Treatment

Goals of treatment include:
Iron-rich foods include:
- Red meat
- Poultry
- Fish
- Beans
- Dark green vegetables
- Raisins
- Apricots
- Prunes
- Iron-fortified breads and cereals
True or false: increasing bioavailable iron is often sufficient to replenish iron stores.
What are treatment options for irons supplementation?
Oral iron therapy:
- Provide 60-200 mg elemental iron /day in divided doses without food.
- Consider adding ascorbic acid (250-500 mg twice daily with the iron preparation) to maximize absorption, although there are no data for its effectiveness in the treatment of iron deficiency anemia.
- Continue oral iron for 3-6 months after the iron deficiency has been corrected in order to replenish iron stores.
- Side effects reported in 30%-70% of patients, including:
- Nausea
- Vomiting
- Diarrhea
- Constipation
- Epigastric pain
- Heartburn
- Metallic taste
- Dark stools (does not produce false positive results on tests for occult blood)
- Common preparations include:
- Ferrous sulfate
- 325 mg (65 mg of elemental iron) orally once daily with a meal
- Ferrous gluconate
- 324 mg (38 mg elemental iron) orally 3 to 4 times daily
- Ferrous fumarate –
- 325 mg (106 mg elemental iron) orally once daily between meals
- Ferric citrate
- Ferric maltol
- Carbonyl iron
- Polysaccharide-iron complex
- 1-2 capsules (150-300 mg elemental iron) orally daily
- Heme-iron polypeptide
- Ferrous sulfate
- Slow-release iron preparations should be avoided since iron release occurs beyond the site of maximal absorption (the duodenum).
Intravenous iron therapy:
- Consider use:
- In patients intolerant or not responding to oral iron
- When there is a need for a quick recovery in patients with iron deficiency anemia
- In patients with iron malabsorption
- May be administered:
- Over multiple doses for repletion
- As single dose repletion
- Contraindicated in:
- Patients in the first trimester of pregnancy
- Patients with infections
- Patients with a history of iron or of other drug allergy
- Common IV iron preparations include:
- Low-molecular-weight iron-dextran (for example, Infed)
- Sodium ferric gluconate (Ferrlecit)
- Iron sucrose (Venofer)
- Ferumoxytol (Feraheme)
- Ferric carboxymaltose (Injectafer)
- iron isomaltoside (Monofer)
- Advantages of IV iron include:
- Compliance is assured
- Circumvents the need for gastrointestinal iron absorption
- Fewer gastrointestinal side effects than oral iron
- Results in more rapid increase in Hb levels compared to oral iron
- With some preparations, total dose required (1,000 mg-1,500 mg) can be provided in a single infusion.
- Decreased number of hospital or clinic visits
- Effective in the presence of inflammation
- Disadvantages of IV iron include:
- Infusion reactions
- More expensive than oral iron
This patient received IV iron owing to side effects from oral iron. He was administered two doses of Feraheme 510 mg IV one week apart. The patient felt better within days of the first infusion. The following is the response in complete blood count:
| Day | Hb (g/dL) | MCV (fL) | MCHC (g/dL) | PLT (109/L) |
|---|---|---|---|---|
| 2 months after IV iron | 10.6 | 61 | 26.4 | 357 |
| Day you first saw him | 8.1 | 55 | 24.8 | 516 |
Note the improvement in the hemoglobin, MCV, MCHC and platelet count!
Should the patient have a gastrointestinal work-up for source of bleeding?
Guideline recommendations:
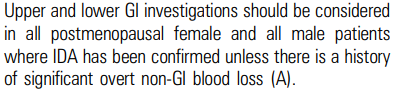
British Society of Gastroenterology (BSG) guideline on management of iron deficiency anemia:
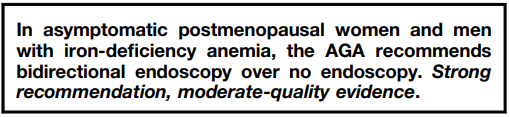
American Gastroenterological Association (AGA) clinical practice guideline on gastrointestinal evaluation of iron deficiency anemia: