Labs
The following is the complete blood count (CBC) when the patient was first seen in the emergency room:
| WBC (109/L) | Hb (g/dL) | Hct (%) | MCV (fL) | PLT (109/L) |
|---|---|---|---|---|
| 33.9 | 20.8 | 69.3 | 81 | 632 |
What’s what: WBC, white blood cell count; Hb, hemoglobin; MCV, mean cell volume; MCHC, mean cellular hemoglobin concentration; RDW-SD, red cell distribution width-standard deviation; platelets, PLT; Normal values: WBC 5-10 x 109/L, RBC 4-6 x 1012/L, Hb 12-16 g/dL, Hct 35-47%, MCV 80-100 fL, MCHC 32-36 g/dL, RDW-SD < 45 fL, platelets (PLT) 150-450 x 109/L











If the patient’s mean cell volume was 95 fL six months ago, what would you be suspicious of today?
Click for AnswerThe following is a complete blood count from an individual with beta thalassemia. Note the increased red cell count, with a normal hematocrit (Hct). Hct = mean cell volume x red cell count, so if the red cells are small, as in this case, the bone marrow compensates by producing more of them to maintain a normal Hct. This condition used to be called microcytic erythrocytosis!
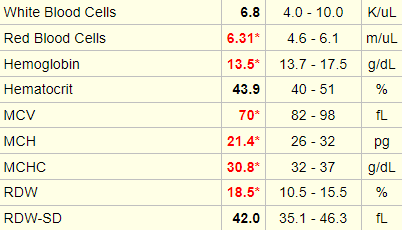
Our patient has elevation in all three cell lines: white cells, red cells and platelets. While we now use the term polycythemia to describe the red cells (and their effect on the Hct) alone, it was originally coined to describe a pan-increase in all three cell types (hence the qualifier poly).
Based on these lab values, what is the most likely diagnosis?
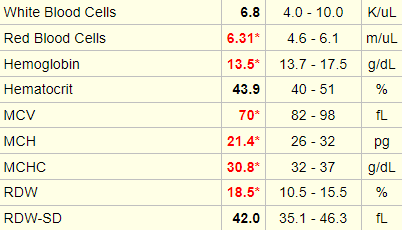
Let’s look at the white cell differential:
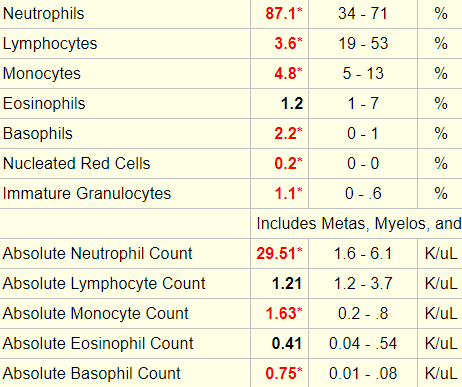
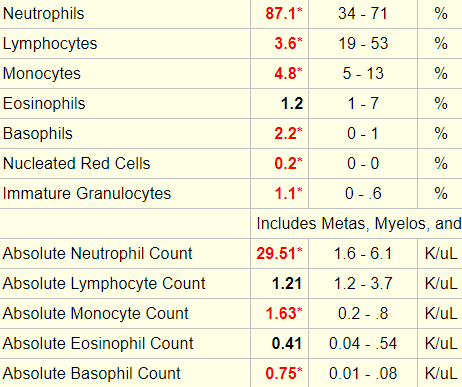


The following is “cheat sheet” of ranges that define lower- or higher-than-normal counts:
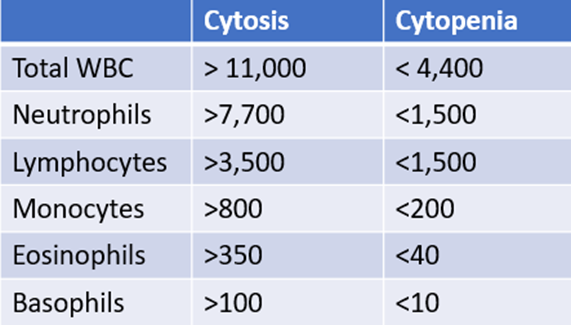











Why are the white cell counts and platelet count often elevated in polycythemia vera
Click for AnswerWhich additional lab tests would you predict might be abnormal (more than one answer may apply)?
The patient had a uric acid of 10.2 mg dL (normal 3.4-7.0 mg/dL).
High uric acid (complicated by gout and kidney stones) is associated with polycythemia vera due to the high turnover of red blood cells, which results in higher-than-normal uric acid production.
