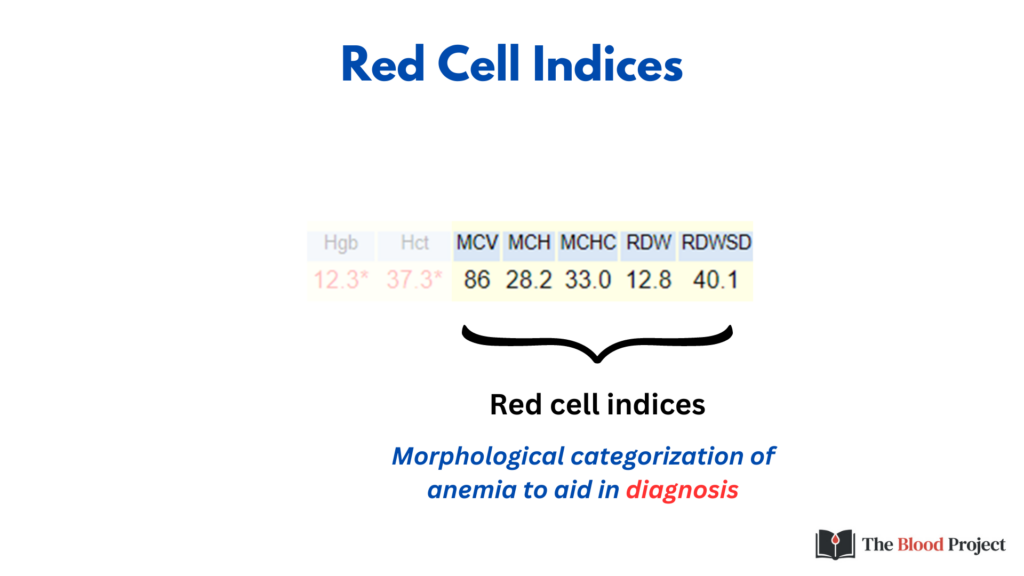
RBC Indices
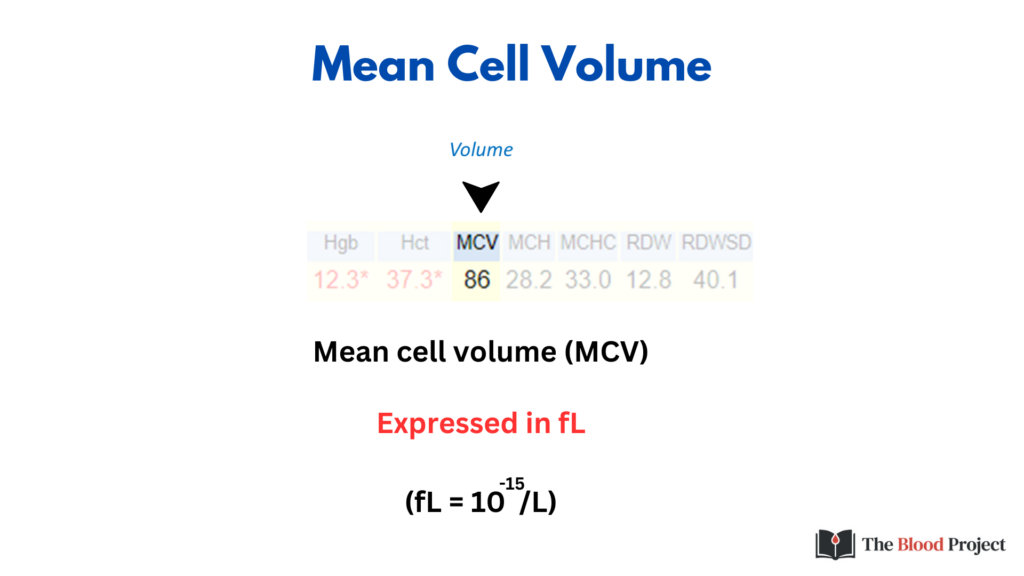
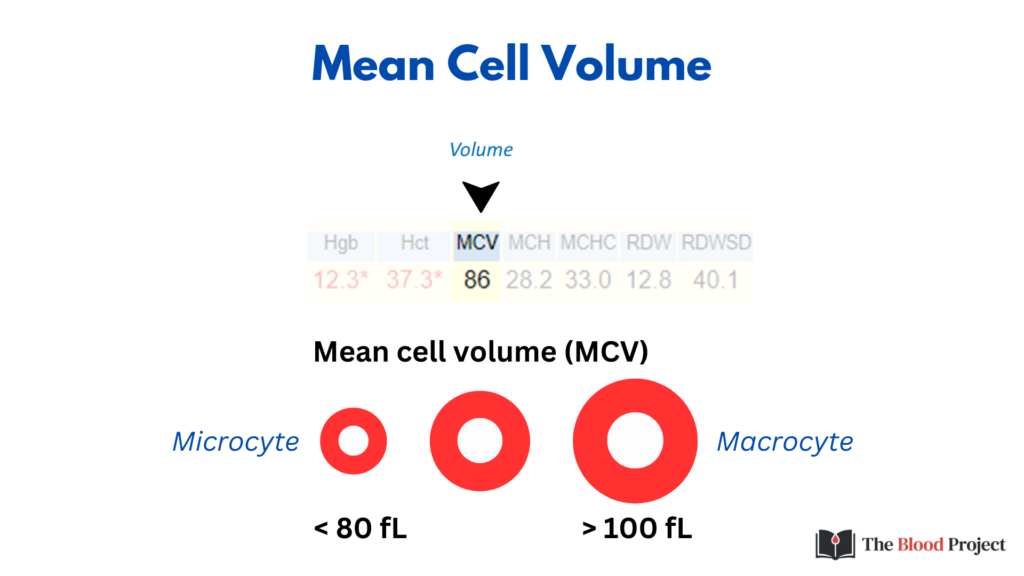
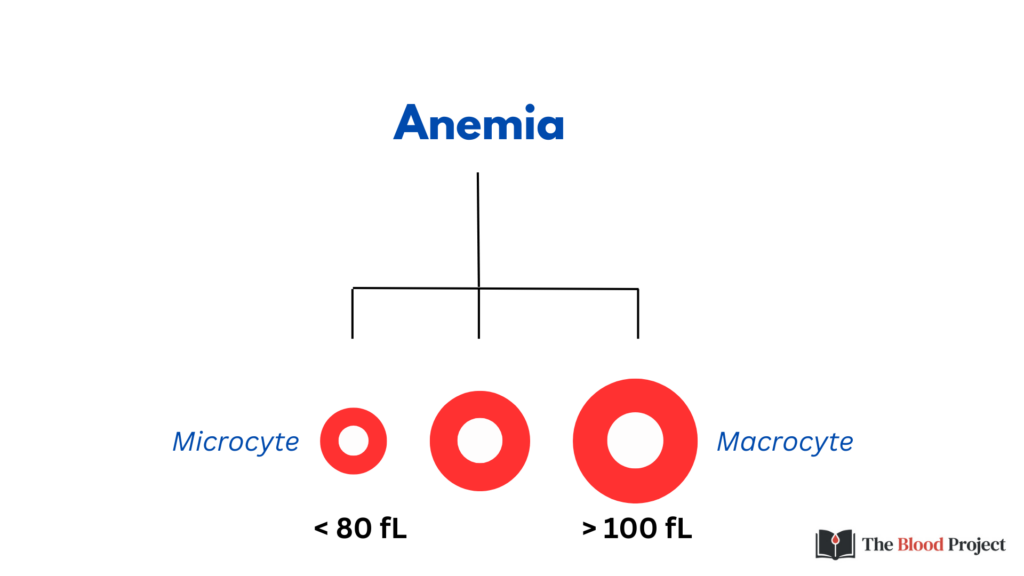
The MCV is the first branch point in the differential diagnosis of anemia (while some would place reticulocyte count proximal to MCV, many health care providers approach the differential diagnosis of anemia – at least initially – without the benefit of a reticulocyte count).
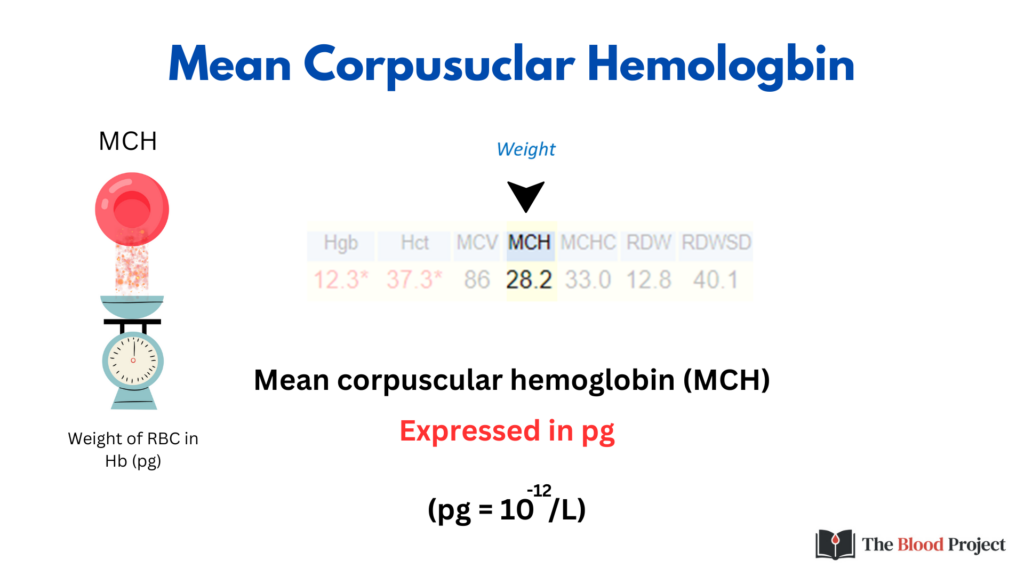
The MCH is the average weight of a single RBC in Hb. Imagine taking a single cell, puncturing a hole in it and emptying out the Hb (like you would saccharine from a packet of artificial sweetener) onto a scale. Repeat thousands of times and calculate the average – that’s the MCH!
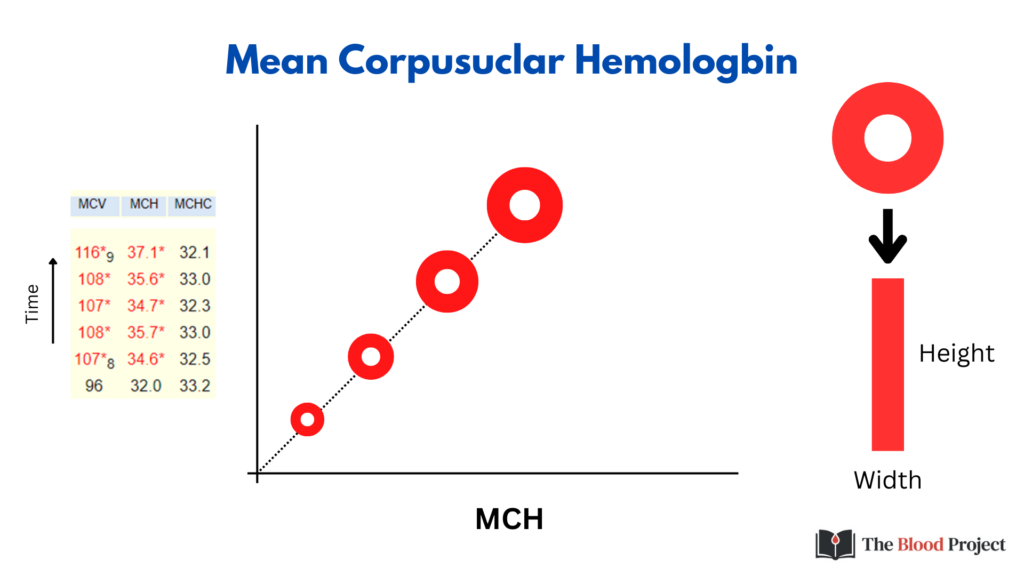
Note how the MCH tracks with MCV. Assuming we keep the MCHC (central pallor) constant, the greater the cell volume, the more weight in Hb. This is shown in the CBC time series on the left. One way to think of the MCH is to imagine counting up all the red pixels in a two-dimensional red blood cell as a marker for Hb weight, or to stretch out the red pixels in rectangular shape and calculate the area (height x width).
