About the Condition
Description/definition:
Thrombocytosis is defined as a platelet count > 450 x 109/L (some labs consider a threshold platelet count of > 400 x 109/L as qualifying for thrombocytosis).
Classification of thrombocytosis:
Spurious – Counting of nonplatelet structures in the peripheral blood by automated counters resulting in high platelet count.
Primary – 15% of cases:
- Familial:
- Intrinsic – mutations of genes within the megakaryocytic lineage (e.g., thrombopoietin receptor).
- Extrinsic – mutations of genes outside the megakaryocytic lineage (e.g. thrombopoietin).
- Acquired:
- Essential thrombocythemia
- Other myeloproliferative neoplasms
- Myelodysplastic syndrome:
- MDS/MPN-RS-T
- del (5q-)
Secondary – 85% of cases:
- Bleeding
- Hemolysis
- Cancer
- Infections
- Inflammatory disorders
- Iron deficiency
- Asplenia
- Drugs
- Tissue injury:
- Trauma
- Surgery

Prevalence:
| Cause | Griesshammer et al, 1999 | Bess et al, 1994 | Hsieh et al, 2019 |
|---|---|---|---|
| 732 adult in-patients and outpatients; platelet count > 500 x 109/L | 280 adult patients with platelet count > 1,000 x 109/L | 305 adult patients with platelet count > 1,000 x 109/L* | |
| Primary | 12% | 14% | 11% |
| Secondary | 88% | 86% | 69%** |
| Tissue damage | 37% | 14% | NM |
| Infection | 21% | 31% | 9% |
| Cancer | 11.6% | 14% | 28% (heme malignancy); 1.6% had newly diagnosed non-heme malignancy |
| Chronic inflammation | 9% | 9% | NM |
| Renal disorders | 2% | NM | NM |
| Post-splenectomy | 1.6% | 19% | 2% |
| Iron deficiency | NM | NM | 0.3% |
| Medications | NM | NM | 6.2% |
| Blood loss | NM | 6% | NM |
| Surgical complications | NM | NM | 54% |
| Multifactorial | NM | NM | 79.3% |
- The patient in this case developed thrombocytosis following cardiac bypass surgery. How common is this occurrence?
- In a cohort of 297 patients undergoing cardiac bypass surgery:
- 20% reported to develop thrombocytosis
- Typically occurred one week after operation
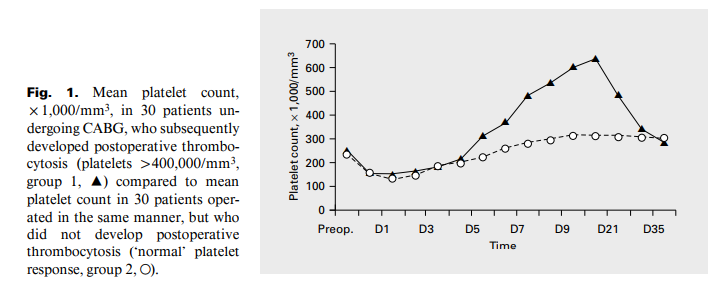
- In another study of 30 patients undergoing cardiac bypass surgery who developed thrombocytosis (platelet count >500 x 109/L), thrombocytosis developed at mean day 6 and peaked on day 14 (see figure).
- In a cohort of 297 patients undergoing cardiac bypass surgery:

Pathophysiology:
| Cause of thrombocytosis | Pathophysiology |
|---|---|
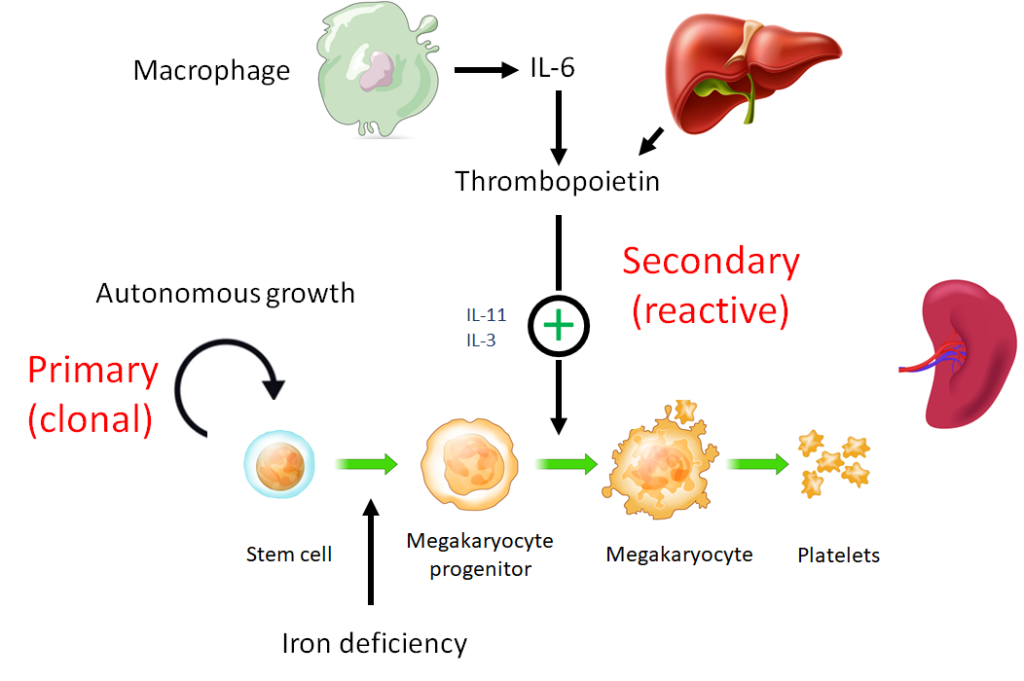
| Primary thrombocytosis | Mutations in driver genes such as Jak2, MPL (thrombopoietin receptor) and CALR. |
| Secondary thrombocytosis | |
| Iron deficiency | Increased commitment of mixed lineage progenitor cells to megakaryocytes. |
| Asplenia | Loss of platelet sequestration, reduced platelet destruction (increased platelet lifespan). |
| Surgery | Overshoot from thrombopoietin response to platelet dilution and consumption (learn more here). |
| Infections | Macrophage-derived cytokines, especially interleukin-6, increase thrombopoietin levels, which in turn increase platelet numbers. |
| Inflammatory disorders | Macrophage-derived cytokines, especially interleukin-6, increase thrombopoietin levels, which in turn increase platelet numbers. |
| Cancer (highest prevalence in colorectal and mesothelioma) | Macrophage-derived cytokines, especially interleukin-6, increase thrombopoietin levels, which in turn increase platelet numbers. |

