Case of polycythemia
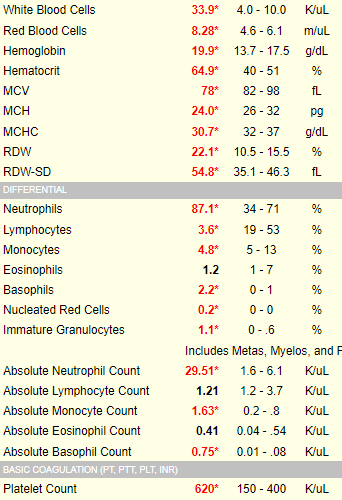
How do we know what qualifies for lower- or higher-than-normal white cell counts? Consult a cheat sheet like this one!
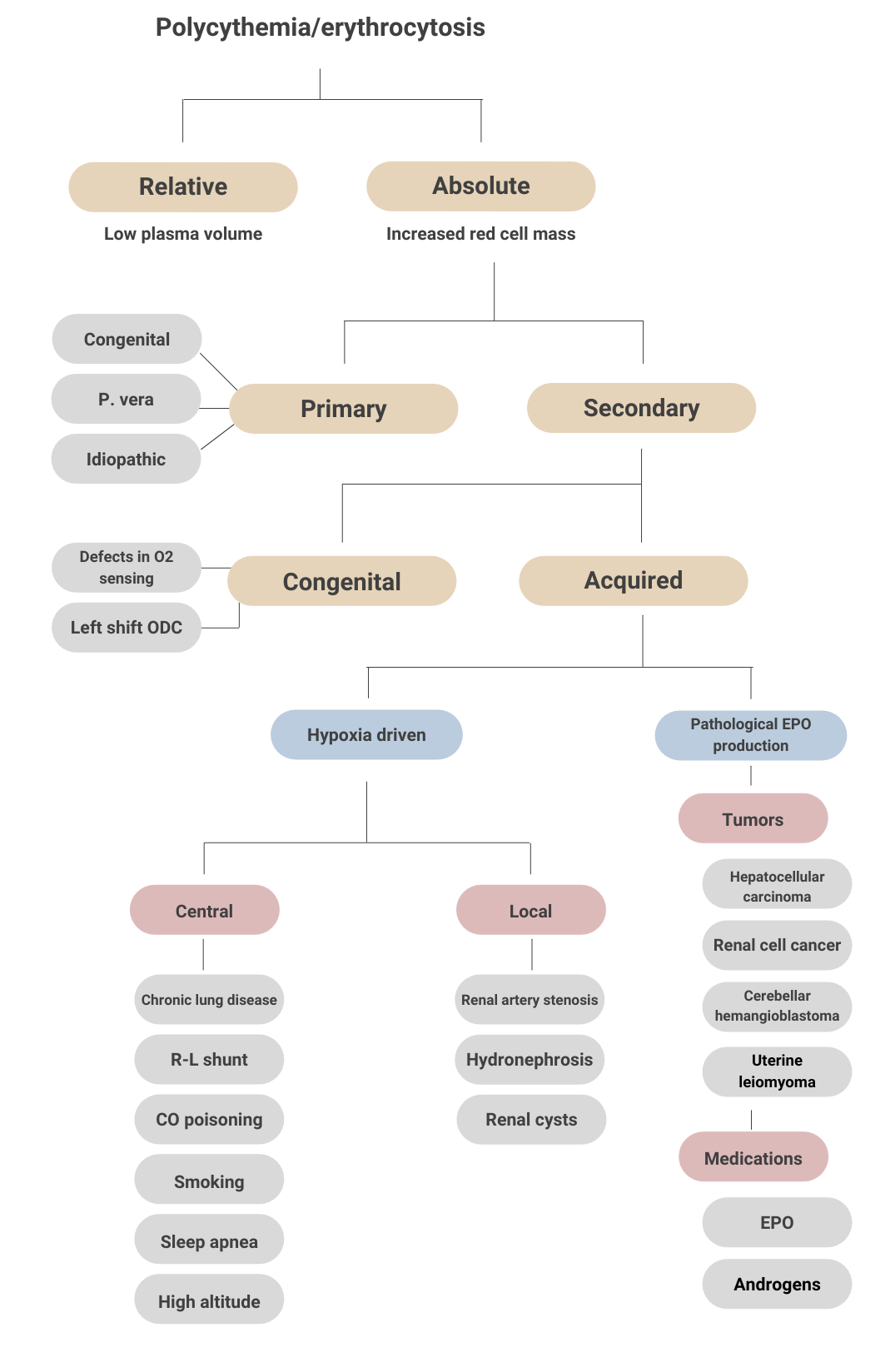
Before we get to the Twitter questions, let’s consider the definition and classification/differential diagnosis of polycythemia:
Definitions
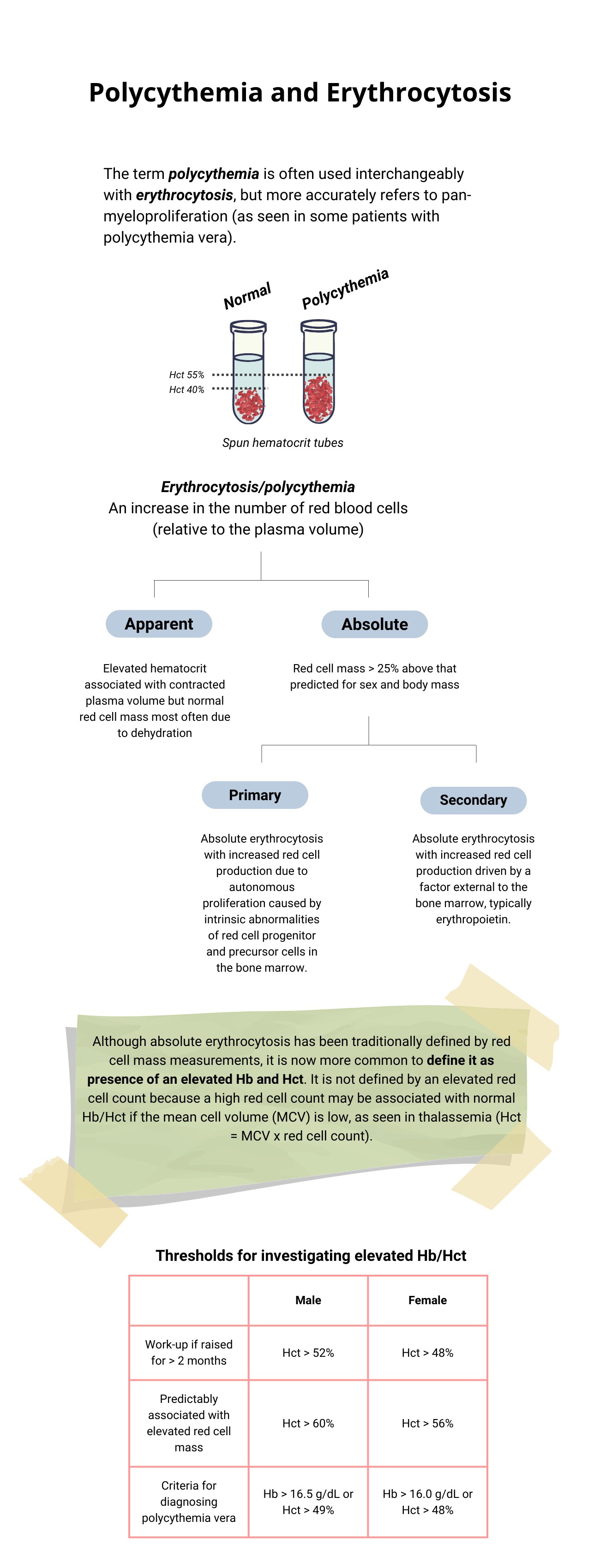
Classification
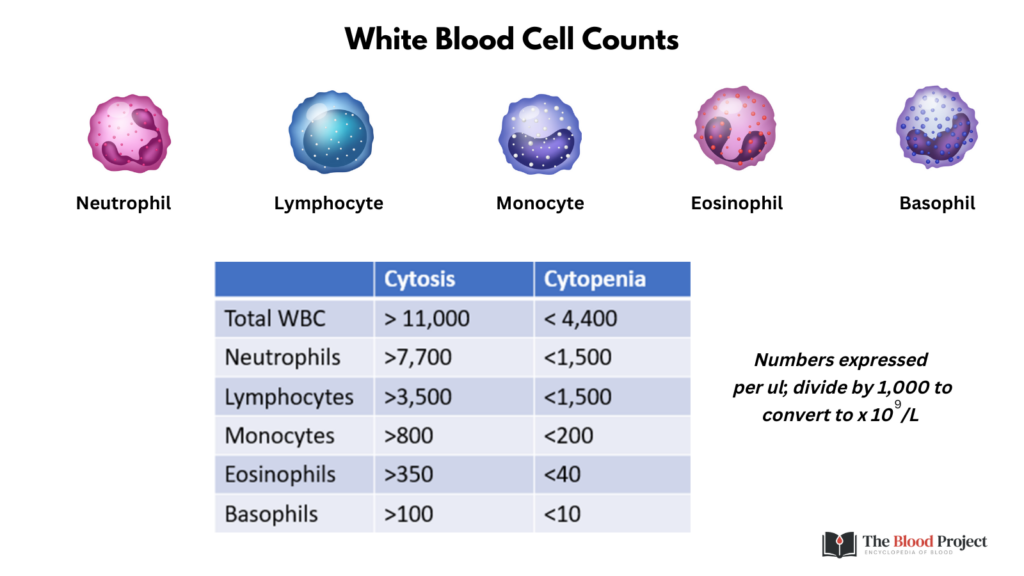
At this point, what is the likeliest diagnosis?
Twitter questions:
- What skin symptom might the patient complain of?
- Why does the patient have a ruddy complexion?
- Is this patient or one with anemia more likely to develop cyanosis at a given SaO2?
- What is the PT and aPTT likely to be?
- Why is the LDH elevated?
- What is the one highest-yield test to order?
Aquagenic pruritus (AP):
- Debilitating dermal condition characterized by the development of intense itching, stinging, tingling or burning sensations, without observable skin lesions, precipitated by contact with water at any temperature.
- Typically occurs after a shower with warm water.
- One of the common symptoms in polycythemia vera (PV).
- In cohort of 1,545 of patients diagnosed with PV according to WHO definition, pruritus in 36% at diagnosis and during median 6.9 years of follow-up.
- Pathogenesis likely involves role of mast cells and basophils.
- Can precede, be concomitant with, or follow diagnosis of PV.
- Has significant influence on patients’ quality of life and personal hygiene.
Twitter questions:
- What skin symptom might the patient complain of?
- Why does the patient have a ruddy complexion?
- Is this patient or one with anemia more likely to develop cyanosis at a given SaO2?
- What is the PT and aPTT likely to be?
- Why is the LDH elevated?
- What is the one highest-yield test to order?
