Treatment
True of false: an acute painful sickle cell episode should be treated as a medical emergency?
Supportive care includes which of the following?
Options for pain management include:
Use of corticosteroids for acute pain management suggested against.
Pain management in vaso-occlusive crisis
Currently, opioids constitute the mainstay of treatment for acute pain when patients with sickle cell disease (SCD) seek care in a health care setting.
Other options for pain control in SCD include:
- Acetaminophen
- Anesthetics
- Sodium channel blockers
- Gabapentinoids (Neurontin and Gabapentin)
- Tramadol
- Tapentadol
- Cannabinoids
- Ketamine
- Venom-derived compounds (Ziconotide)
Clinical practice guideline recommendations for treating pain in vaso-occlusive crisis
2014 NHLBI guideline:
Evidence from several randomized control trials and observational studies support the use of opioid therapy in treating vaso-occlusive crises (VOCs).
2020 guideline recommendations from the American Society of Hematology:
- For adults and children with sickle cell disease (SCD) presenting to an acute care setting with acute pain related to SCD, the ASH guideline panel recommends rapid (within 1 hour of emergency department [ED] arrival) assessment and administration of analgesia with frequent reassessments (every 30-60 minutes) to optimize pain control (strong recommendation based on low certainty in the evidence about effects).
- For adults and children with SCD presenting to an acute care setting with acute pain related to SCD for whom opioid therapy is indicated, the ASH guideline panel suggests tailored opioid dosing based on consideration of baseline opioid therapy and prior effective therapy (for adults: conditional recommendation based on moderate certainty in the evidence about effects).
- For adults and children with acute pain related to SCD, the ASH guideline panel suggests a short course (5 to 7 days) of nonsteroidal anti-inflammatory drugs (NSAIDs) in addition to opioids for acute pain management (conditional recommendation based on very low certainty in the evidence about effects).
- For adults and children presenting for acute pain related to SCD, the ASH guideline panel suggests against corticosteroids for acute pain management (conditional recommendation based on low certainty in the evidence about effects).
- For adults and children presenting with acute pain related to SCD who are hospitalized, the ASH guideline panel suggests a subanesthetic (analgesic) ketamine infusion as adjunctive treatment of pain that is refractory or not effectively treated with opioids alone (conditional recommendation based on very low certainty in the evidence about effects.
- For adults and children presenting with acute pain related to SCD, the ASH guideline panel suggests regional anesthesia treatment approaches for localized pain that is refractory or not effectively treated with opioids alone (conditional recommendation based on very low certainty in the evidence about effects.
- For adults and children who seek treatment of acute pain, the ASH guideline panel suggests massage, yoga, transcutaneous electrical nerve stimulation (TENS), virtual reality (VR), and guided audiovisual (AV) relaxation in addition to standard pharmacological management (conditional recommendation based on very low certainty in the evidence about effects.
A reminder of the patient’s complete blood counts:
| Date | WBC (109/L) | Hb (g/dL) | MCV (fL) | PLT (109/L) |
|---|---|---|---|---|
| Day of admission | 11.2 | 6.3 | 105 | 403 |
| 2 months earlier | 7.3 | 7.9 | 106 | 313 |
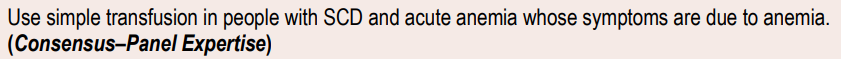
Assuming that the patient is asymptomatic from her anemia, should she be transfused?
The drop in Hb is typical for a patient with vaso-occlusive crisis. See explanation for not transfusing her on the next slide.
Clinical practice guideline recommendations for transfusion in vaso-occlusive crisis
NHLBI recommendations:
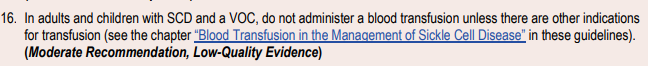
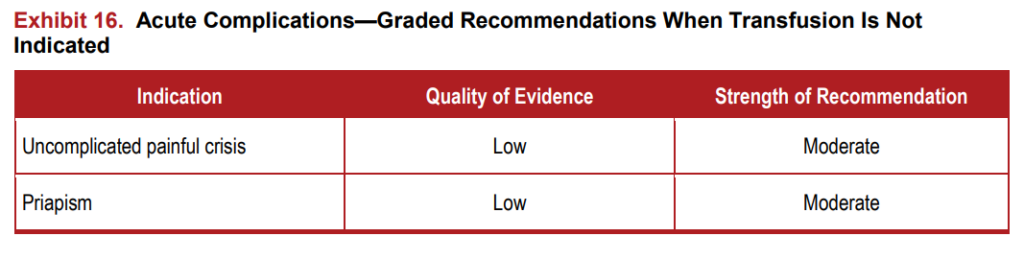
baseline value
British Society of Hematology recommendations:
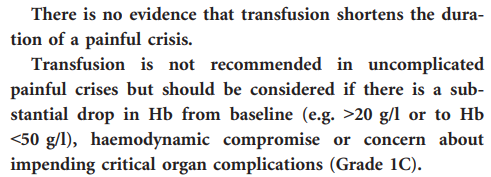
Bottom line:
Bottom line: do not routinely transfuse your patient with vaso-occlusive crisis… only if there is another indication to do so!
The patient has an oxygen saturation of 96% on room air. Should she be provided with supplemental oxygen?
You ignore the recommendation not to administer supplemental oxygen, and provide the patient with 2 liters oxygen by nasal prongs. You end up obtaining an arterial blood gas on her and show that the PO2 is 168 mmHg. That’s a big jump from a normal arterial PO2 of 90-100 mmHg. Does it represent a significant improvement in her blood oxygen content and oxygen delivery?
Oxygen delivery = cardiac output x oxygen content of blood
Oxygen content of blood = (Hb x SaO2 x oxygen binding capacity of Hb) + amount of dissolved oxygen in blood
- Oxygen binding capacity of Hb = 1.39 ml oxygen/gram Hb
- Dissolved oxygen in blood 0.003 ml oxygen x PaO2
Oxygen delivery = cardiac output x ([Hb x SaO2 x 1.39] + [0.003 x PaO2])
On room air:
Oxygen delivery = cardiac output x ([Hb x 96 x 1.39] + [0.003 x 100])
On 2L nasal prongs:
Oxygen delivery = cardiac output x ([Hb x 100 x 1.39] + [0.003 x 168])
As you can see from the above calculations, the change in oxygen content and oxygen delivery is minimal when the patient is provided with supplemental oxygen!
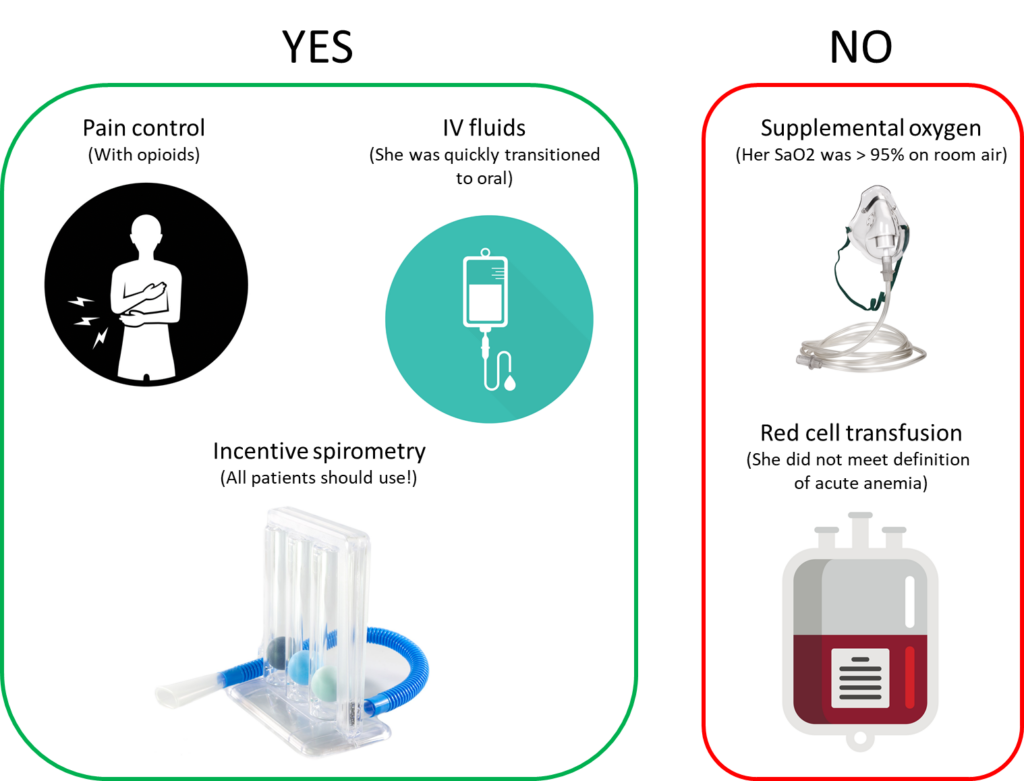
Course in hospital
The patient was treated with opioids. Her oxygen saturations were consistently > 95%, so she did not require supplemental oxygen. She was instructed to use incentive spirometry every 4 hours while awake. She was initially started on IV fluids (normal saline) because she was in too much pain to take liquids orally, but she was transitioned to oral fluids shortly thereafter. She was not transfused with red cells. Her pain subsided over the next 5 days, and her hemoglobin increased to her baseline of about 8 g/dL. She was discharged from the hospital feeling fatigued, but otherwise well.
Schematic of what the patient received and did not receive: