One more physiological consideration
We often use the hemoglobin (Hb) and hematocrit (Hct) interchangeably when discussing and considering patients.
Let’s see how the Hb and Hct affect oxygen delivery:
Oxygen delivery = cardiac output x oxygen content of blood
- As we discussed earlier in the case, Hct affects blood viscosity, which increases total peripheral resistance and reduces cardiac output.
- Hb, by contrast, increases the oxygen content of blood.
As Hb increases, so too does Hct (that is the price paid for packaging Hb inside red cells). Therefore as oxygen content increases, cardiac output decreases. This relationship can be illustrated in the following schematic:
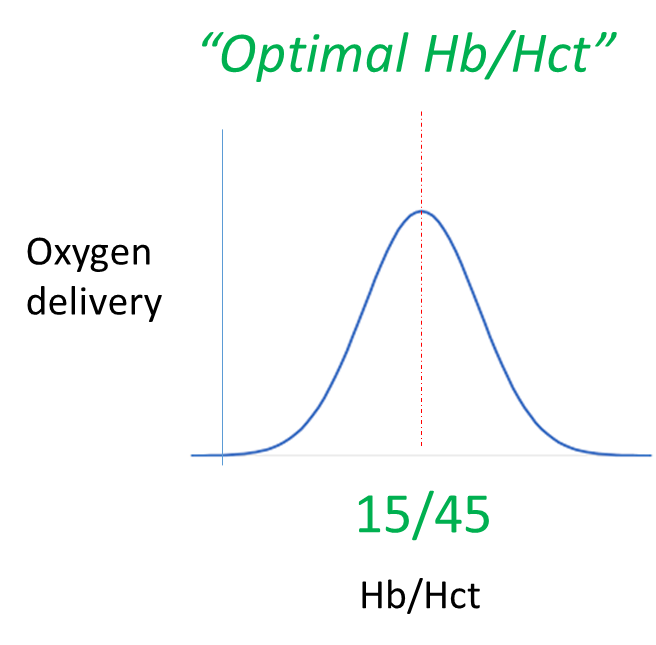
When patients deviate to the left of the optimal Hb/Hct (anemia), the Hb (and oxygen carrying capacity of blood) is limiting, so it makes sense to talk about the hemoglobin.
On the other side of the hill are those rare patients with polycythemia. In this case, Hct/viscosity are limiting and the goal of therapy is to reverse course and pull the patient back to the summit (hill top) using phlebotomy or myelosuppressive agents.