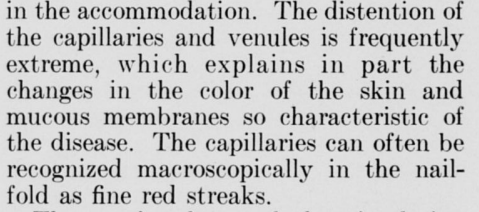
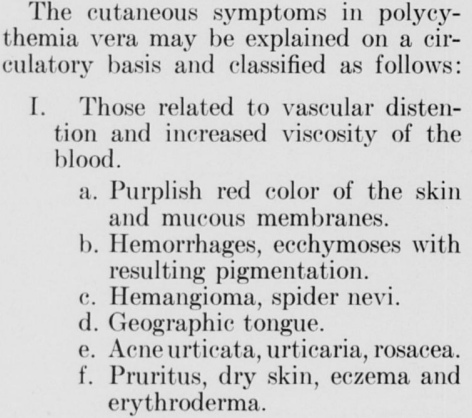
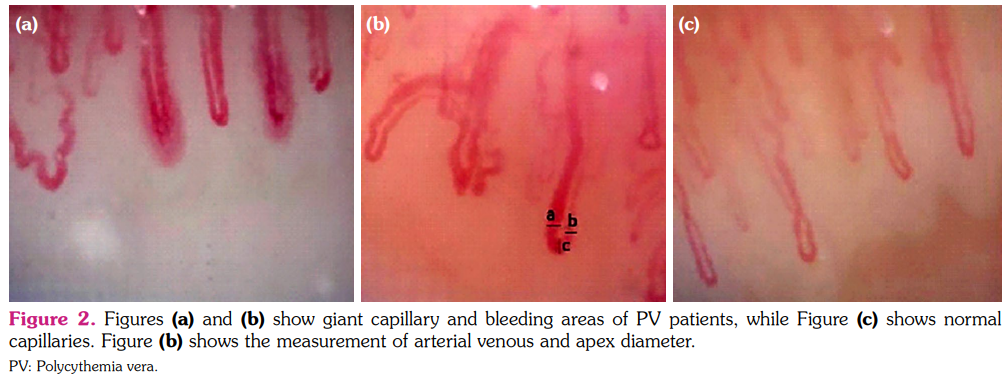
The color of the skin in cases of polycythemia vera is due largely to:
- The large increase in the circulating red blood cells and hemoglobin.
- The number of capillaries for each unit area of skin.
- The degree of vasodilation of skin microvessels.

What is the hemodynamic advantage of vasodilation in a patient with polycythemia vera?
Click for Answer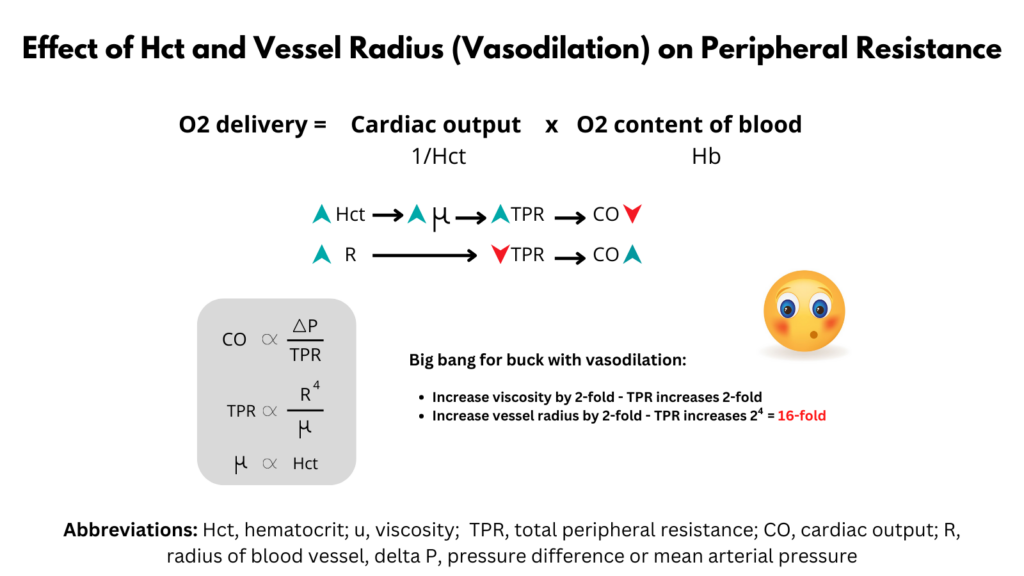
Twitter questions:
- What skin symptom might the patient complain of?
- Why does the patient have a ruddy complexion?
- Is this patient or one with anemia more likely to develop cyanosis at a given SaO2?
- What is the PT and aPTT likely to be?
- Why is the LDH elevated?
