42 yo M with Hemolytic Anemia and Thrombocytopenia
Note in Emergency Department:
"42-year-old M with no past medical history who presents to the ED after labs at urgent care showed platelet count of 7k. He reports having right frontal/periorbital headaches last week. He went to an [outside hospital] 4 days ago and was discharged after evaluation. Did not have blood work there. Then two days ago, he noted a dotted rash on his elbows and thighs for which he went to urgent care. He had blood work there which showed Hb ~10 and platelets 7. He was asked to come to the ED. He also reports epistaxis 2 days ago which resolved by self. Currently he denies having headaches, bleeding issues, fevers, chills. No confusion, weakness, numbness noted. He also denies having bloody diarrhea or diarrhea."
Is this story consistent with a diagnosis of TTP?
Do you expect hemolytic markers to be positive, if the patient has TTP?
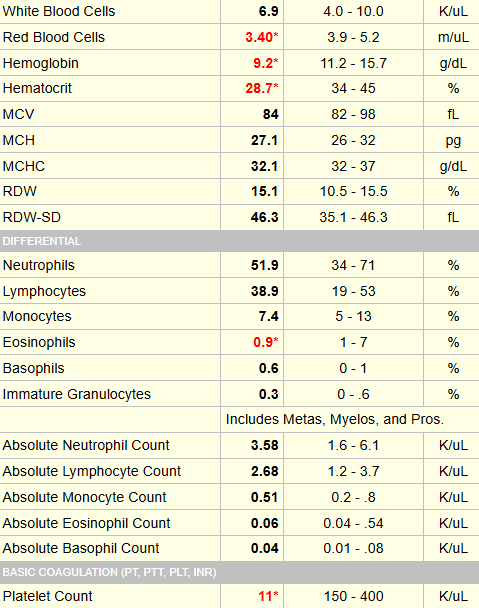
Results of hemolysis markers at time of admission:
- Haptoglobin < assay
- LDH 799 IU/L (normal range 94-250)
- AST normal
- Total bilirubin not done
- Reticulocyte count 0.14 x 1012/L
The smear was similar to the one shown below:
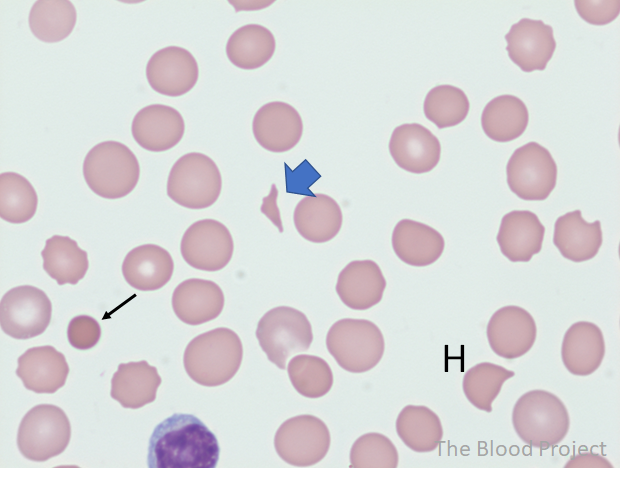
Which of the causes of MAHA is/are also associated with thrombocytopenia:
So far, the data are most consistent with a diagnosis of TMA. There are many different causes of TMA. One of these, TTP, has a mortality of about 90% if left untreated.
This patient had blood drawn for ADAMTS13 activity level at the time of admission. However, this is a send out test and takes 3-4 days to come back. We cannot afford to wait this long to decide on treatment. Instead, we use a clinical prediction rule to determine pretest probability of having TTP and empirically treat those who are at high risk.
The results of the PLASMIC score in this case are shown below:
This patient had the highest possible score, and as per strong recommendations by clinical practice guidelines, received which of the following treatments:
In response to corticosteroids and TPE, the patient’s platelet count (and haptoglobin, not shown) increased nicely with normalization after 5 daily therapeutic exchanges (with one volume per exchange):
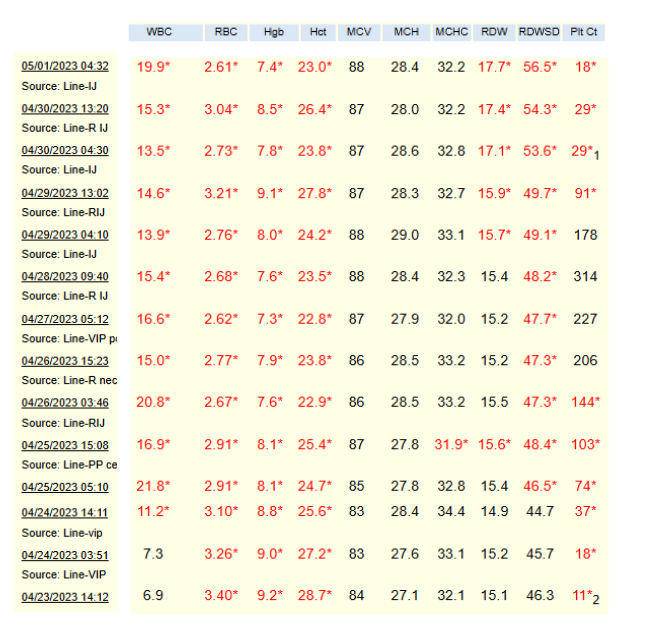
This patient had a clinical response, which is defined as a sustained normalization of platelet count (for example, > 150 × 109/L) and lactate dehydrogenase (LDH) level < 1.5 times the upper limit of normal after cessation of plasma exchange.
However, his platelet count subsequently fell again within several days, requiring reinstitution of therapeutic plasma exchange. This qualifies as an exacerbation, defined as a fall in platelet count to below the lower limit of the reference range (for example, < 150 × 109/L) requiring reinitiation of plasma exchange within 30 days of the last plasma exchange after initial clinical response had been achieved.
As shown in the next slide, he responded well to reinitiation of therapeutic plasma exchange.

The results of the ADAMTS13 activity assay came back 4 days after the patient was admitted:
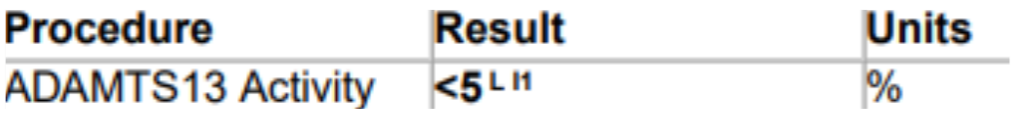
What statement is correct (choose one):
The patient had an ADAMTS13 inhibitor study done, which was positive, indicating this was a case of immune TTP.

The patient did well and was discharged in remission. He received one additional treatment, which continued as an outpatient.


