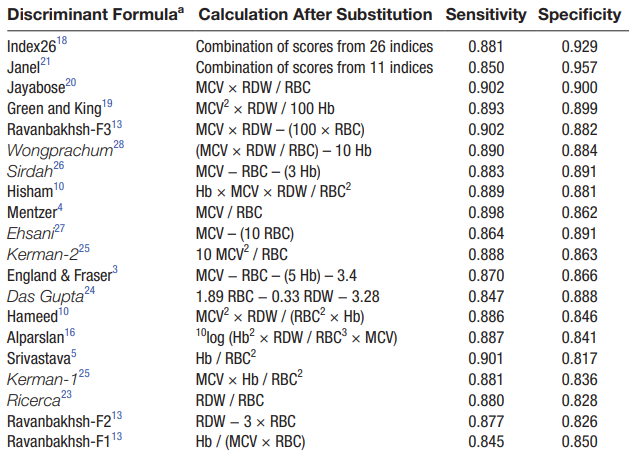
Several discriminant formulas have been published for distinguishing thalassemia from iron deficiency in patients with microcytic anemia:
Among the more popular formulas is the Mentzer index, first described in 1973. The index is very simple: MCV/RBC.
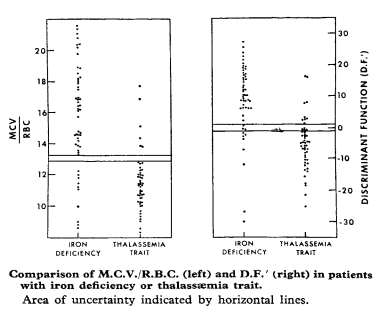
Mentzer Index > 13 indicates a greater likelihood of iron deficiency anemia diagnosis.
What is the Mentzer index really saying?
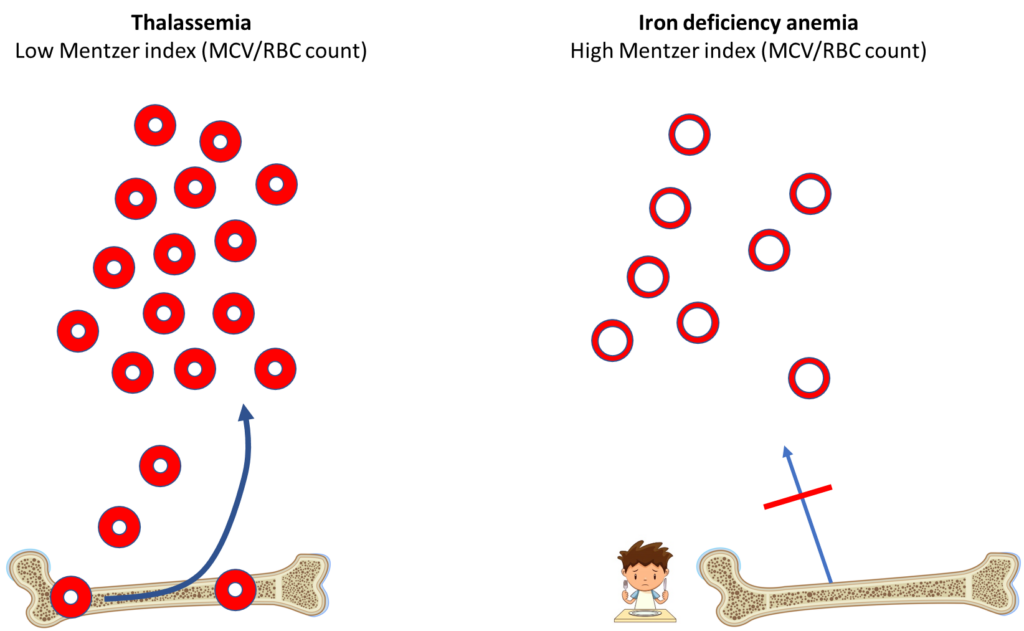
The Mentzer index reflects the fact that in iron deficiency, the loss of the essential nutrient, iron, causes a block in erythropoiesis and decreased production of red blood cells (RBCs), while in thalassemia, no such block occurs. In thalassemia, the bone marrow works overtime to compensate for the small RBC size by producing and releasing many more cells. The index also takes into consideration that the MCV tends to be lower in thalassemia.
Question 3: What is the most likely diagnosis?