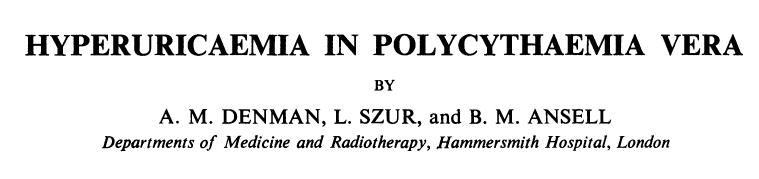
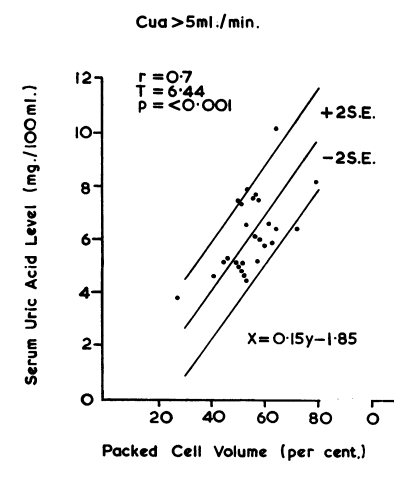
As mentioned under the Physical Exam, the patient was seen by rheumatology who diagnosed her with crystal-proven gouty arthritis of the left elbow. She was treated initially with colchicine and NSAIDs and was subsequently started on allopurinol.
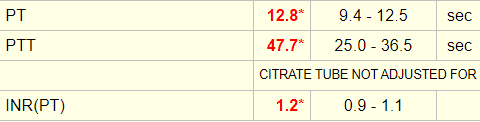
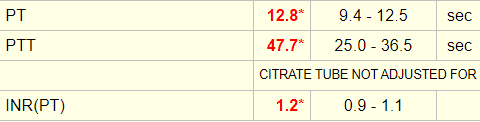
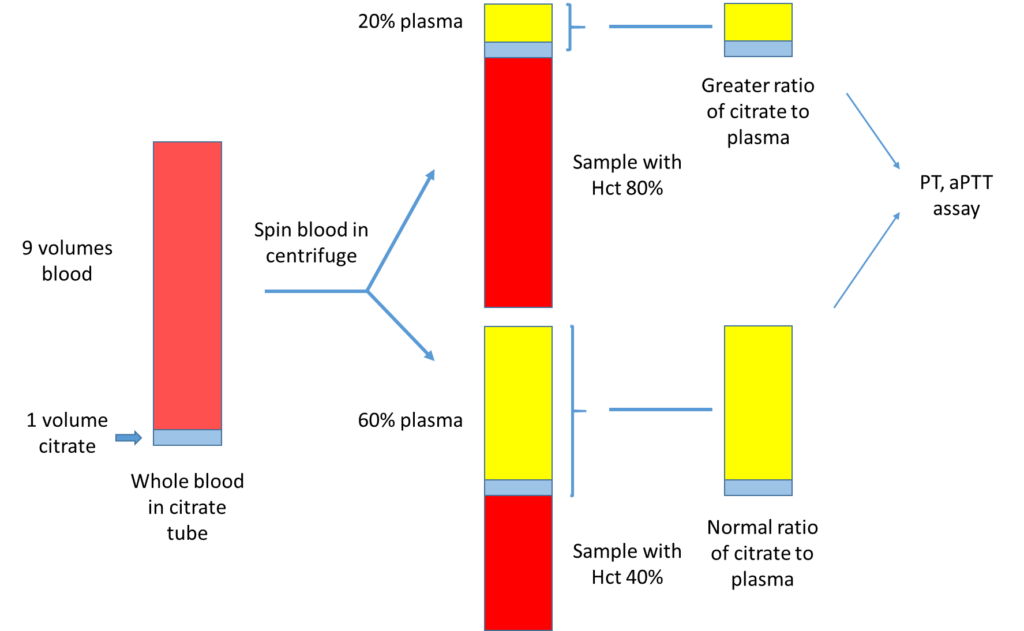
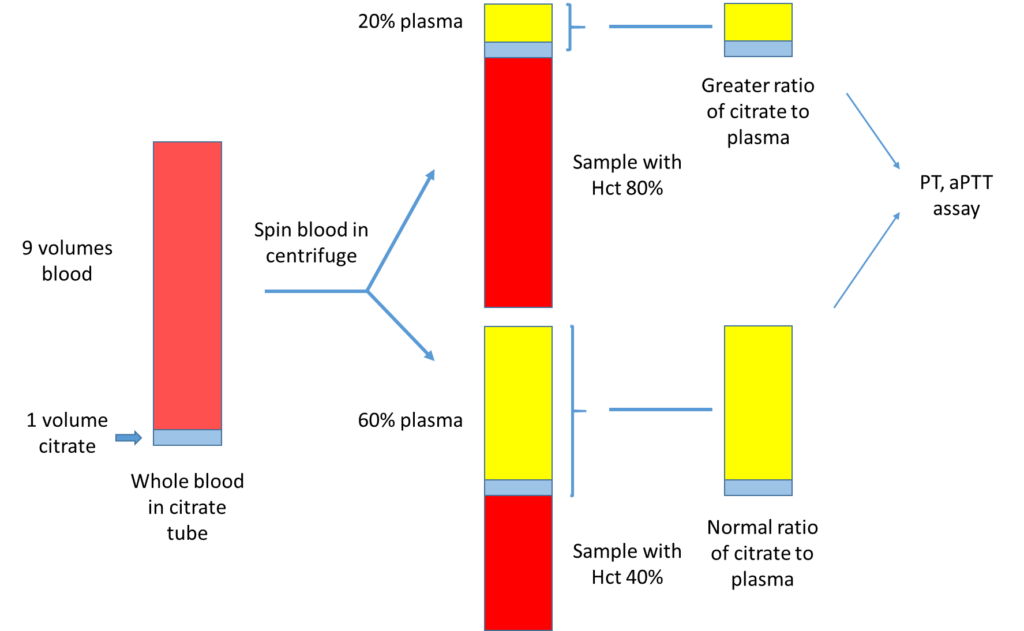
The patient’s initial coagulation screen showed the following:
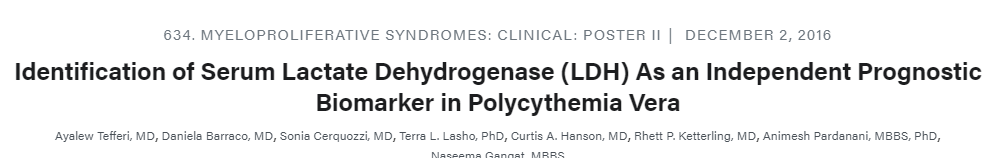
The patient had a serum lactate dehydrogenase (LDH) of 315 IU/L (normal 94-250 IU/L).
Serum lactate dehydrogenase (LDH) is a surrogate quantitative measure of cell turnover and tumor burden. The following is an abstract that reported the LDH level in 216 patients with polycythemia vera:











What single lab test would you like to order to definitively rule in/out polycythemia vera?
Click for AnswerFor more information on Jak2 V617F, click here.
The Jak2 mutation was ordered when the patient was first seen, but this test takes several days to come back, so treatment decisions had to be made without knowledge of the result.
When the test result did return, it showed the following:
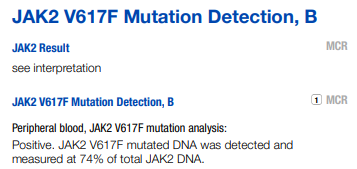
Is the Jak2 V617F mutation specific to polycythemia vera?
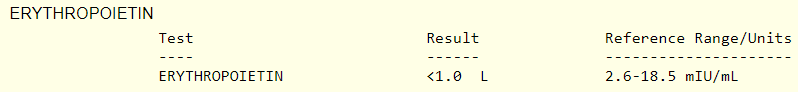
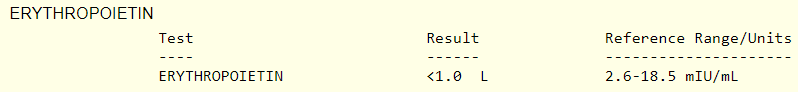