Because the MCH tracks with the MCH (and, as we will discuss shortly, the MCHC), it really does not offer any information beyond the latter two indices, and can safely be ignored. The one situation where the MCH may be helpful is when blood is stored for a prolonged period of time, and the red blood cells swell in the test tube, resulting in a spurious increase in the MCV. The MCH does not change no matter how much the red cells swell, so it may be used as a marker for the MCV on such occasions (e.g., with space travel research where blood is taken from an astronaut and stored at 4oC until landing).
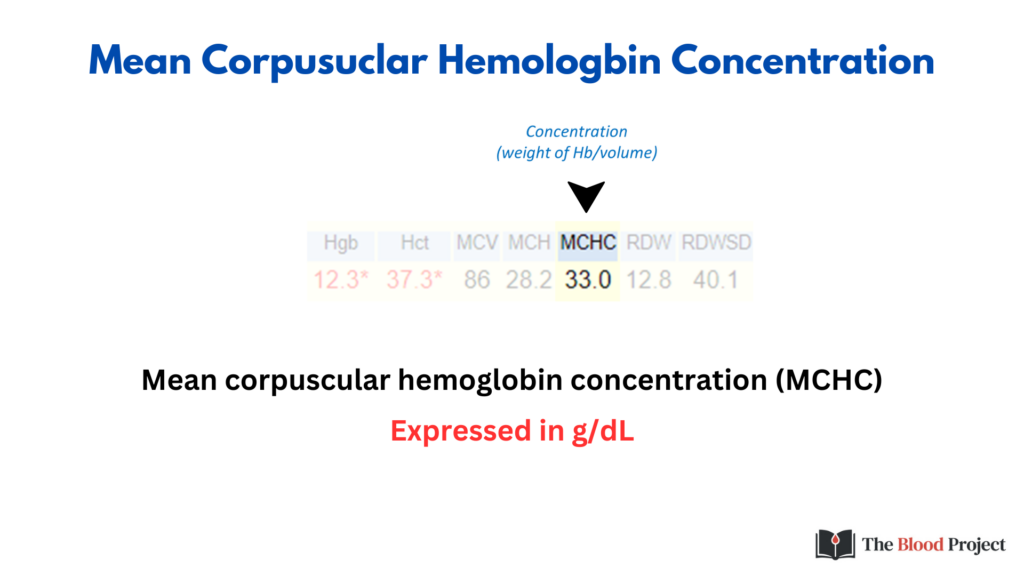
By contrast to the MCH the MCHC is a valuable index. The MCHC is a measure of the weight of Hb per volume of RBC and is reported in g/dL.
