Postscript
Have you ever heard of Gaïsbock disease or Gaïsbock syndrome? I learned about it in medical school as a cause of polycythemia. But I rarely hear mention of it today.
- Is it a real phenomenon?
- If it is real:
- What is its pathophysiology?
- What are the diagnostic criteria?
- How should we treat it?
Let’s start with some facts so that we are all on the same page:
- The terms polycythemia and erythrocytosis are used interchangeably today.
- Polycythemia/erythrocytosis may be:
- Relative, which is associated with:
- Normal red cell mas
- Reduced plasma volume
- Absolute, which is associated with:
- Elevated red cell mass
- Normal plasma volume
- Relative, which is associated with:
- Relative polycythemia may be:
- Acute, owing to:
- Early diuretic use (plasma volume normalizes over time)
- Burns
- Diarrhea
- Vomiting
- Third spacing
- Chronic
- Gaïsbock syndrome?
- Acute, owing to:
- Absolute polycythemia may be:
- Primary (polycythemia vera)
- Secondary
- Before the invention of red cell mass measurements, there was no way of determining with certainty whether an elevated hematocrit or hemoglobin was secondary to increased red cell mass or decreased plasma volume. This makes assessment of early studies very difficult.
At the turn of the 20th century, Richard Cabot, a physician from the Massachusetts General Hospital wrote:
In 1905, Felix Gaïsbock (from Innsbruck, Tyrol, Austria) observed that some patients with hypertension and vascular disease appear plethoric or apoplectic 1. He described 18 male patients in whom hypertension was associated with an elevated red cell count and Hb but without splenomegaly. He named the condition polycythemia hypertonica. He believed the condition to be a true form of polycythemia, though distinct from polycythemia vera (known at the time as Vasquez disease). Since blood volume determinations were not done in his cases, it is not possible to determine the exact type of polycythemia he described.
In 1952, Lawrence and Berlin reported 18 cases of apparent, relative or stress polycythemia in which blood volume measurements revealed a decrease in plasma volume and a normal circulating red cell mass. The following was the typical patient profile:
- Male in the fourth or fifth decade
- Overweight
- Ruddy cyanosis
- Hypertension
- Moderate elevation of the red count, hemoglobin, or hematocrit with a normal white count and platelet count
The authors concluded:
In many respects these patients seem to fit into the group of patients described by Gaïsbock in which there were polycythemia and hypertension but no splenomegaly.
The authors attributed the blood abnormality to stress:
The psychiatric background of some of these patients indicated that they had been subjected to undue nervous stress and strain. One is tempted to relate the blood volume changes in these patients to some form of emotional stress and to class this condition as a psychosomatic phenomenon.
In 1953, William Dameshek wrote in an editorial:
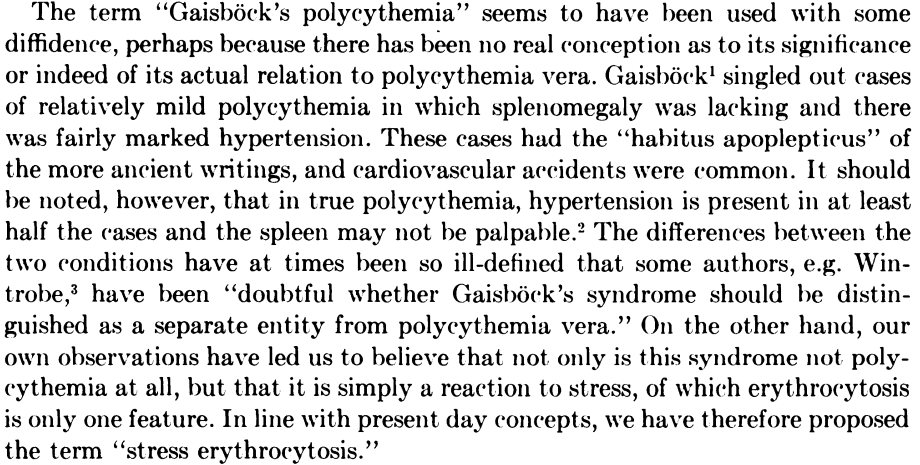
In 1962, similar cases were encountered by Kaung and Peterson who described ten cases with relative polycythemia or pseudopolycythemia 2. In these cases also there was a high incidence of hypertension and thromboembolic disease.
In 1964, Russell and Conley commented that “until recently Gaisböck’s syndrome has received little attention, and some modern authors have even questioned its independent existence.” They then describe a series of patients with a clinical profile consistent with Gaisböck’s:
- Predominantly white men
- Early middle age
- Overweight/sticky habitus
- Plethoric appearance with suffusion of the eyes
- Many had tense and anxious personalities
- Most were smokers
- Hypertension and the manifestations of vascular disease
The authors stated in their Discussion that:
The syndrome is not rare and occurs much more frequently than polycythemia. In our survey of 6,000 patients in a general hospital, seven new cases were discovered while no new cases of polycythemia vera were encountered.
In 1965, Hall named the condition Gaïsbock disease: “Gaisbock’s name is used as an eponym in recognition of his early attempt to separate an entity from the classification of polycythemia vera, where it does not belong.” Hall identified a subgroup of patients with apparent polycythemia with what he believed to be Gaïsbock disease or syndrome. Common manifestations included:
- Plethora
- Vascular disease
- Labile hypertension
- Headaches
- Excessive nervousness or tension
- Obesity
Splenomegaly and panmyelosis were notably absent.
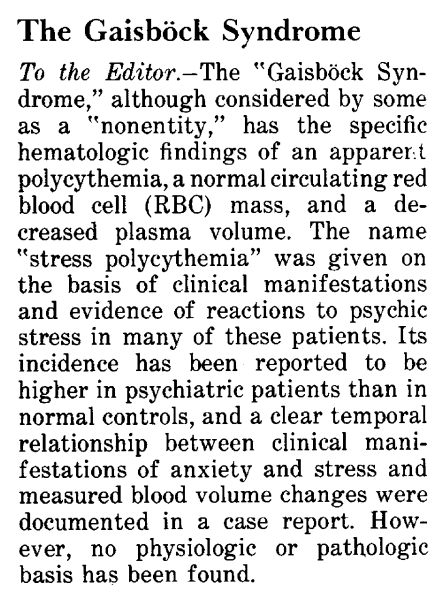
In 1972, a letter to the editor in JAMA raised the question of whether Gaïsbock disease/syndrome is a real entity:
In 1975, Burge et al published a study in which they stated:
Patients with a high packed-cell volume, low plasma volume, and normal red-blood-cell volume have been variously described as having pseudopolycythæmia, Gaisbock’s syndrome, relative polycythæmia, polycythemia of stress, and benign polycythæmia. Others maintain that these patients fall at the end of a normal distribution curve and have no disease.
The authors followed 35 patients presenting between 1962 and 1974 with relative polycythemia. The following were patient characteristics at presentation:
- 32 men, 3 women
- 24 smoked at presentation
- 7 were heavy drinkers
- 23 were “anxious” or “under undue stress”
- 8 patients were taking diuretics
- No patient had splenomegaly
- 9 patients had diastolic hypertension (authors: “this is a lower frequency of hypertension than that found by others in similar patients.”)
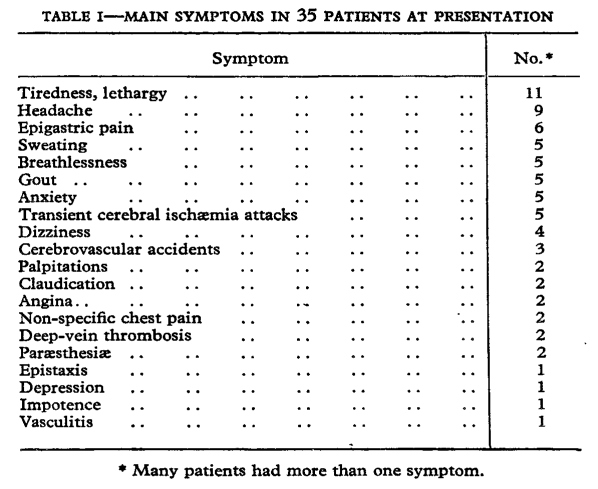
The authors concluded:
The argument whether pseudopolycythaemia is a single disease or just one end of a normal spectrum is
academic, since patients have symptoms which often produce disability and increased mortality.
In 1993, Pearson made a case to use the term relative polycythemia to cover related terms including Gaisbock’s syndrome:
Today, we still find reference to Gaisbock’s syndrome:
The following is from UpToDate (accessed September 2022):
Smokers may develop polycythemia from a combination of reduced plasma volume and increased RBC mass; these abnormalities generally return to normal with cessation of smoking. There is controversy regarding the existence of a distinct entity called Gaisböck’s syndrome (also referred to as spurious polycythemia or stress polycythemia), which was classically described as polycythemia in tense/anxious patients with hypertension, no splenomegaly, and reduced plasma volume. Hypertension with diuretic use and smoking may account for the relative polycythemia in many of these individuals… Smoking should be discontinued in all such patients.
In 2022, a group published the first review on Gaisböck’s syndrome in decades:
The authors cite population-level studies showing an association between 1) increased hematocrits and hypertension, and 2) higher hematocrits and a higher risk of death due to cardiovascular disease. They state that patients with relative or stress erythrocytosis should have volume contraction, and they propose a number of important factors in mediating relative erythrocytosis including:
- Hypertension itself
- Reduced antidiuretic hormone activity at night
- Nocturnal hypoxemia
- Chronic cigarette use
- Chronic alcohol use
Summary:
- There appears to be a syndrome of chronic relative polycythemia that is associated with:
- High hematocrit of venous blood
- Decreased plasma volume
- Normal red cell mass
- Hypertension (especially diastolic)
- Absence of splenomegaly, leukocytosis, and thrombocytosis
- This has been referred to as Gaïsbock syndrome; other terms include:
- Stress polycythemia
- Pseudopolycythaemia
- Spurious polycythemia
- Idiopathic erythrocytosis
- The term relative polycythemia is a broader term that includes all types of low plasma states, including:
- Acute fluid loss
- Gastrointestinal fluid loss
- Acute diuresis
- Third spacing (e.g., in acute pancreatitis)
- Chronically low plasma volume – Gaïsbock syndrome
- Acute fluid loss
- Because red cell mass (and plasma volume) measurements have fallen out of favor over the past 2 decades, it is no longer possible to accurately diagnose chronic relative polycythemia.
- While it has been proposed that patients with Gaïsbock syndrome may be at increased risk for developing cardiovascular complications, there is scant evidence to support this notion.
- Treatment includes antihypertensive therapy and smoking cessation. There is no proven role for phlebotomy.