- What is the one highest-yield test to order?

Is this patient or one with anemia more likely to develop cyanosis at a given SaO2?
Click for AnswerCyanosis:
- Clinical manifestation of bluish discoloration of skin or mucosa resulting from the presence of deoxygenated hemoglobin within the superficial dermal capillaries, subpapillary venous plexus and mucous membranes (not the deeper arteries and veins).
- Sometimes difficult to detect clinically due to factors such as skin color, dermal thickness, exposure to light, presence of jaundice and state of the cutaneous capillaries.
- Best appreciated in areas of the body where the overlying epidermis is thin and the blood vessel supply abundant, including the lips, cheeks, nose, ears, mucous membranes, and nailbeds.
- Classified as:
- Central cyanosis:
- Apparent at the:
- Lips
- Tongue
- Sublingual tissues.
- Results from:
- Reduced arterial oxygen saturation (PaO2)
- Abnormal hemoglobin derivatives (methemoglobin or sulfhemoglobin)
- Causes include:
- Decreased arterial oxygen saturation
- Decreased atmospheric pressure (altitude)
- Impaired pulmonary function
- Pneumonia
- Pulmonary embolism
- Obstructive lung disease
- Pulmonary edema
- Alveolar hypoventilation
- Anatomic shunts
- Hemoglobin abnormalities
- Hemoglobin with low oxygen affinity
- Methemoglobinemia (hereditary or acquired)
- Sulfhemoglobinemia (acquired)
- Decreased arterial oxygen saturation
- Apparent at the:
- Peripheral cyanosis:
- Apparent on the hands and feet but not oral mucosa.
- Results from vasoconstriction and diminished peripheral blood flow, as seen in:
- Reduced cardiac output
- Cold exposure
- Redistribution of blood flow from extremities
- Arterial or venous obstruction
- Central cyanosis:
- Pathophysiology:
- Cyanosis is discernible to the human eye when the deoxygenated hemoglobin (Hb) in the blood > 3-5 g/dL.
- The increased amount of deoxygenated hemoglobin is due to either:
- Increased amount of venous admixture (due to vasodilatory effects on the venous plexi).
- Reduced arterial oxygen tension in the capillaries.
- Note that it is the absolute, not relative, quantity of deoxygenated hemoglobin that determines whether cyanosis is observed. Thus, the level of SaO2 at which cyanosis becomes apparent depends on their total hemoglobin concentration.
- Severely anemic patients with marked arterial desaturation may not have cyanosis.
- Patients with polycythemia develop obvious cyanosis at much higher SaO2.
- For a nice review on cyanosis, click here.
Twitter questions:
- What skin symptom might the patient complain of?
- Why does the patient have a ruddy complexion?
- Is this patient or one with anemia more likely to develop cyanosis at a given SaO2?
- What is the PT and aPTT likely to be?
- Why is the LDH elevated?
- What is the one highest-yield test to order?
