Case TTP
Hematology consult note:
Ms. X is a 27-year-old woman who is 20 weeks pregnant who presents with thrombocytopenia and anemia. She has been feeling unwell with a headache and was concerned for a viral infection for which she presented to the CHA ED. She complained of R sided facial numbness. She was found to have hgb 5.1 and plt 5. She was transferred to BIDMC for further evaluation. Here she was found to have similar labs. She is hemodynamically stable and has no signs of bleeding. Her pregnancy has been relatively uncomplicated. Hematology was called for the concern for TTP.
The answer to these questions was no. The physical exam was unremarkable except for gravid uterus.
True or false: TTP rarely occurs at 20 weeks’ gestation. Patients typically present in the first trimester.
Here is the patient’s CBC, WBC differential and reticulocyte count at presentation:


What are two buckets of causes of elevated reticulocyte count in the setting of anemia?
Click for Answer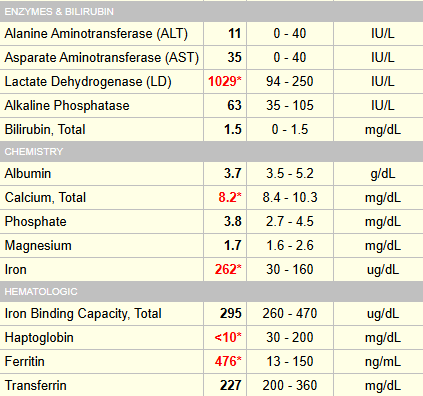
Let’s take a look at the peripheral smear:

What does the smear show?
Let’s look at more lab data at admission:


Renal function and liver function normal, arguing against aHUS or HELLP.
Hematology progress note (day 2):

The patient presented with headache and facial numbness. A CT head was ordered, which was normal:

Have any of the clinical prediction scores (PLASMIC score, French score) been validated for pregnant women?
Ferrari and Flora: “In practice, when we are facing a previously healthy pregnant woman with biochemical features of acute TMA with severe thrombocytopenia (especially <30 000/mL) and absent-to-mild renal and hepatic involvement (creatinine < 2 mg/dL, AST/alanine aminotransferase (ALT) <2x ULN), especially if neurological impairment is present in the absence of hypertension, we assume acute TTP until proven otherwise, and we start the appropriate treatment as soon as possible if the fetal parameters are not life threatening”.
This patient fits the bill and should treated for presumed TTP.
Which of the following therapies should be started as soon as possible:
True or false: early delivery is key to treating TTP in pregnancy.
Which of the following blood product(s) is/are relatively contraindicated in TTP:
Maternal fetal medicine (day 1):

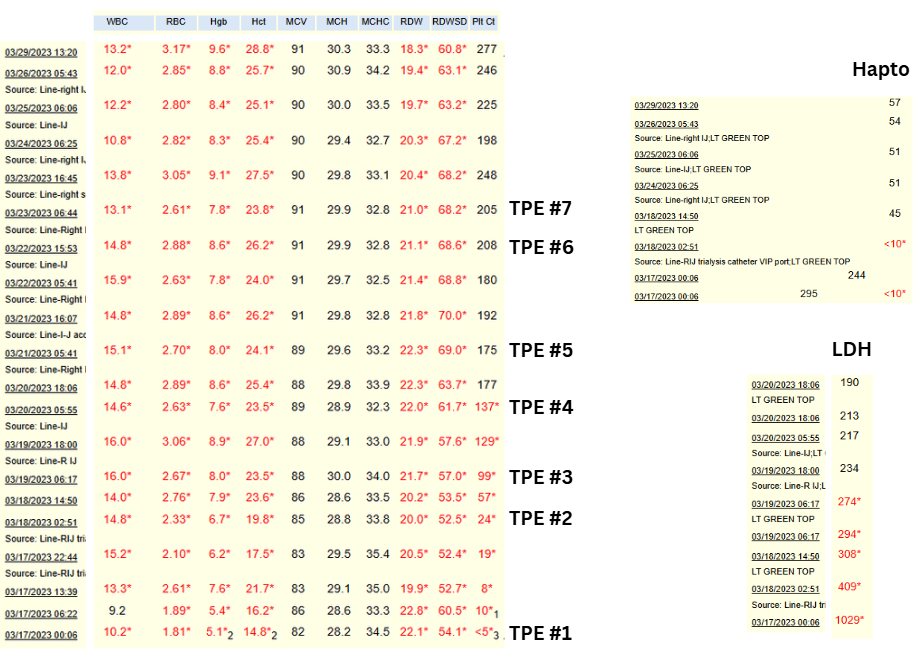
Time series of CBC, haptoglobin and LDH while in hospital:
Results of ADAMTS13 activity level (came back on day 5):

Are these results consistent with a diagnosis of TTP?
TTP, as defined by ADMTS13 activity level < 10%, may be hereditary (congenital) or acquired (immune).
True or false: virtually all cases of TTP presenting during pregnancy are congenital.

The patient was discharged after 9 days (7 sessions of therapeutic plasma exchange) on prednisone 60 mg daily (tapered down to 15 mg at time of delivery), aspirin 81 mg daily. Per hematology note:
- “Weekly hematology follow-up for now”
- “Defer rituximab due to limited data w/ regard to safety in pregnancy. We could consider this if a future relapse occurs.”
Repeat ADAMTS13 activity levels:

She delivered a healthy baby boy at 36 weeks gestation without evidence of recurrence/relapse of TTP.
A year later, the patient comes to see you, stating that she wants to become pregnant again. What do you tell her (more than once answer may apply)?
