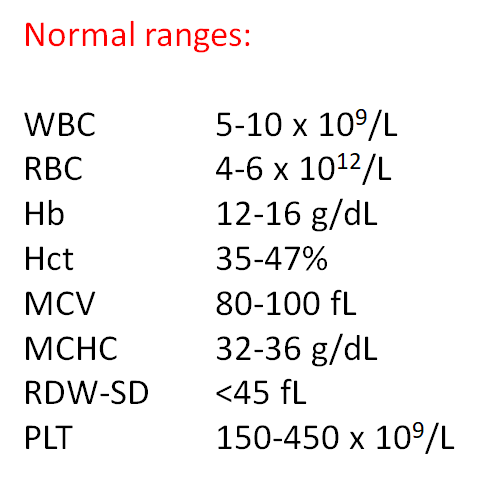
Quiz 1 – Red Cell Indices
By William Aird
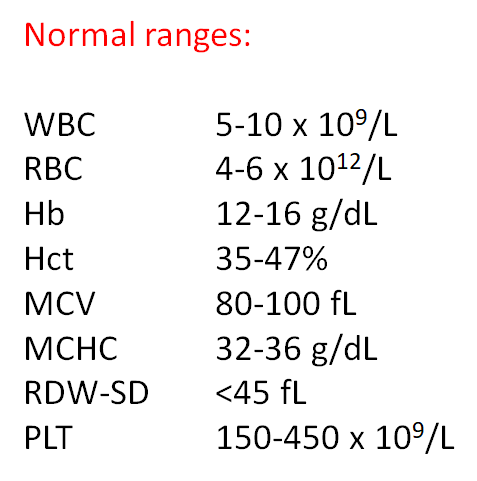
Abbreviations:
Hb – hemoglobin
Hct – hematocrit
MCH – mean corpuscular hemoglobin
MCHC – mean corpuscular hemoglobin concentration
MCV – mean cell colume
RBC – red blood cell count
RDW – red blood cell distribution width
RDW-CV – RDW coefficient of variation
RDW-SD – RDW standard deviation
Note: The terms MCV, MCH and MCHC are all mean values and by definition apply to populations of red cells. To simplify matters, we use the term more loosely to include descriptions of single cells. For example, we may refer to a large red cell as one with a high MCV, or a cell with increased central pallor as one with a low MCHC.
Question 1
Which conditions are associated with microcytosis?
Question 2
Which conditions are associated with macrocytosis without anemia?

Question 3
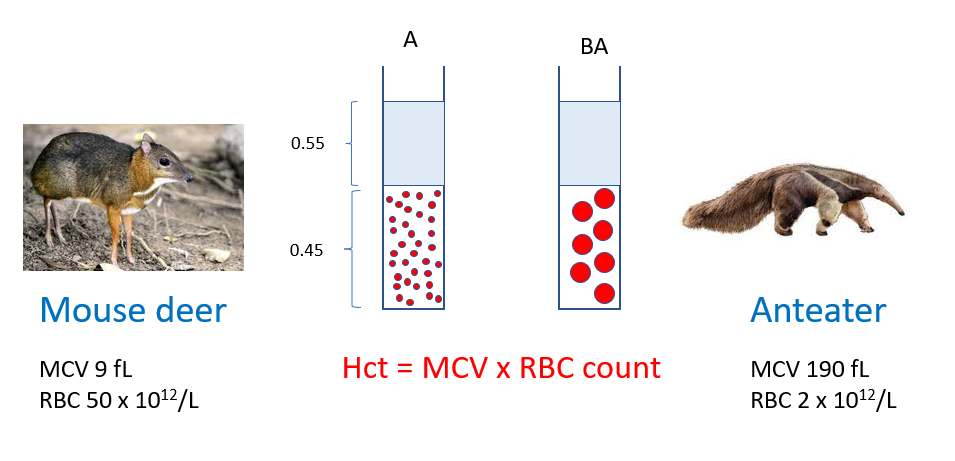
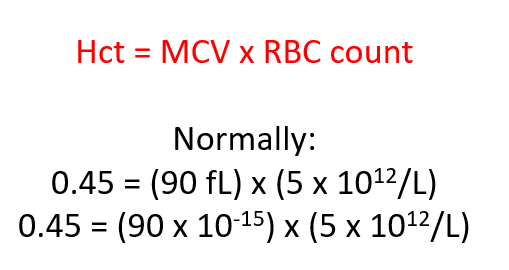
Which RBC parameter is evolutionarily conserved across species?