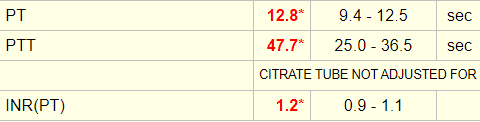
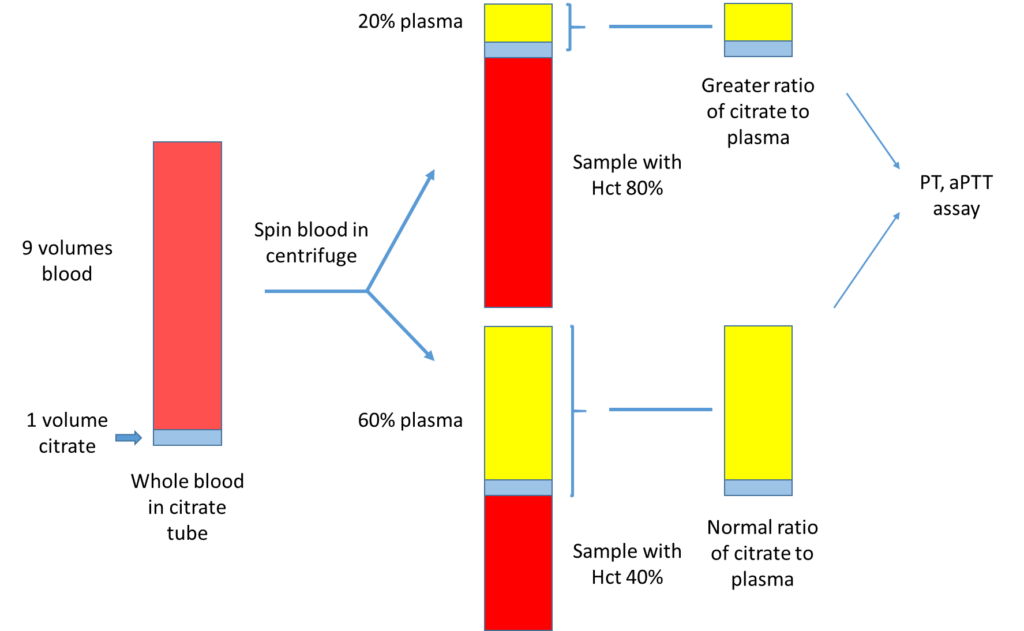
The patient’s initial coagulation screen showed the following:
Twitter questions:
- What skin symptom might the patient complain of?
- Why does the patient have a ruddy complexion?
- Is this patient or one with anemia more likely to develop cyanosis at a given SaO2?
- What is the PT and aPTT likely to be?
- Why is the LDH elevated?
- What is the one highest-yield test to order?
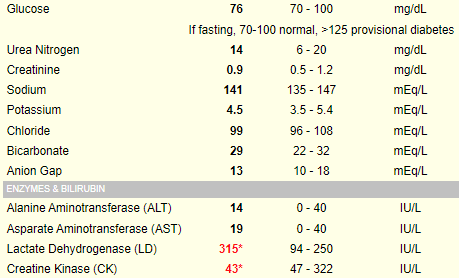
Serum lactate dehydrogenase (LDH) is a surrogate quantitative measure of cell turnover and tumor burden. The following is an abstract that reported the LDH level in 216 patients with polycythemia vera:
Twitter questions:
- What skin symptom might the patient complain of?
- Why does the patient have a ruddy complexion?
- Is this patient or one with anemia more likely to develop cyanosis at a given SaO2?
- What is the PT and aPTT likely to be?
- Why is the LDH elevated?
- What is the one highest-yield test to order?

What single lab test would you like to order to definitively rule in/out polycythemia vera?
Click for AnswerHere are the results of the Jak2 mutations status:
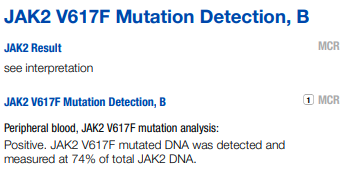
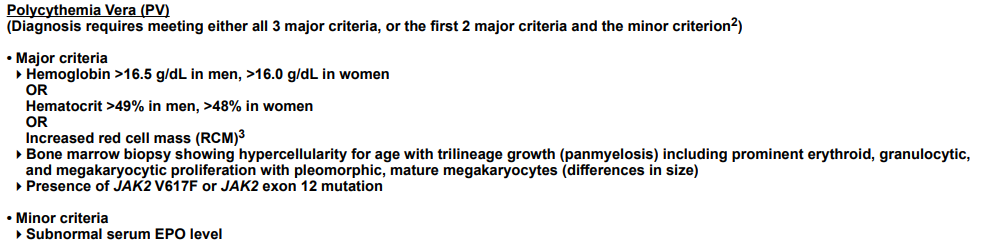
Our patient has 2 major criteria (Hb > 16.5) and presence of Jak2 V617F. For formal diagnosis, he would require a bone marrow biopsy. However, the pretest probability for polycythemia vera is virtually 100% and the patient should be treated accordingly.