Labs
The following results are from the complete blood count (CBC) the day you see the patient:
| WBC (109/L) | Hb (g/dL) | MCV (fL) | PLT (109/L) |
|---|---|---|---|
| 11.2 | 6.3 | 105 | 403 |
What’s what: WBC, white blood cell count; Hb, hemoglobin; MCV, mean cell volume; MCHC, mean cellular hemoglobin concentration; RDW-SD, red cell distribution width-standard deviation; platelets, PLT; Normal values: WBC 5-10 x 109/L, RBC 4-6 x 1012/L, Hb 12-16 g/dL, Hct 35-47%, MCV 80-100 fL, MCHC 32-36 g/dL, RDW-SD < 45 fL, platelets (PLT) 150-450 x 109/L
Indeed, the reticulocyte count was elevated:
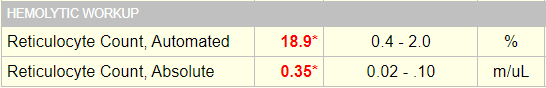
Reticulocyte count is:
- 18.9% of the total red cell count
- 0.35 x 1012/L or 350 x 109/L
Focus on the absolute reticulocyte count. It keeps things simple. An absolute reticulocyte count >120 x 109/L is considered an appropriate response to anemia.
Therefore, this patient has a hyperproliferative anemia.
What is a typical baseline Hb for a patient with sickle cell anemia (HbSS)?
Here are data on baseline hemoglobin concentration (Hb) from a large series of patients with HbSS:
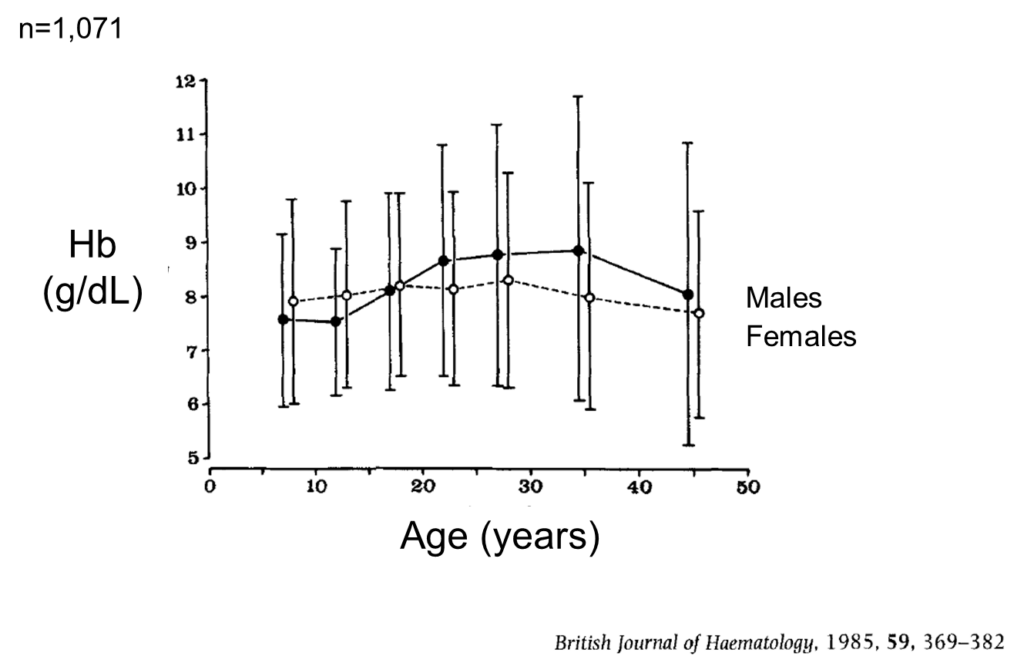
Your patient presented with a hemoglobin concentration (Hb) of 6.3 g/dL. What do you predict her baseline Hb is?
