About the condition
Description/definition:
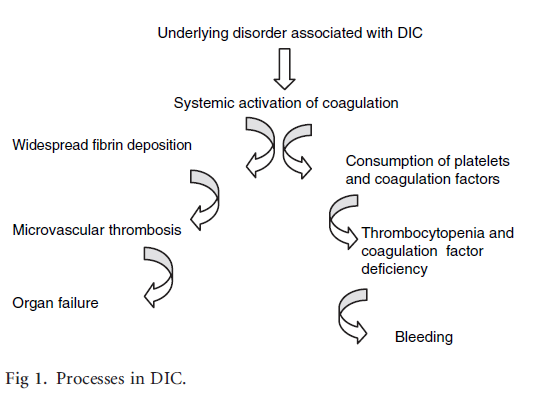
Disseminated intravascular coagulation (DIC) is an acquired clinicopathological syndrome that complicates a range of conditions, such as infection/sepsis, cancer, vascular anomalies, complicated pregnancy, and trauma. DIC is characterized by widespread activation of the clotting cascade and, in some cases, excessive activation of fibrinolysis. Activation of coagulation leads to 1) fibrin clots and vascular damage, which may cause organ dysfunction/failure, and 2) depletion of clotting factors (termed consumptive coagulopathy) and platelets, which may lead to clinically significant bleeding, especially in cases where fibrinolysis is concomitantly hyper-activated (for example in acute promyelocytic leukemia).
Classification of DIC:
According to underlying disease:
- Infection
- Cancer, including acute leukemia
- Vascular anomalies
- Trauma
- Pregnancy
- Heparin-induced thrombocytopenia
According to hemostatic phenotype:
- Hypercoagulable (also called suppressed-fibrinolytic-type) DIC:
- Typically seen in patients with sepsis.
- Characterized by activation of coagulation, minimal activation of fibrinolysis owing to suppression of plasminogen activator inhinbitor-1 (PAI-1).
- Microthrombi are not readily lysed, leading to organ failure.
- Fibrinolytic (also called enhanced-fibrinolytic-type) DIC:
- May occur in:
- Acute promyelocytic leukemia (APL)
- Aortic aneurysms
- Giant hemangioma
- Placental abruption
- Metastatic prostate cancer
- Characterized by marked fibrinolytic activity compared with lesser activation of coagulation.
- Excessive lysis of fibrinogen/fibrin results in serious bleeding; organ failure rarely seen.
- May occur in:
According to chronicity:
- Acute (decompensated) – typically seen in settings such as sepsis, trauma, or acute promyelocytic leukemia.
- Chronic (compensated) – typically seen in patients with advanced cancer, including pancreatic, gastric, ovarian, and brain tumors.
According to clinical phase:
- Non-overt DIC (latent DIC or compensated DIC)
- Overt DIC (non-compensated or decompensated DIC)

Pathophysiology:
DIC is initiated by tissue factor-mediated activation of the clotting cascade. The source of tissue factor varies according to the etiology of the DIC. For example, In sepsis, tissue factor is upregulated in circulating activated monocytes, while in trauma, tissue factor, already present in the blood vessel wall, is exposed to circulating factor VII. The up-regulation of tissue factor activates coagulation, which overcomes natural anticoagulant control mechanisms (protein C/S, antithrombin, and tissue factor pathway inhibitor), leading to the widespread deposition of fibrin and microvascular thromboses, which may, in turn, contribute to multiple organ dysfunction. In addition to upregulating tissue factor, DIC may result in either suppression or hyper-activation of fibrinolysis. Finally, some types of DIC, for example DIC associated with sepsis, also leads to reduced expression/activity of natural anticoagulants, including protein C and antithrombin. The relative activities of tissue factor, fibrinolysis and natural anticoagulants determine the clinical phenotype (organ failure vs. bleeding).
| Cause of DIC | Mechanism of coagulation activation |
|---|---|
| Trauma | Trauma-associated vessel wall dysfunction; systemic inflammatory mediators; release of tissue debris containing tissue factor, especially in patients with cerebral trauma. |
| Placental abruption | Systemic release of thromboplastin (tissue factor) from placental or amniotic sources into the maternal circulation. |
| Malignant disease | Expression of procoagulant components by tumor cells. |
| Large vascular abnormalities | Local hemostatic activation overflowing in the systemic circulation accompanied by massive release of plasminogen activators from disrupted endothelial cells. |
| Giant hemangiomas | Massive release of large multimeric von Willebrand factor may cause enhanced platelet-vessel wall interaction leading to thrombotic microangiopathy. |
| Sepsis | Tissue factor induction on circulating monocytes; systemic inflammatory mediators (inflammatory cytokines and chemokines). |

