Treatment

What would you recommend to the patient’s surgery team?
Returning to a schematic we saw in the Labs section, the results of the 4T score determine the course of action not only with regard to further investigation (immunoassay) but also with regard to management (continue or stop heparin). If heparin is stopped, an alternative non-heparin anticoagulant must be started.

Our patient had a 4T score of 6. As we discussed in the section on labs, blood should be sent for an immunoassay. In addition, heparin should be discontinued, and a suitable anticoagulant started in its place.
What are acceptable alternative anticoagulants to heparin?
In the previous question, DOACs were not offered as an option. Can we use DOACs in a patient with heparin-induced thrombocytopenia (HIT)?
Table of anticoagulants used to treat patients with heparin-induced thrombocytopenia (HIT).
| Drug | Mechanism | Route of administration | Elimination |
|---|---|---|---|
| Argatroban | Small molecule direct thrombin inhibitor | IV, continuous infusion | Liver |
| Bivalirudin | Synthetic analog of hirudin (from leech), a direct thrombin inhibitor | IV, continuous infusion | Enzymatic |
| Fondaparinux | Synthetic pentasaccharide factor Xa (FXa) inhibitor | SC | Kidney |
| Rivaroxaban | Direct FXa inhibitor | PO | Kidney |
Table of anticoagulants used to treat patients with heparin-induced thrombocytopenia (HIT) (cont’d).
| Drug | Dose | Lab monitoring | Comments |
|---|---|---|---|
| Argatroban | Normal organ function → 2 μg/kg/min Liver dysfunction (bilirubin >1.5 mg/dL) Heart failure, multiple organ system failure, severe anasarca, or postcardiac surgery → 0.5-1.2 μg/kg/min | Adjust to aPTT 1.5-3.0 times baseline. | Preferred agent if patient has impaired renal function; contraindicated in patients with severe hepatic failure. |
| Bivalirudin | Normal organ function → 0.15 mg/kg/h Renal or liver dysfunction → dose reduction may be appropriate | Adjust to aPTT 1.5-2.5 times baseline. | Recommended for those undergoing cardiac surgery or percutaneous coronary interventions. |
| Fondaparinux | <50 kg (110 lbs) → 5 mg once per day 50-100 kg (110-221 lbs) → 7.5 mg once per day >100 kg (221 lbs) → 10 mg once per day | None | Cannot be used in patients with renal dysfunction. |
| Rivaroxaban | HITT: 15 mg twice per day × 3 weeks, then 20 mg once per day HIT: 15 mg twice per day until platelet count recovery | None | Included in the 2018 ASH guideline as an acceptable alternative, though not in those with complicated by life- or limb-threatening thromboembolism. |
What would you recommend if the patient was taking warfarin/coumadin at the time of onset of heparin-induced thrombocytopenia (HIT)?
Should I add aspirin to the treatment regimen?
You recommend that the surgery team start argatroban. What is argatroban?
How is argatroban dosed and monitored?
Meanwhile the immunoassay comes back positive, at high titer. What is the next step?
For information on HIT immunoassays, click here.
For information on the serotonin release assay, click here.
What would you do if the immunoassay came back negative?
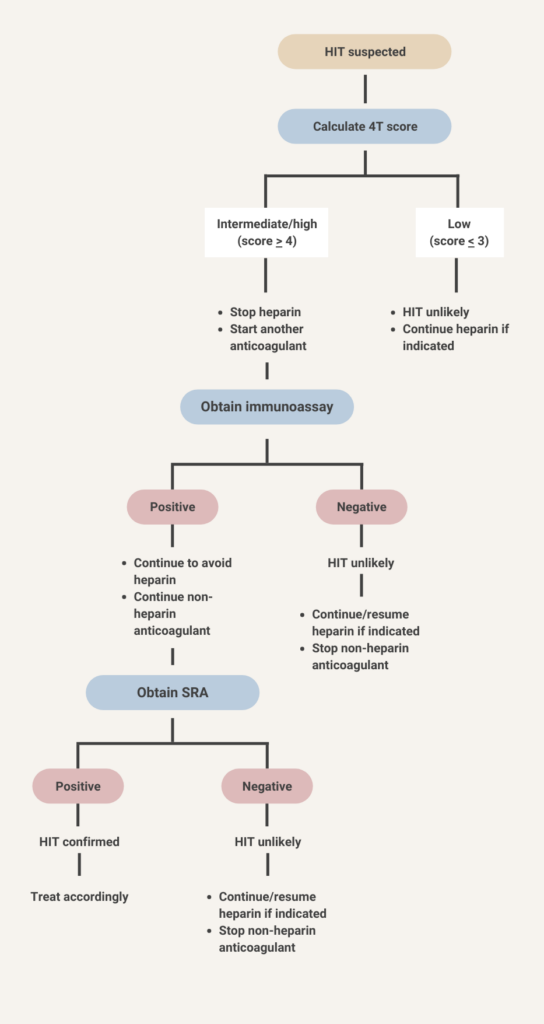
Because the immunoassay in this case was positive, you order a serotonin release assay. It is a send out test and takes several days to come back. While you wait for the result, what action would you take?