Spun hematocrits
Question 4
What is MCV defined as?
Remember:
Question 5
What does anisocytosis mean?
Question 6
Which of the following red cell indices is/are expressed as a concentration?
Question 7
Which of the following red cell indices are expressed as a weight?
Question 8
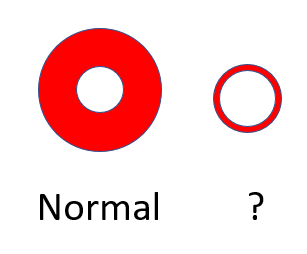
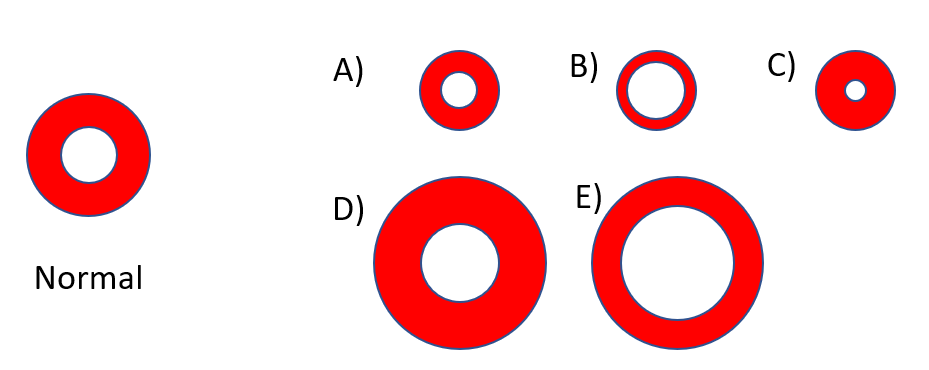
How would you describe the red cell on the right (schematic of a normal red cell is shown on the left)?
Question 9
What method(s) are used to measure/calculate the Hct?
Spun Hct



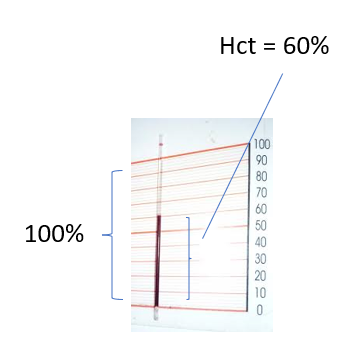
Question 10
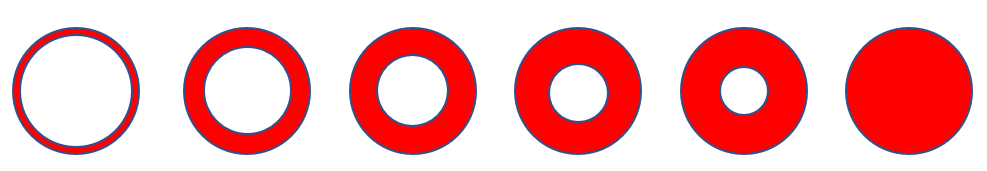
What is happening to the mean cell hemoglobin (MCH) moving left to right (assume a constant central pallor or MCHC)?
