Case Study
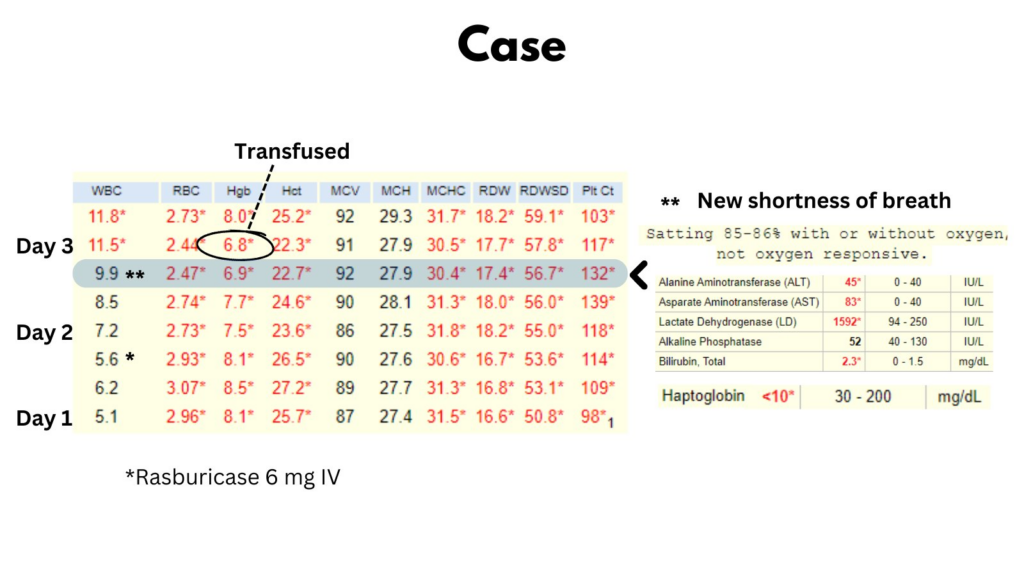
64 yo M presents with B symptoms, generalized adenopathy and evidence of tumor lysis syndrome. He is given a dose of Rasburicase in the ED. The next day he develops shortness of breath. His SaO2 is 85% and does not increase with supplemental O2. Compared with baseline on admission, his labs now show:
- Drop in Hb
- Increased AST:ALT ratio (normal on admission)
- Elevated LDH (about 500 IU/L on admission)
- Low haptoglobin (normal on admission)
Taken together, these data are consistent with hemolysis.
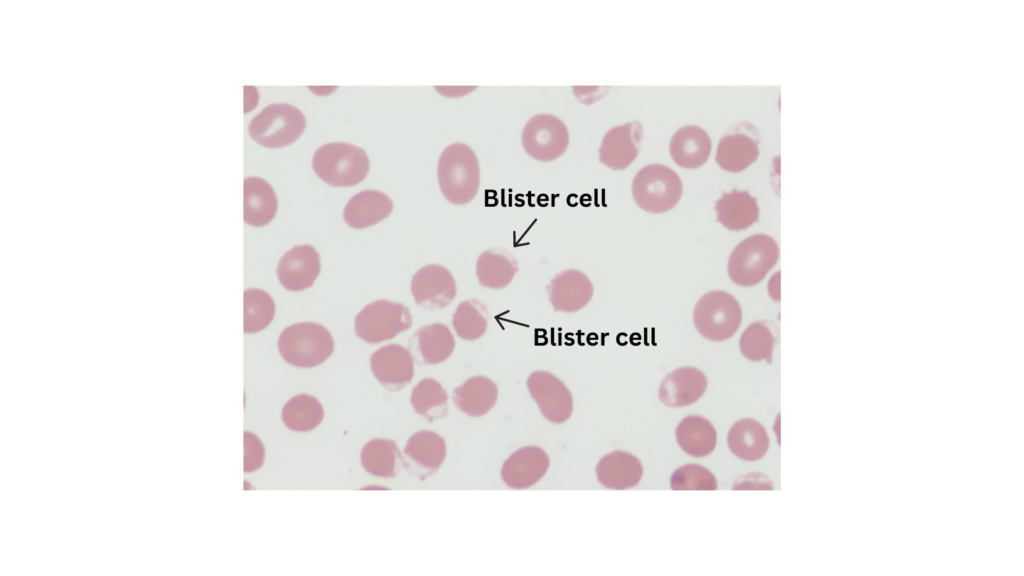
Peripheral smear (actual smear from this patient shown below) demonstrated a multitude of blister cells, occasional bite cells. The Heinz body prep was positive (not shown).
The ICU team noted that G6PD activity levels, which were drawn the night before (day 2), came back earlier that day showing deficiency. This clued them into the possibility of Rasburicase-mediated methemoglobinemia (MHb). Indeed the MHb level came back at 7%, confirming their suspicion.
