Physical Exam
Prev
1 / 5 Next
Prev
1 / 5 Next
Which of the following physical findings are characteristic of iron deficiency anemia?
Physical (1 of 5 slides)
Which of the following physical findings are characteristic of iron deficiency anemia?
Physical (2 of 5 slides)
Which of the following physical findings are characteristic of iron deficiency anemia?
a
Scleral icterus
Scleral icterus may be seen in patients with hemolytic anemia, or in those with anemia associated with chronic liver disease. However, it is not a general finding in iron deficiency anemia.
b
Glossitis
Atrophic glossitis (in which the tongue appears red and smooth) is caused by atrophy of tongue papillae. It is reported in about 30% of patients with iron deficiency. It is a non-specific finding.
c
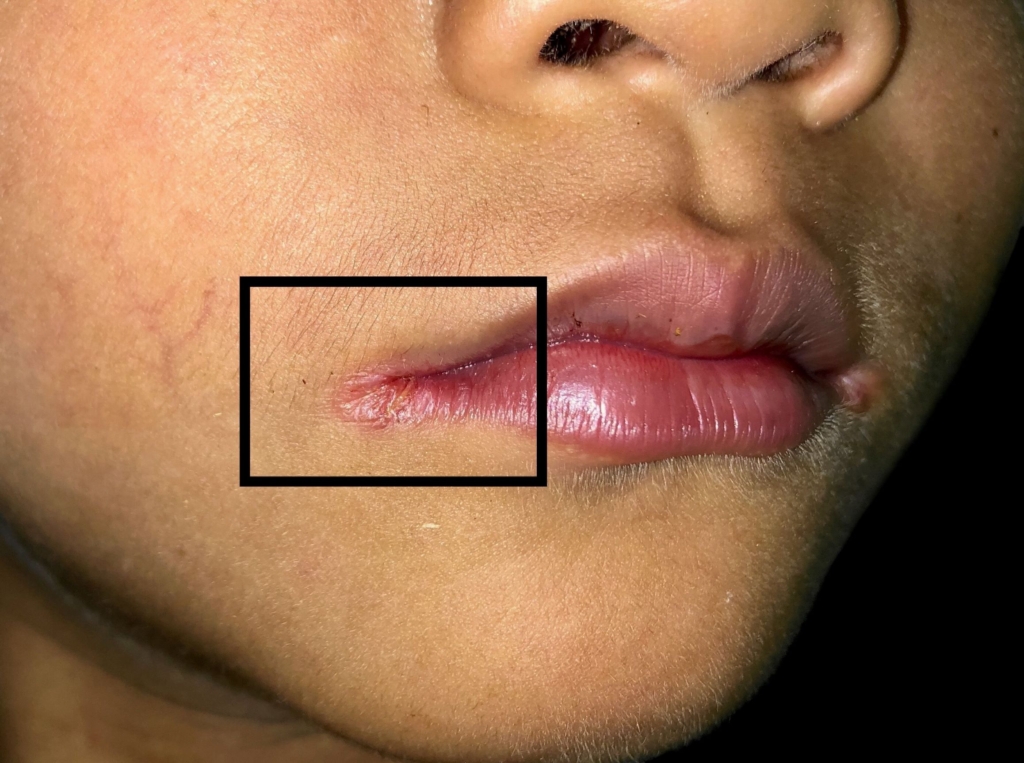
Angular cheilitis (cracking at the corners of the mouth)
Also called angular stomatitis, angular cheilitis is manifested by a grayish white thickening with adjacent erythema at the corners of mouth in early stages, and granulation tissues in later stages.
d
Purpura
Purpura may be a manifestation of a disorder of primary hemostasis (though there are many other causes). It is not a general finding in iron deficiency anemia.
e
Spoon-shaped nails (koilonychia)
Koilonychia is manifested by upward curving of the distal nail plate, resulting in a spoon-shaped nail. It is often associated with nail thinning and brittleness of the nails. Koilonychia is reported in only about 5% of patients with iron deficiency. You will more likely encounter this on a board exam than in a patient!
Physical (3 of 5 slides)
The following describes this patient’s physical exam:
Vital signs: Heart rate is 105/min, other vitals stable
Head and neck: Pale conjunctiva, tongue smooth along the edges
Chest: Normal to inspection, palpation, percussion, and auscultation
Abdomen: Non-tender, no hepatosplenomegaly
CNS: Grossly normal
Skin: Pale; nails cracked
Physical (4 of 5 slides)
Physical (5 of 5 slides)

Prev
1 / 5 Next
