Considerations Prior to Seeing the Patient
What we know so far:
- 68 year-old woman with extreme thrombocytosis (defined below)
- Inpatient setting
Definitions:
- Thrombocytosis = platelet count > 450 x 109/L
- Extreme thrombocytosis = platelet count > 1000 x 109/L
Patients with extreme thrombocytosis are sometimes called “platelet millionaires”. Why? Because the platelet count in extreme thrombocytosis can be written in one of two ways:
- > 1000 x 109/L
- > 1 x 106/microliter (ul) or > 1 million/ul
What is the most important question to address from an etiologic standpoint?
Without knowing anything else about the patient, what is the most likely diagnosis?
Correct. Secondary (reactive) thrombocytosis accounts for 80% of cases of thrombocytosis (including those with platelet counts >1000 x 109/L).
What is the mechanism underlying primary thrombocytosis?
What is the mechanism underlying secondary thrombocytosis?
MECHANISMS OF THROMBOCYTOSIS
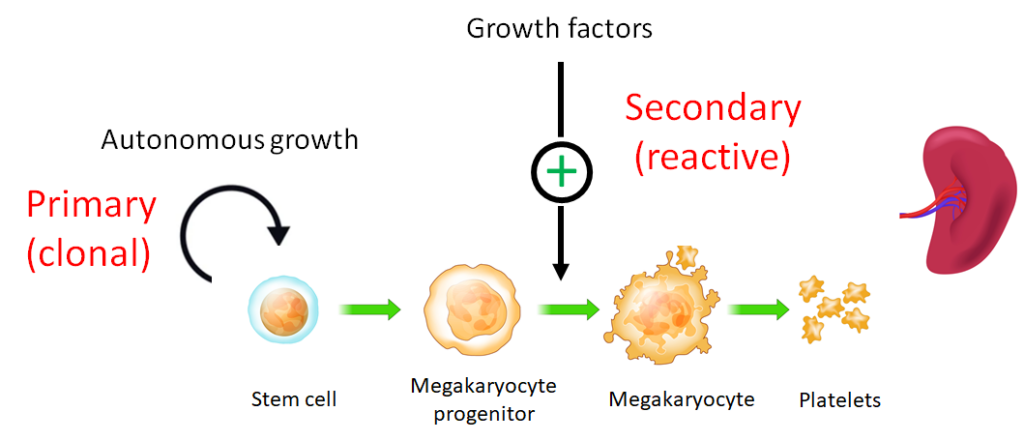
What is the main growth factor that controls proliferation of megakaryocytes and the platelet count?
Can stimulate megakaryocyte growth in vitro.
True or false: if you were to find that the patient’s thrombocytosis was longstanding (say it was present for months or years before admission to hospital), the diagnosis is, by definition, primary, not secondary thrombocytosis.
True or false: secondary thrombocytosis resolves when the underlying causative condition is addressed.
As you prepare to see the patient, you are now armed with information that she has extreme thrombocytosis and you have considered the possibility that the elevated platelet count may be primary (autonomous, clonal) or secondary (reactive to extracellular signals). Beyond diagnostic considerations, what are your most pressing concerns for the patient (more than one answer may apply)?
Before taking a history, it helps to consider the questions you will ask the patient. Such questions are guided by the differential diagnosis of thrombocytosis. To that end, which of the following question(s) is/are relevant?
Yes, iron deficiency is a common cause of secondary (reactive) thrombocytosis, though typically with platelet counts < 1000 x 109/L.
What are some other causes of secondary (reactive) thrombocytosis?
Below is a table of representative symptoms associated with different underlying causes of secondary thrombocytosis:
| Cause of secondary thrombocytosis | Symptoms |
|---|---|
| Bleeding | Melena, hematochezia, surgical blood loss, traumatic blood loss, hemoptysis, hematuria, epistaxis, menorrhagia, hematoma. |
| Hemolysis | Jaundice, history of gall stones, red or dark colored urine, history of extracorpuscular or intracorpuscular causes of hemolysis. |
| Iron deficiency | History of iron deficiency or supplementation, bleeding history, pica, hair loss, brittle nails, restless legs. |
| Asplenia | History of splenectomy or sickle cell disease. |
| Infections | History of chronic infections, especially abscesses and empyema. |
| Inflammatory disorders | History or symptoms of inflammatory bowel disease or rheumatological disorders. |
| Surgery | Recent surgery. |
| Drugs | Use of thrombopoietin receptor agonists, epinephrine, glucocorticoids. |
| Cancer | Focal or constitutional symptoms. |
Regarding primary thrombocytosis, which of the following questions is/are relevant?
Now you are ready to see the patient!