- Thalassemia, based on Mentzer index (and here we are talking about thalassemia minor, since the there is no significant anemia)
- There are two types of thalassemia, depending on which gene is involved:
- Alpha thalassemia
- Beta thalassemia

In addition to alpha and beta thalassemia, what other types of hemoglobinopathy cause microcytosis?
Click for Answer| Hemoglobinopathy | Cause of microcytosis |
|---|---|
| Beta thalassemia | Globin chain imbalance (unmatched alpha chains) |
| Alpha thalassemia | Globin chain imbalance (unmatched beta chains) |
| Hb E | Cryptic mRNA splice site causing reduced synthesis of the HbE chain causing globin chain imbalance (unmatched alpha chains) |
| Hb C | Cellular dehydration |
Here are the results of the patient’s hemoglobin electrophoresis:
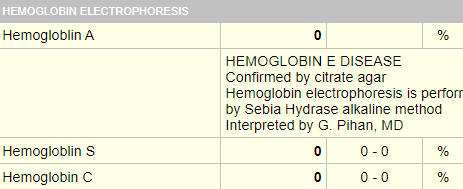
So, the patient has hemoglobin E disease (meaning he is homozygous for the HbE gene!
About Hb E
- Hemoglobin E (HbE) disorders are a group of chronic, hereditary anemias characterized by the presence of ≥ 1 HbE allele.
- Most prevalent in:
- Thailand
- Laos
- Cambodia
- Mechanism:
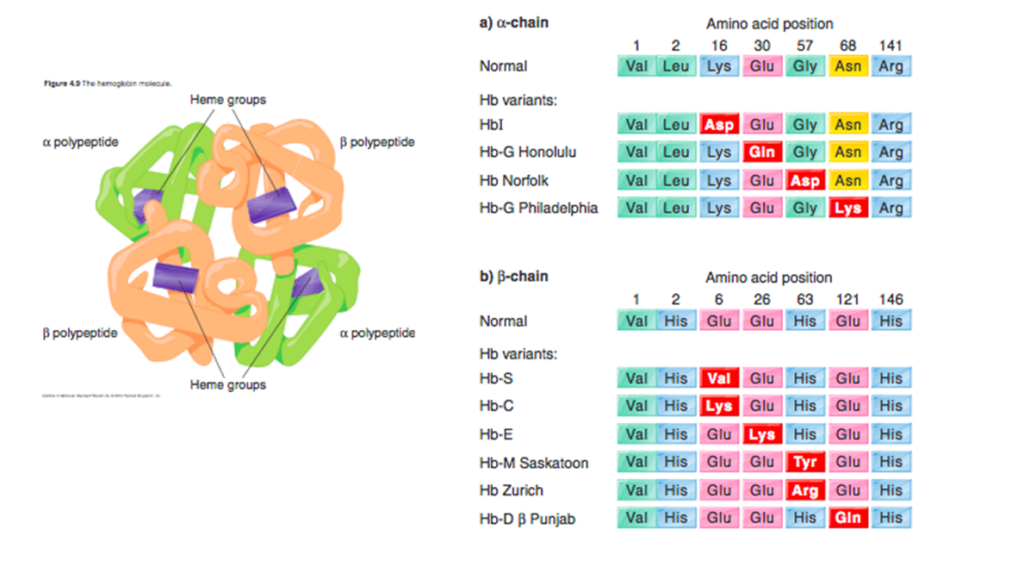
- Caused by single base mutation at codon 26 of the beta-globin gene, leading to the substitution of lysine for glutamic acid.
- The hemoglobin E (HbE) mutation activates a cryptic mRNA splice site (one that does not lead to a functional protein), resulting in reduced synthesis of the HbE chain, mild globin chain imbalance (unmatched alpha chains), and a thalassemia phenotype.