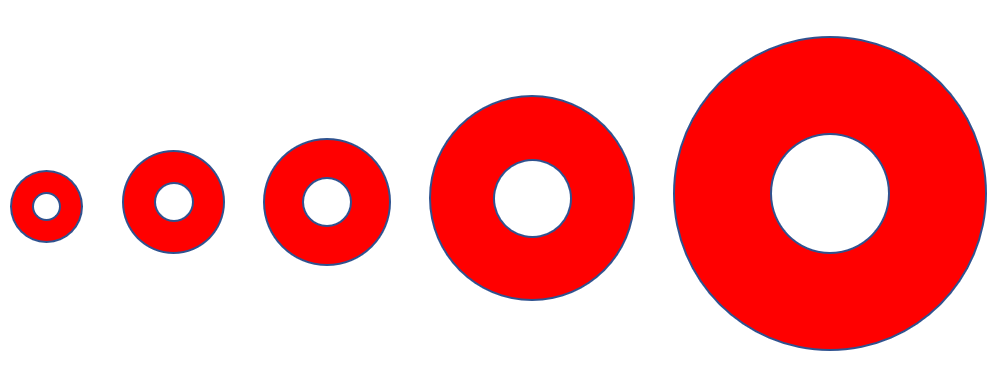
Question 10
MCH tracks with the MCV
Question 11
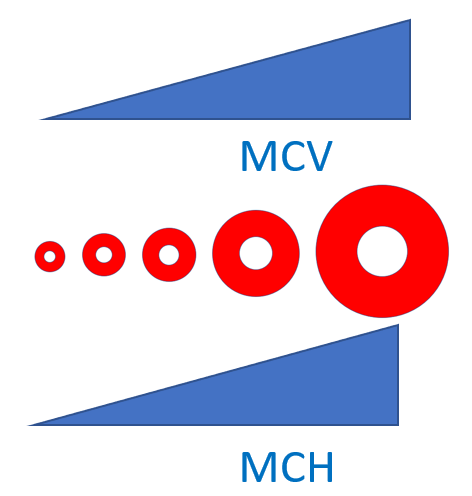
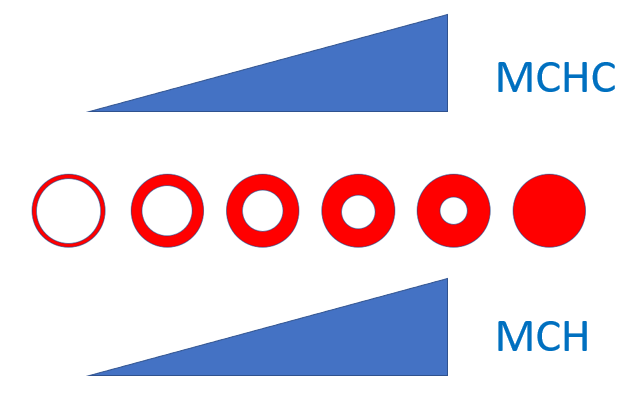
What is happening to the mean cell hemoglobin (MCH) in this series of red cells (moving left to right)? Note that the red cell volume is the same in all cells.
Question 11
MCH also tracks with the MCHC
Question 12
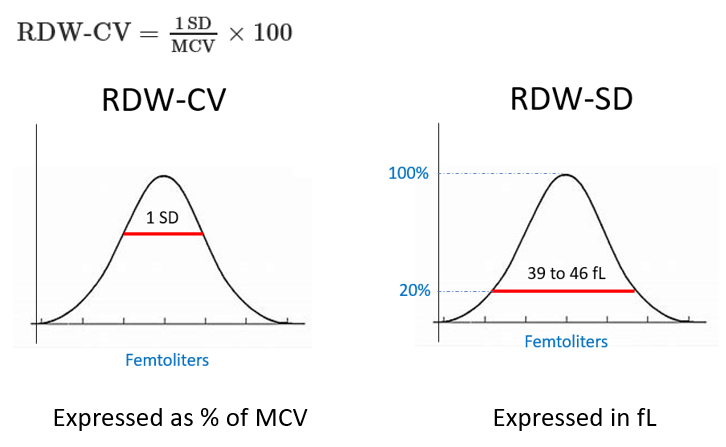
What are two ways of calculating the RDW?
