Labs
The following is the complete blood count (CBC) on the day you see the patient:
| WBC (109/L) | Hb (g/dL) | Hct (%) | MCV (fL) | PLT (109/L) |
|---|---|---|---|---|
| 13.5 | 13.2 | 40.5 | 93 | 303 |
What’s what: WBC, white blood cell count; Hb, hemoglobin; MCV, mean cell volume; MCHC, mean cellular hemoglobin concentration; RDW-SD, red cell distribution width-standard deviation; platelets, PLT; Normal values: WBC 5-10 x 109/L, RBC 4-6 x 1012/L, Hb 12-16 g/dL, Hct 35-47%, MCV 80-100 fL, MCHC 32-36 g/dL, RDW-SD < 45 fL, platelets (PLT) 150-450 x 109/L
Thus, the patient does indeed have leukocytosis.
How is a white blood cell differential performed (more than one answer may apply)?
Automated differential

Manual differential

The white cell differential was carried out in this patient using an automated counter. The results are the following:
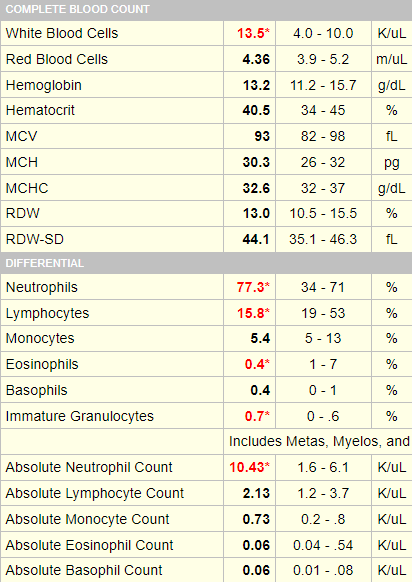

Elevated or decreased white cell subset counts are defined by absolute counts.
To drive this point home, consider the following 3 hypothetical individuals:
| Patient | Total white cell count | % Neutrophils |
|---|---|---|
| 1 | 5 x 109/L | 70 |
| 2 | 0.1 x 109/L | 99 |
| 3 | 100 x 109/L | 2 |
Which patient has neutropenia?
So, we need to rely on absolute counts to define lower- or higher-than-normal values. Before interpreting a patient’s white cell differential. it helps to consult a “cheat sheet” of thresholds:
| White cell subset | Cytosis (increased) | Cytopenia (decreased) |
|---|---|---|
| Total white cells | >11 x 109/L | <4.4 x 109/L |
| Neutrophils | >7.7 x 109/L | <1.5 x 109/L |
| Lymphocytes | >3.5 x 109/L | <1.5 x 109/L |
| Monocytes | >0.8 x 109/L | <0.2 x 109/L |
| Eosinophils | >0.35 x 109/L | <0.04 x 109/L |
| Basophils | >0.1 x 109/L | <0.01 x 109/L |
So, we need to rely on absolute counts to define lower- or higher-than-normal values. Before interpreting a patient’s white cell differential. it helps to consult a “cheat sheet” of thresholds:
| White cell subset | Cytosis (increased) | Cytopenia (decreased) |
|---|---|---|
| Total white cells | >11 x 109/L | <4.4 x 109/L |
| Neutrophils | >7.7 x 109/L | <1.5 x 109/L |
| Lymphocytes | >3.5 x 109/L | <1.5 x 109/L |
| Monocytes | >0.8 x 109/L | <0.2 x 109/L |
| Eosinophils | >0.35 x 109/L | <0.04 x 109/L |
| Basophils | >0.1 x 109/L | <0.01 x 109/L |
The patient’s only absolute count that is out of range is the absolute neutrophil count (10.34 x 109/L).
Therefore, she has neutrophilia.
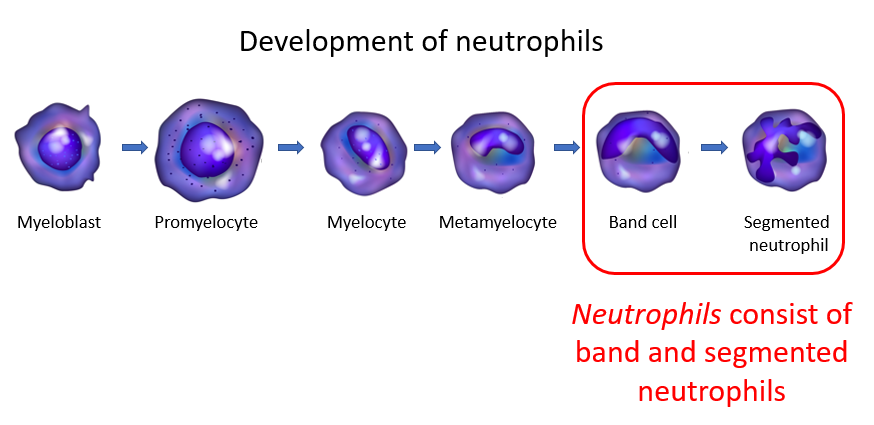
What is included in the neutrophil count (more than one answer may apply)?
A peripheral smear was examined, and was determined to be normal.
We can conclude that the patient has leukocytosis, owing specifically to neutrophilia.
Broadly speaking, neutrophilia can be separated into primary (clonal) and reactive causes. Clonal means that there is autonomous proliferation of neutrophils. Reactive indicates that the cause is coming from a source outside the neutrophil.
An otherwise healthy 47 year-old woman with chronic, incidentally discovered, mild neutrophilia is almost certainly going to have a reactive cause. Let’s consider the possibilities in table format:
| Cause | Patient History |
|---|---|
| Infection | Negative history |
| Inflammation | Negative history of rheumatological disorder, inflammatory bowel disease |
| Smoking | 2 packs per day |
| Metabolic syndrome | Not obese, no diabetes |
| Cushing’s disease | No evidence on history or physical exam |
| Solid tumor | Asymptomatic, up to date on cancer screening |
| Medication | Not taking steroids, lithium or beta agonists |
| Stress | Denies emotional stress or extreme exercise |
| Splenectomy | Negative history |
A C-reactive protein was ordered to screen for inflammation, and this was normal.
Based on these considerations, smoking is the likely cause of the patient’s neutrophilia.
Is it possible to have neutrophilia with a normal white cell count?
Here is an example from a different patient:
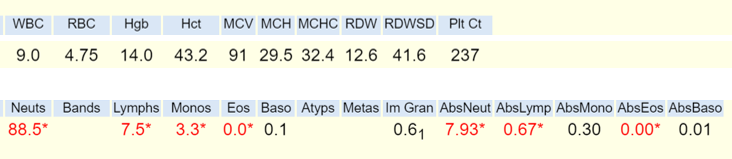
The learning point here is that a normal count can belie abnormalities in the differential, and we won’t know about these unless we look!