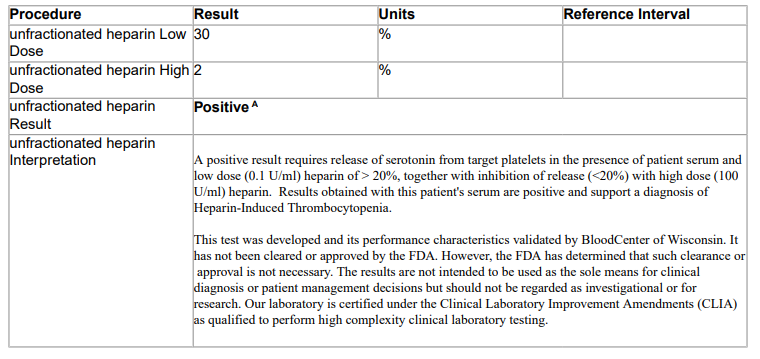
The serotonin release assay comes back positive. This patient’s actual result is shown below:
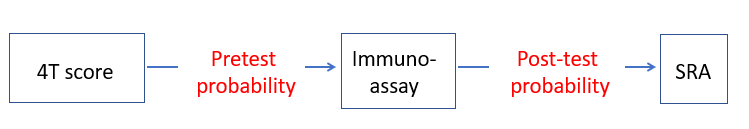
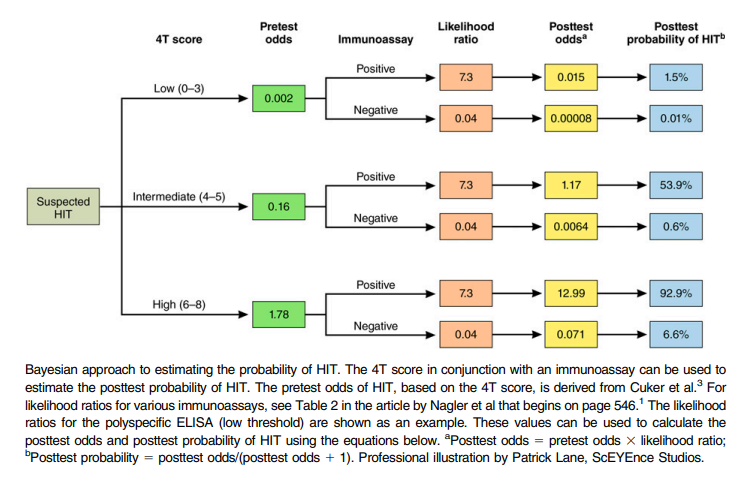
You may run into the terms pretest probability and post-test probability in the heparin-induced thrombocytopenia (HIT) literature.
- The pretest probability is the probability of having HIT based on the initial 4T score. For example, patients with a score of 6 or higher (such as our patient) have a high pretest probability (> 60%) of having HIT.
- The post-test probability is the probability of having HIT (as diagnosed by the gold standard serotonin release assay) based on the results of the immunoassay.
Back to our patient, should you consider transfusing him with platelets?
The surgery team looking after the patient asks whether they should screen for deep vein thrombosis (DVT) in the legs. The patient has no leg swelling, pain or discoloration. What is your recommendation?
How rapdily should plasma exchange be initiated?
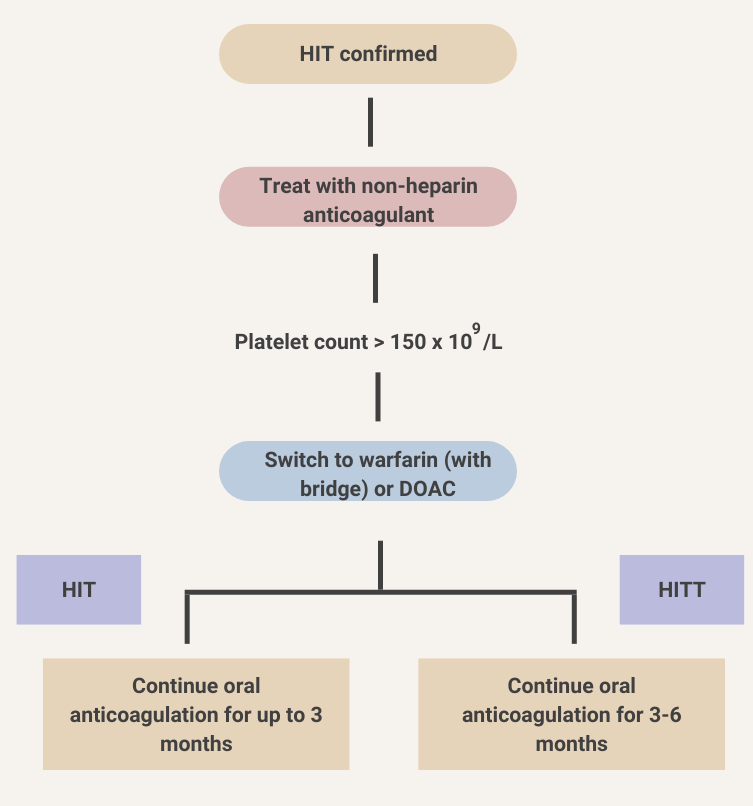
The patient’s platelet counts improve over the next several days while receiving argatroban. He is ready to go home. What are your recommendations for continued anticoagulation?