Question 12 (cont’d)
The RDW-CV measures size dispersion by means of a ratio formula of 1 standard deviation to the MCV, and is expressed as a percentage of the MCV (reference range of 11% to 16%)
The RDW-SD is the arithmetic width of the distribution curve measured at the 20% frequency level and is expressed as standard deviation in femtoliters (fL) (reference range 39-46 fL)
Question 13
What happens to the RDW-CV when the MCV is low?
Question 13 (cont’d)
Because the RDW-SD is not influenced by the MCV, it is considered by some to be the superior method for measuring the RDW.
Question 14
Which of the following may explain a normal MCV in iron deficiency anemia (IDA)?
Question 15
Does a normal MCV rule out iron deficiency anemia (IDA)?
Question 16
What conditions may be associated with iron deficiency without the presence of anemia?
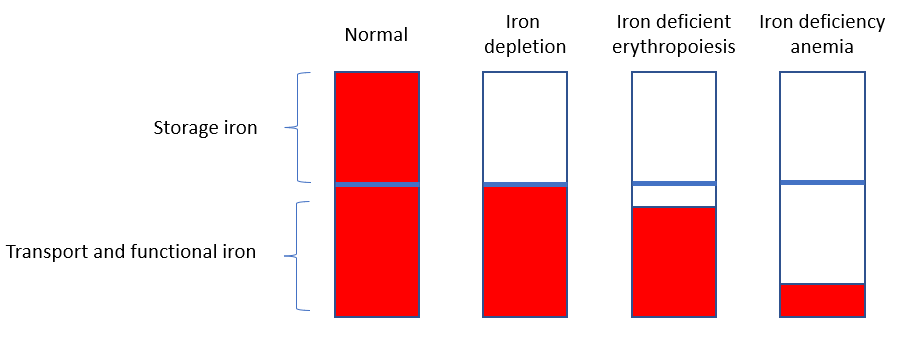
Stage 1 – iron depletion
- Storage iron depleted (primarily macrophages)
- Only remaining iron is in the transport and functional (e.g. Hb) pools
- Serum ferritin (marker of iron stores) low
Stage 2 – Iron deficient erythropoiesis
- Reduction of transport iron
- Decreased serum iron
- Increased total iron binding capacity (TIBC) to maximize iron transport to red cells
- Increased expression of transferrin receptor on RBC membrane to promote iron uptake
Stage 3 – Iron deficiency anemia