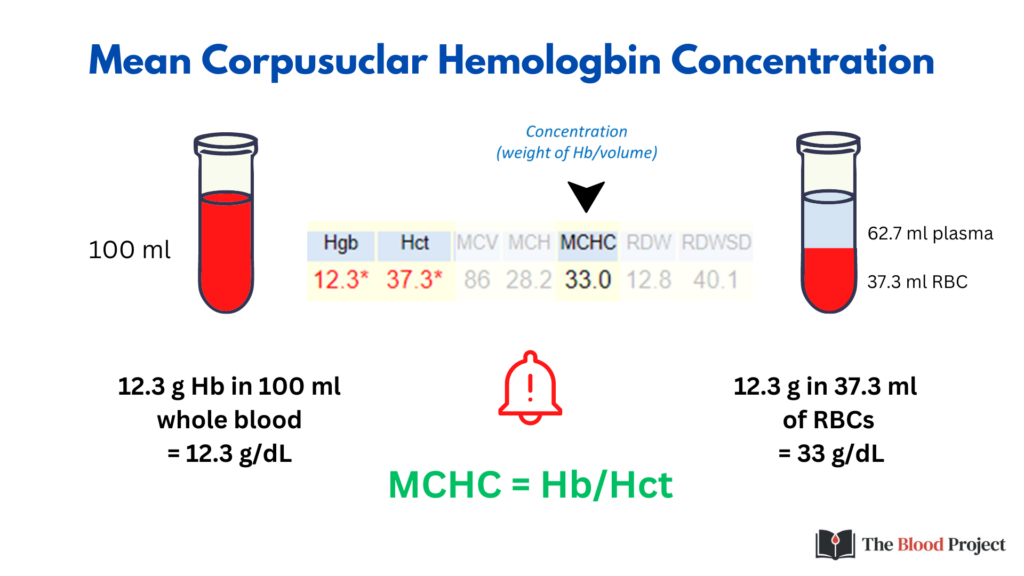
We don’t often think of the relationship between Hb and MCHC, but both measure Hb concentration, the difference being that Hb is a measure of Hb weight per whole blood, while MCHC is a measure of Hb weight per packed RBCs (whole blood minus the plasma). The formula MCHC = Hb/Hct is key to understanding the difference between Hb and Hct. We will come back to that when we discuss the so-called 3:1 rule.
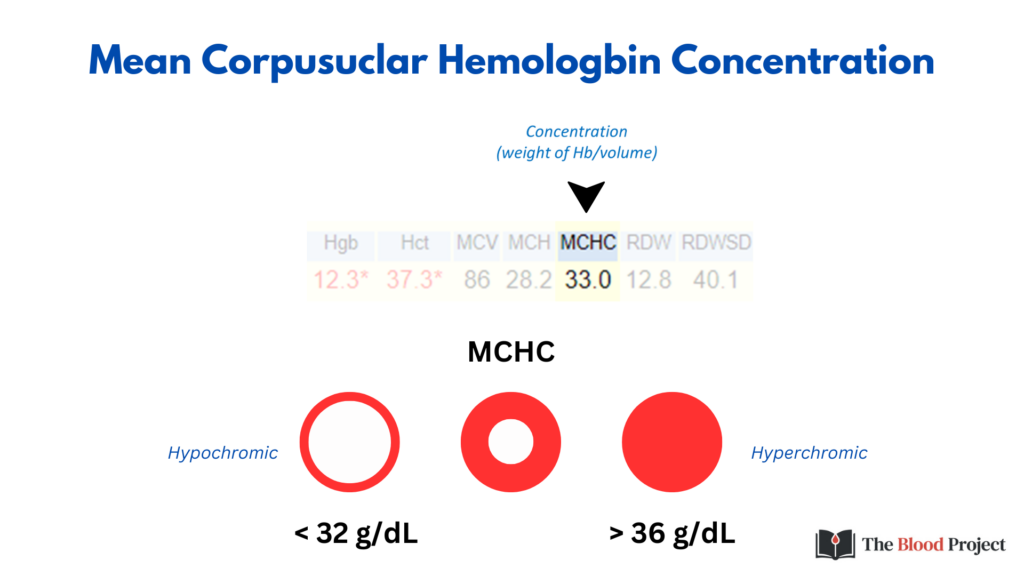
The MCHC can decrease more that it can increase, because the Hb is already supersaturated in the RBC. That’s why an MCHC of 31 g/dL is not that impressive (we can see values as low as 26 g/dL), whereas an MCHC of 37 g/dL is very significant.
