Therapeutic Plasma Exchange in TTP
Prev
1 / 1 Next
Prev
1 / 1 Next
Therapeutic plasma exchange (TPE) thrombotic thrombocytopenic purpura (TTP)
According to 2019 American Society for Apheresis Guidelines:
- Overview:
- TPE is a therapeutic procedure in which blood of the patient is passed through a medical device which separates out plasma from other components of blood. The plasma is removed and replaced with a replacement solution such as colloid solution (e.g., albumin and/or plasma) or a combination of crystalloid/colloid solution.1
- TPE is one of several therapeutic apheresis modalities. Others include:
- Erythrocytapheresis
- Leukocytapheresis
- RBC exchange
- Thrombocytapheresis
- Extracorporeal photopheresis
- In thrombotic thrombocytopenic purpura (TTP), TPE is used to:
- Replace ADMATS13
- Remove antibodies against ADAMTS13
- Treatment notes:
- For autoimmune TTP
- TPE has decreased overall mortality of immune mediated TTP from nearly uniformly fatal to <10-20%.
- TPE should be initiated emergently once the diagnosis is recognized. If TPE is not immediately available, large dose plasma infusions (25-30 mL/kg), may be given if tolerated, until TPE can be initiated.
- Corticosteroids should be used as an adjunct, either a daily prednisone dose at 1 mg/kg/day, pulsed methylprednisone for a few days, or a combination.
- Rituximab is commonly used to treat refractory or relapsing TTP. Studies have also described the incorporation of rituximab as adjunctive agent with initial TPE. Since rituximab immediately binds to CD20-bearing lymphocytes, an 18-24-hour interval between its infusion and TPE is used in practice.
- Platelets should only be transfused if potential life-threatening bleeding is present.
- Congenital TTP is characterized by constitutive deficiency of ADAMTS13 activity without an inhibitor, simple infusions of plasma (10-15 mL/kg) or cryoprecipitate (which contains ADAMTS13) or plasma derived vWF concentrates have been used.
- For autoimmune TTP
- Technical notes:
- Allergic reactions and citrate reactions are more frequent due to large volumes of plasma required.
- Fibrinogen levels may decrease following serial TPE procedures with cryoprecipitate depleted plasma as replacement.
- The use of cryoprecipitate depleted plasma as replacement may be associated with more frequent acute exacerbations.
- Duration and discontinuation:
- TPE is generally performed daily until the platelet count is >150 × 109/L, and LDH is near normal for 2-3 consecutive days.
- The role of tapering TPE over longer duration has not previously been studied prospectively but is currently being reviewed.

Other considerations (source):
- In one study of patients with TTP receiving TPE, the total number of TPE varied widely from four to 21, with an average of 13 TPEs.
- TPE procedure involves connecting the patient’s vasculature to the apheresis device, which separates the plasma ex vivo and replaces it with one of the following fluids:
- An oncotic solution such as 5% albumin
- Donor plasma (the replacement fluid of choice in TTP)
- Combination of colloid solutions or with a crystalloid solution (such as 0.9% saline)
- All TPE devices approved in the United States are centrifugation based as opposed to the membrane-based devices used in other countries. Centrifugation-based devices:
- Require blood flow rates that range from 50 to 120 mL/min.
- Separate blood components based on the specific gravity of plasma (range, 1.025-1.029), which is lower than that of red blood cells (range, 1078-1.114; most dense), leukocytes, and platelets, when the blood is exposed to an appropriate centrifugal force (G force).
- Because the blood flow from the patient into the device has to be steady (continuous) and > 50 mL/min:
- The site of vascular access has to withstand high negative pressure without collapsing.
- The line from the device returning the patient’s cells admixed with the replacement fluid also has to be in a large blood vessel capable of tolerating high positive pressure.
- Among the options to obtain vascular access in a patient undergoing TPE, the options include
- Peripheral veins and arteries of the hands and arms
- Internal jugular veins
- Subclavian veins
- Femoral veins and arteries
- AV fistulae and grafts
- Peripheral venovenous access is the primary access method in Europe, whereas CVCs are the primary access method in North, Central, and South America.
Guideline recommendations
Guidelines on the Use of Therapeutic Apheresis in Clinical Practice:
- TPE should be initiated emergently once the diagnosis is recognized (Grade 1A recommendation)
- If TPE is not immediately available, large dose plasma infusions (25-30 mL/kg), may be given if tolerated, until TPE can be initiated.
British Committee for Standards in Haematology guidelines:
- In view of the high risk of preventable, early deaths in TTP, treatment with PEX should be initiated as soon as possible, preferably within 4–8 h, regardless of the time of day at presentation, if a patient presents with a MAHA and thrombocytopenia in the absence of any other identifiable clinical cause.
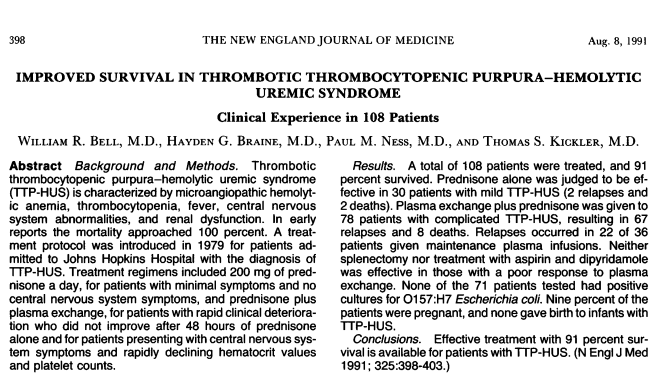
Seminal study showing improved survival in patients with TTP receiving plasma exchange:
Prev
1 / 1 Next