- RBCs are no longer able to compensate, and production falls
Question 17
Describe the CBC (answer on next slide)
| WBC | Hb | Hct | MCV | MCHC | RDW-SD | PLT |
|---|---|---|---|---|---|---|
| 5.6 | 17.8 | 54 | 70 | 33 | 52 | 440 |
Question 17 (cont’d)
Description of CBC: Leukocytosis, polycythemia, microcytosis, elevated RDW and thrombocytosis
This was a patient with polycythemia vera who presented, as many do, with iron deficiency (presumably from slow GI blood loss and increased iron requirements for erythropoiesis)
Question 18
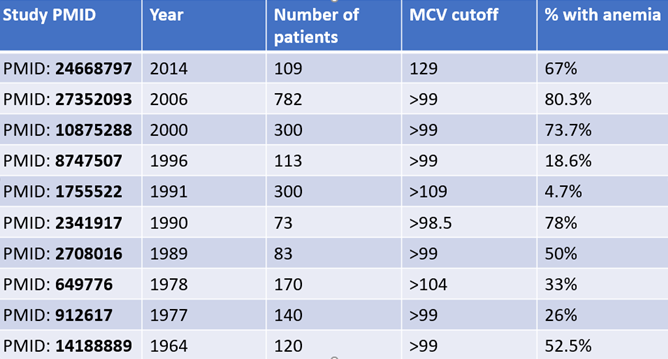
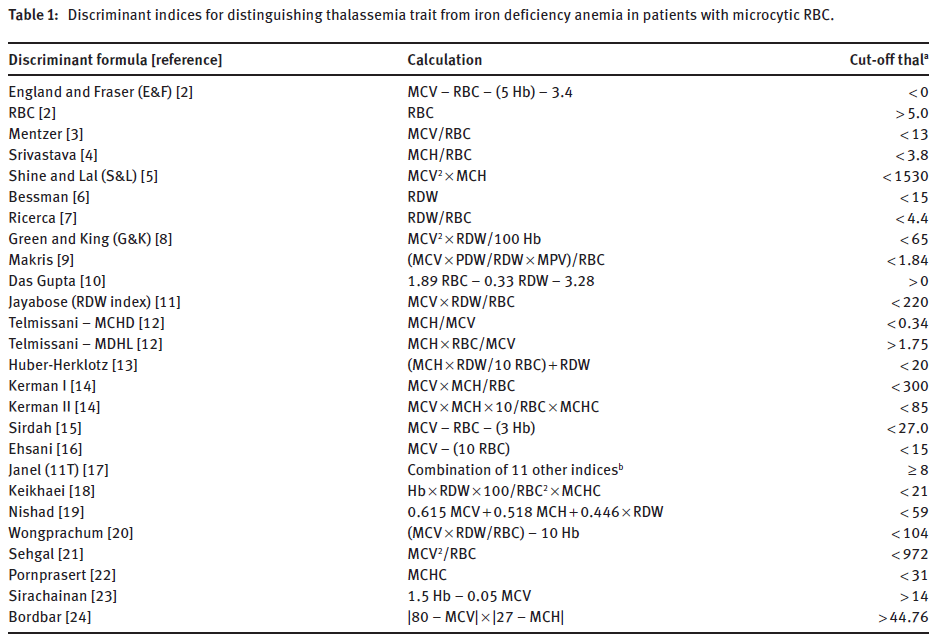
What is the Mentzer index (one of many indices used to distinguish between iron deficiency anemia and thalassemia minor) (see NOTES page for other)?
Discriminatory formulas for distinguishing thalassemia from iron deficiency in patients with microcytic anemia (the Mentzer index is third from the top)
Question 19
What are the 2 ways to lower the MCH?
Question 20
Which parameters correlate with MCHC?
Question 22
What is a red cell with reduced MCHC called?
Question 23
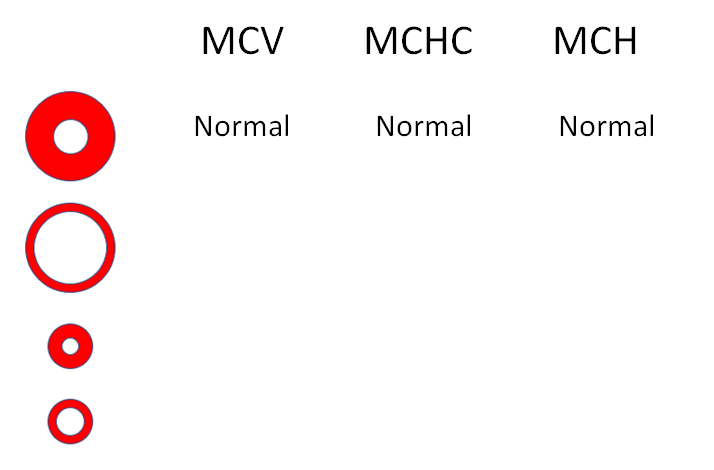
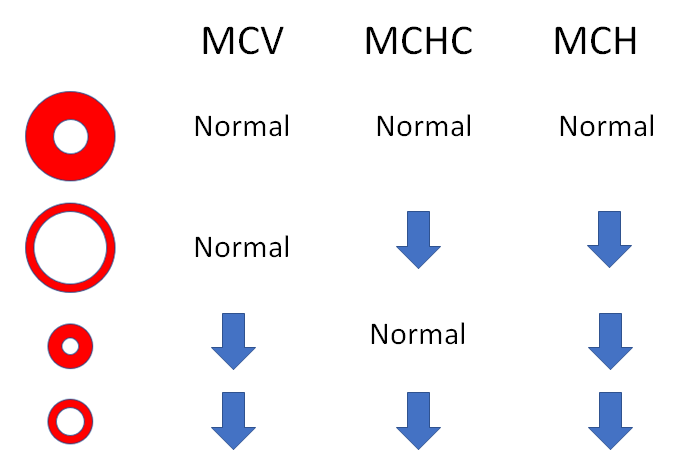
Fill in the parameters: Normal, increased or decreased (answer on next page)
Question 23 (cont’d)
Fill in the parameters: Normal, increased or decreased (answer on next page)
Question 24
How would you describe these results (see next slide for answer)?