Diagnosis:
There is no single blood test for diagnosing DIC. The use of clinical prediction tools is recommended by clinical practice guidelines. It is important to repeat testing on a regular basis, since DIC is a rapidly evolving condition. Several scoring systems have been published. The following is from the ISTH:
| Parameter | Score | Comment |
|---|---|---|
| Fibrinogen (g/L) | >1 (0) <1 (1) | Overall sensitivity of low fibrinogen level reported to be about 30%. |
| Prothrombin time (PT) (seconds) | <3 (0) 3-6 (+1) >6 (+2) | Elevated in 50%-60% of patients with DIC at some point during course of illness. |
| Platelet count (109/L) | >100 (0) 50-100 (+1) <50 (+2) | Thrombocytopenia reported to occur in up to 98% of DIC cases. |
| D-dimers or FDPs | No increase (0) Moderate increase (+2) Severe increase (+3) | Elevated FDPs and D-dimers are sensitive, but not specific for DIC. |

Differential diagnosis:
| Diagnosis | PLT count | PT | aPTT | Fibrinogen |
|---|---|---|---|---|
| DIC | Decreased | Increased | Increased | Decreased |
| TTP | Decreased | Normal | Normal | Normal |
| HUS | Decreased | Normal | Normal | Normal |
| Cirrhosis | Decreased | Increased | Increased | Low or normal |
| ITP | Decreased | Normal | Normal | Normal |
| HIT | Decreased | Normal | Normal | Normal |

Treatment:
Three general principles of management:
- Treatment of underlying condition
- Replacement therapies
- Therapies that inhibit thrombin generation (and therefore fibrin deposition)
Treatment of underlying condition:
- Antibiotics and source control for sepsis-induced DIC
- ATRA in patients with APL
- Surgery for patients with trauma
- Delivery for patients with obstetrical DIC
Replacement therapies:
- Blood component therapy should not be used to treat numbers. They should only be given if patient is bleeding or is at high risk of bleeding.
- Platelet transfusions:
- Therapeutic if active bleeding and platelet count < 50 x 109/L.
- Prophylactic if platelet count < 20 x 109/L.
- Fresh frozen plasma (FFP):
- If prolonged PT/aPTT (>1.5x normal) and one of:
- Active bleeding
- Requirement for invasive procedure
- If prolonged PT/aPTT (>1.5x normal) and one of:
- Cryoprecipitate or fibrinogen concentrate – if active bleeding with persistently low fibrinogen (<1.5 g/L) despite FFP replacement.
- Prothrombin complex concentrate (PCC) may be considered if FFP not available for actively bleeding patients.
- Heparin:
- No randomized trials examining efficacy of heparin in patients with DIC.
- Therapeutic doses should be considered in cases of DIC where thrombosis predominates.
- All patients should receive heparin prophylaxis.
- Anticoagulant factor concentrates:
- Use outside of clinical studies is mostly restricted to purpura fulminans (a specific type of DIC associated with reduced protein C activity and extensive skin lesions).
- Agents include:
- Antithrombin
- Recombinant human thrombomodulin
- Protein C

Prognosis:
Major bleeding reported in 5%-12% of patients with DIC. Risk is 5-fold higher in those with platelets < 50 x 109/L.
Among critically ill patients with DIC, reported 28-day mortality 20%-50%.
Among patients with sepsis and DIC, mortality reported to be about 2 times higher than those without DIC.