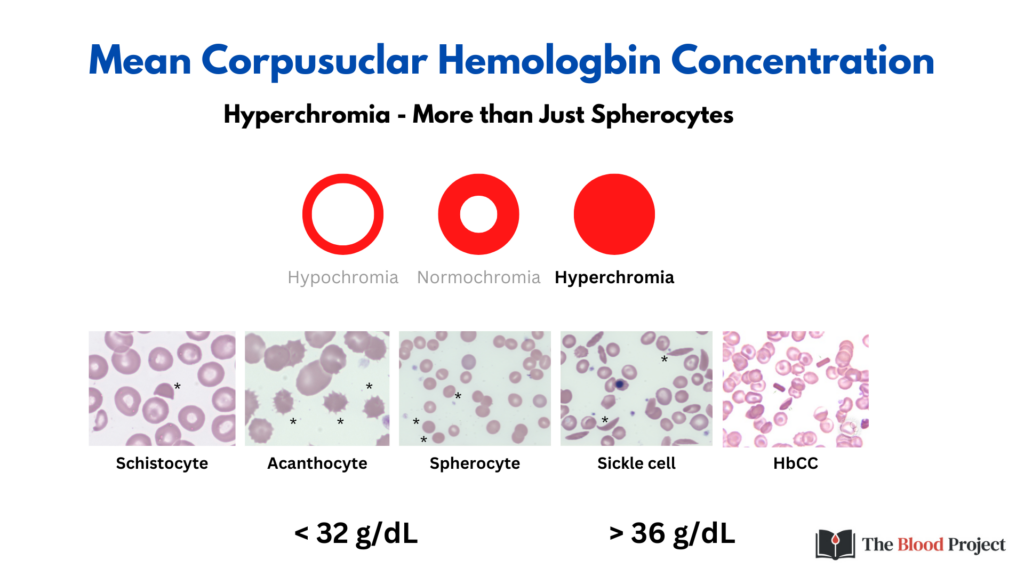
There is a tendency to consider hyperchromia as being synonymous with spherocytosis. However, as shown in this slide there are several other ways to increase the MCHC. Note that in each case, the poikilocyte lacks central pallor.
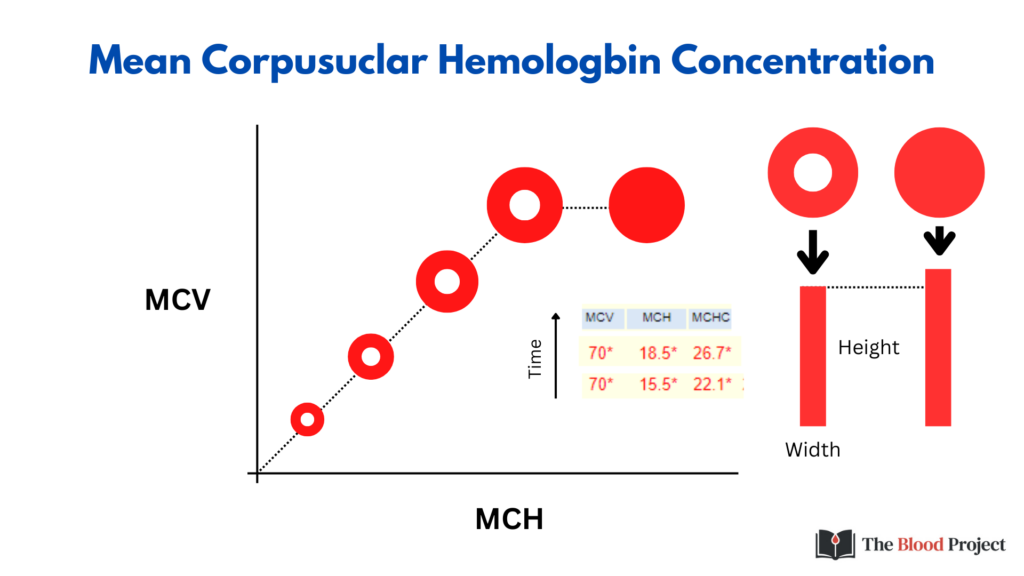
The MCH not only tracks with MCV but also with MCHC.

The first branchpoint in the morphological classification of anemia is the MCV. The second branchpoint is MCHC. When this classification was first proposed by Max Wintrobe, a normal and low MCHC were used to differentiate causes of microcytic anemia. As we will see, the classification can be expanded to include hypochromic, normochromic and/or hyperchromic subcategories of microcytic, normocytic and/or macrocytic cells.