| WBC | Hb | Hct | MCV | MCHC | RDW-SD | PLT |
|---|---|---|---|---|---|---|
| 6.1 | 13.3 | 40 | 84 | 33 | 44 | 384 |
| Parameter | Value | Normal value |
|---|---|---|
| Iron | 42 | 30-160 ug/dL |
| Total iron binding capacity | 417 | 260-470 ug/dL |
| Ferritin | 12 | 13-150 ng/ml |
Question 25
What are spurious causes of macrocytosis?
Question 25
What are the three most common causes of microcytosis?
Question 26
What is the prevalnce of macrocytosis in the genral population?
Question 27
What happens to the mean cell volume of red cells as people age?
Question 28
Does alcohol intake cause macrocytosis independent of liver disease?
Question 29
What is wrong with the following statement (answer on next slide)?
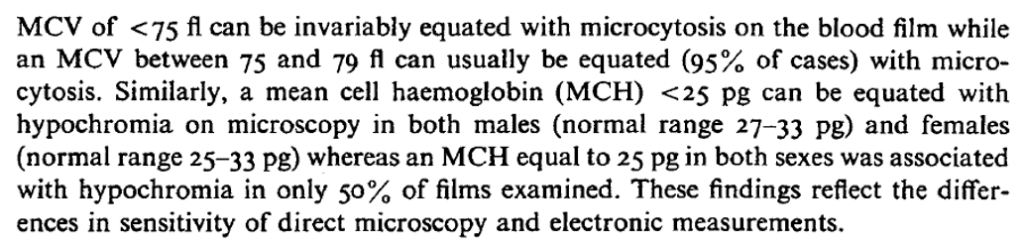
Question 13 (cont’d)
Hypochromia is represented by a low MCHC, not MCH
Question 30
Increased numbers of reticulocytes can increase the MCV. What is the effect of anemia on reticulocytosis-mediated macrocytosis?
Question 31
Which RBC best describes the phenotype in hypernatremia when measured in vitro (as part of a CBC)?
Question 32
Is the RBC count low, normal or high in this patient (answer on the next slide)?
| WBC | RBC | Hb | Hct | MCV | MCHC | RDW-SD | PLT |
|---|---|---|---|---|---|---|---|
| 9.2 | ? | 12.1 | 36.3 | 106 | 33.3 | 51.4 | 219 |
Question 32 (cont’d)
Is the RBC count low, normal or high in this patient?
| WBC | RBC | Hb | Hct | MCV | MCHC | RDW-SD | PLT |
|---|---|---|---|---|---|---|---|
| 9.2 | 3.4 | 12.1 | 36.3 | 106 | 33.3 | 51.4 | 219 |
The RBC is low. Evolution has selected for an optimal Hb/Hct. In this case because the MCV is increased, the RBC count is correspondingly reduced to maintain a normal Hb/Hct.