Another test that is commonly ordered in patients with polycythemia is a serum erythropoietin. What do you predict the serum erythropoietin will be in this case?
The erythropoietin level was undetectable!
Does the patient have polycythemia vera? Can this diagnosis be made prior to the Jak2 mutation result? To address this question, we need to consider the diagnostic criteria for polycythemia vera.
Diagnosis requires meeting either all 3 major criteria, or the first 2 major criteria and the minor criterion:
Major criteria
- Hemoglobin > 16.5 g/dL (male), > 16 g/dL (female), or either of:
- Hematocrit > 49% (males), > 48% (women).
- Other evidence of increased red cell volume.
- Bone marrow biopsy with hypercellularity for age with panmyelosis with prominent erythroid, granulocytic, and megakaryocytic proliferation.
- JAK2 V617F or other mutation of similar function (for example, JAK2 exon 12 mutation).
Minor criteria
- Serum erythropoietin level below normal reference range.
You will note that without the JAK2 V617F mutation status, and without a bone marrow biopsy, the patient does not formally meet the criteria for diagnosis of polycythemia vera. But in a case like this (extreme elevation in the Hct, elevated white cells and platelets, basophilia and an absence of any obvious secondary cause for the polycythemia), the pretest probability of polycythemia vera is so high that is should be treated as such, pending the results of the complete work-up.