Clinical presentation:
Thrombocytosis may be found while evaluating other clinical findings or as an incidental finding on a complete blood count. Primary thrombocytosis is more likely if:
- Unexplained vasomotor symptoms (eg, erythromelalgia, flushing, pruritus).
- Constitutional symptoms (eg, unexplained fever, sweats, or weight loss) and/or splenomegaly.
- Thrombosis at unusual sites or unprovoked or recurrent thrombosis without other explanation.
- Blood smear that reveals leukemic blasts, leukoerythroblastic features, or other evidence of leukemia or related hematologic malignancy.
- Family history of unexplained thrombocytosis.

Diagnosis:
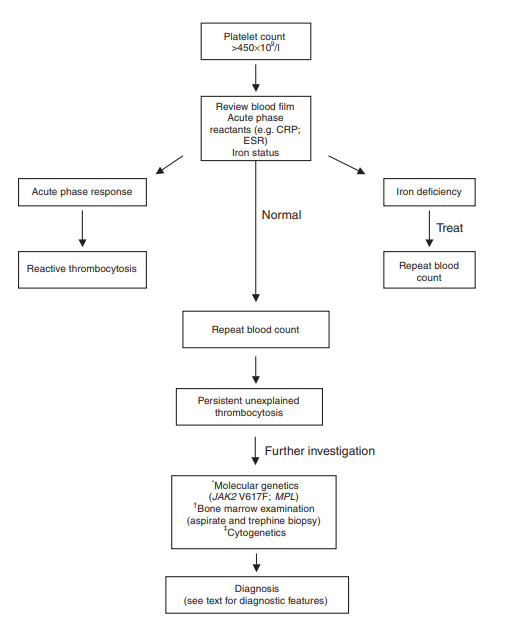
Primary diagnostic goal is to differentiate between primary and secondary thrombocytosis because only primary types have established increased risk of thrombosis and bleeding.
| Cause of thrombocytosis | Lab tests |
|---|---|
| Primary thrombocytosis | If no secondary cause is found, genetic testing for driver mutations such as JAK2, MPL, CALR found in essential thrombocythemia. |
| Secondary thrombocytosis | |
| Bleeding | CBC and reticulocyte count, investigation of underlying bleeding source, for example with upper and lower endoscopy. |
| Hemolysis | CBC, reticulocyte count, LDH, haptoglobin, bilirubin, AST. |
| Iron deficiency | CBC, serum iron, TIBC, ferritin. |
| Asplenia | Peripheral smear for Howell-Jolly bodies. |
| Infections | CXR, CT scan as indicated, blood cultures. |
| Inflammatory disorders | CRP, erythrocyte sedimentation rate, additional evaluation for inflammatory conditions as indicated. |
| Drugs | Stop medication(s) and repeat platelet count. |
| Cancer (highest prevalence in colorectal and mesothelioma) | Cancer screening, imaging as indicated (thrombocytosis may precede diagnosis of cancer by months or years). |

Treatment:
| Primary thrombocytosis | Secondary thrombocytosis | |
|---|---|---|
| Risks | ||
| Thrombosis | Yes | No |
| Bleeding | Yes | No |
| Treatment | ||
| Antiplatelet agent | Yes | No |
| Cytoreductive therapy | Yes | No |
| Plateletpheresis | Yes | Yes* |
| Treat underlying cause | No | Yes |