Question 33
A patient has a Hb 8 g/dL and Hct 29%. What is the most likely diagnosis?
Question 34
What are the 2 most likely causes of MCV > 130 fL?
Question 35
Which parameters is copper deficiency associated with?
Question 36
Which of the following is/are causes of transient change in the mean cell volume (MCV)?:
Question 37
Reticulocytes can be detected on Wright Giemsa, true or false?
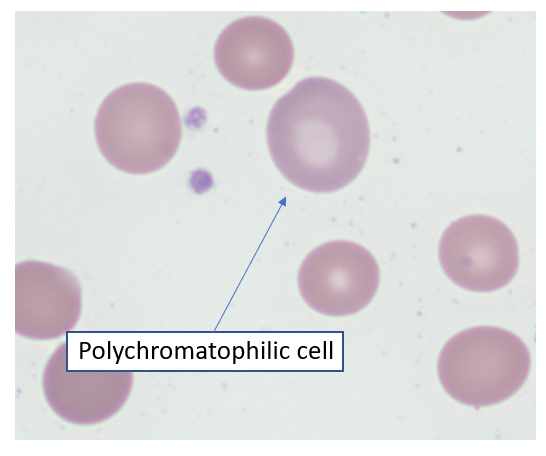
Wright Giemsa stain showing polychromatophilic cell. According to the College of American Pathologists, polychromatophilic cells are nonnucleated, round, or ovoid red cells staining homogeneously pink-gray or pale purple. They are larger than mature RBCs and usually lack central pallor
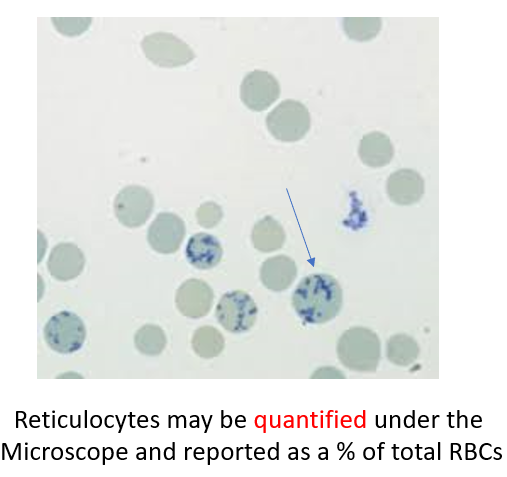
On supravital stains (meaning that the slide is stained without prior fixation – the RBCs are still “alive” when they are incubated with the staining solution), reticulocytes are identified by clumped granular material called reticulum (this is where the term “reticulocyte” comes from). Reticulum consists of aggregates of residual ribosomes mitochondria.
Question 38
What is the MCHC of a typical reticulocyte?
Question 39
Reticulocytosis may cause macrocytosis. What is the MCV of a typical reticulocyte?
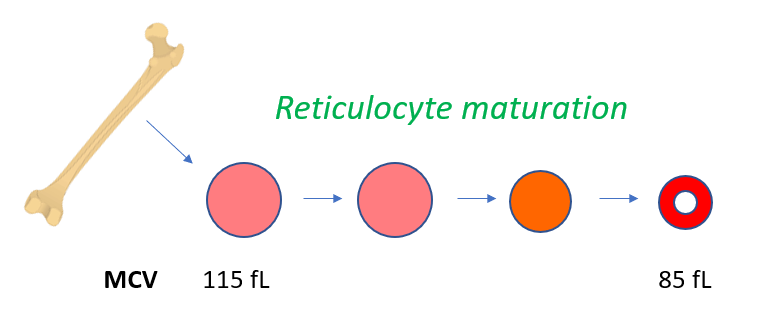
values from increased production and shortening of marrow maturation time (leading to increased retic circulation time).
Question 40
How often is macrocytosis not associated with anemia?