- Because synthesis of the beta chain of HbE is impaired, HbE is considered a beta+-thalassemic hemoglobinopathy
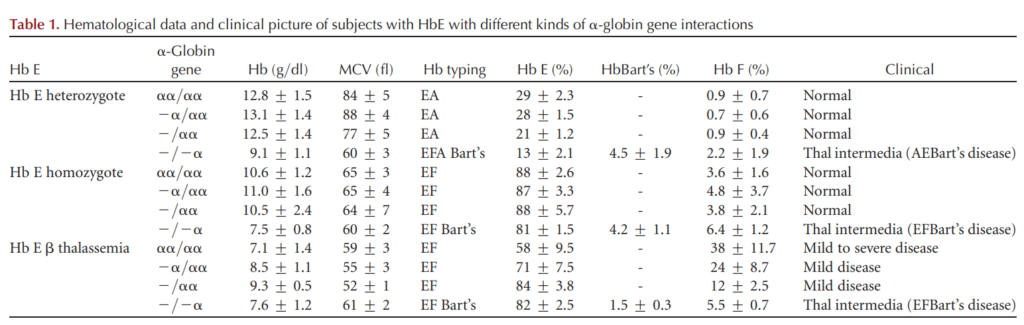
- Genotypes/phenotypes:
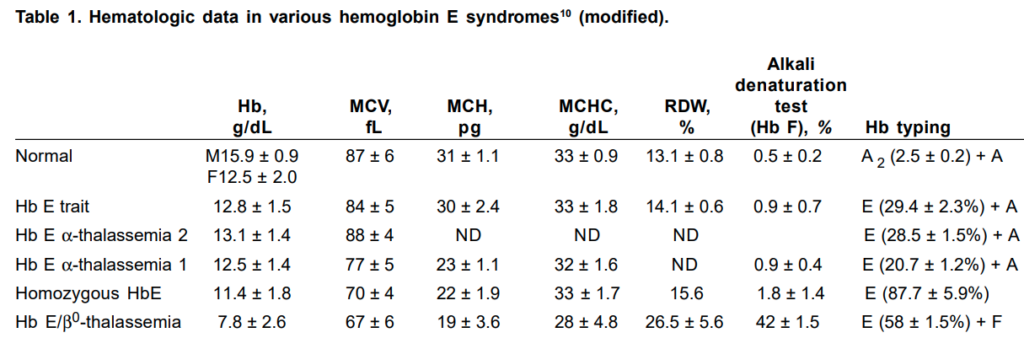
- Patients with HbE trait (HbAE) are asymptomatic and may have:
- Reduced MCV
- Reduced MCH
- Mild or no anemia
- Patients homozygous for HbE (HbEE, hemoglobin E disease) resemble those with heterozygous beta-thalassemia:
- Reduced MCV
- Reduced MCH
- Mild or no anemia
- Patients who co-inherit HbE and beta-thalassemia (HbE beta0-thalassemia) have a highly variable phenotype ranging from nontransfusion-dependent beta-thalassemia to transfusion-dependent beta-thalassemia.
- Patients with HbE trait (HbAE) are asymptomatic and may have:
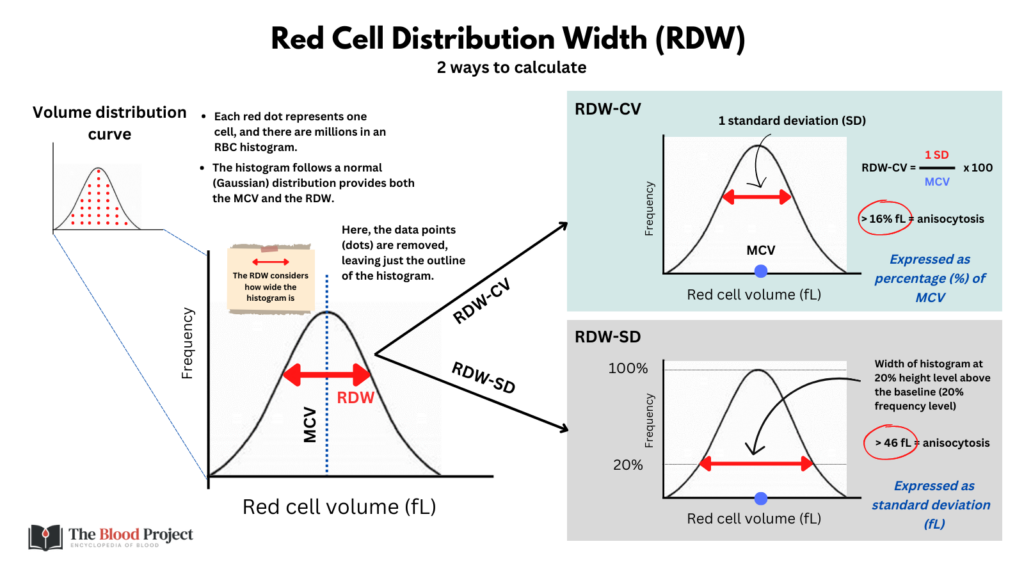
Question 4: Why is the RDW-CV (labeled RDW) increased, but not the RDW-SD?
- Because the RDW-CV is inversely proportional to the MCV. That’s why the RDW-SD is a better/more accurate measure of the RDW.