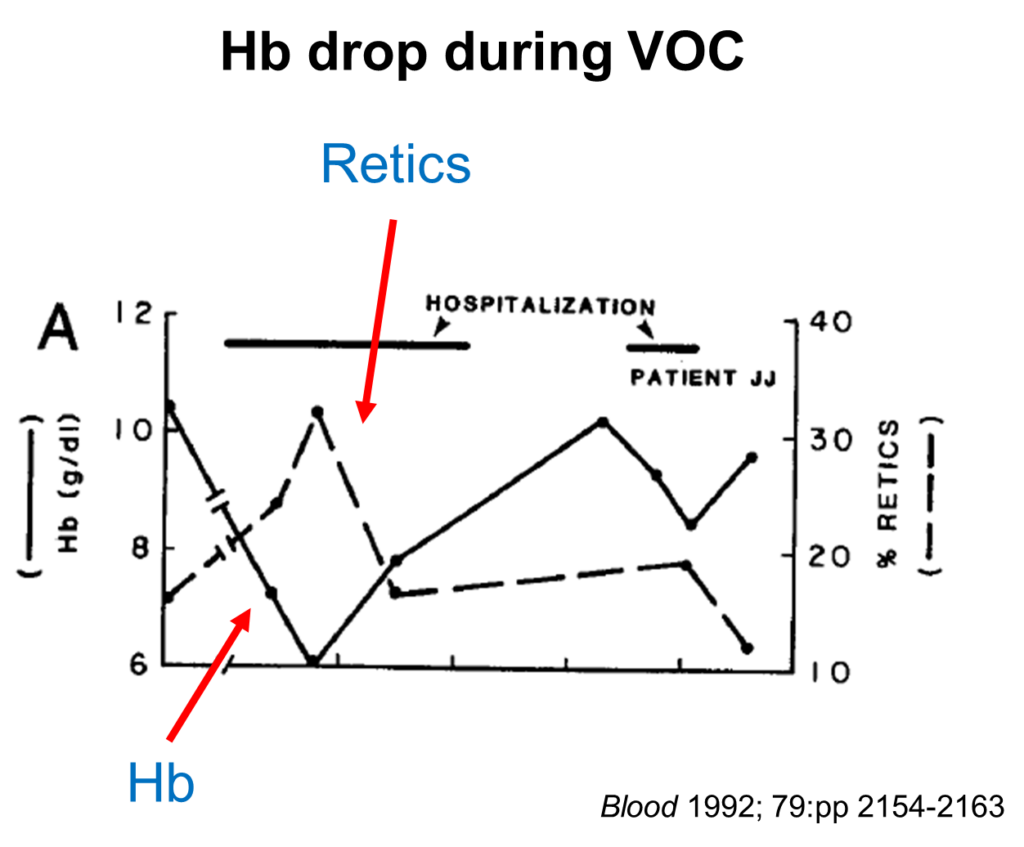
Most patients with a veno-occlusive crisis (VOC) experience a drop in hemoglobin (Hb) of 1-2 g/dL. Here is a nice example from a single patient during the course of their pain crisis (note how the drop in Hb is accompanied by an increase in % reticulocytes [% retics]):
Let’s look at the baseline values for this patient’s complete blood count:
| Date | WBC (109/L) | Hb (g/dL) | MCV (fL) | PLT (109/L) |
|---|---|---|---|---|
| Day of admission | 11.2 | 6.3 | 105 | 403 |
| 2 months earlier (baseline) | 7.3 | 7.9 | 106 | 313 |
What’s what: WBC, white blood cell count; Hb, hemoglobin; MCV, mean cell volume; MCHC, mean cellular hemoglobin concentration; RDW-SD, red cell distribution width-standard deviation; platelets, PLT; Normal values: WBC 5-10 x 109/L, RBC 4-6 x 1012/L, Hb 12-16 g/dL, Hct 35-47%, MCV 80-100 fL, MCHC 32-36 g/dL, RDW-SD < 45 fL, platelets (PLT) 150-450 x 109/L
Note the new leukocytosis and the drop in hemoglobin concentration (Hb).
The patient has a new (albeit mild) leukocytosis. This is not unusual in a case of vaso-occlusive crisis. Here is her white blood cell differential:
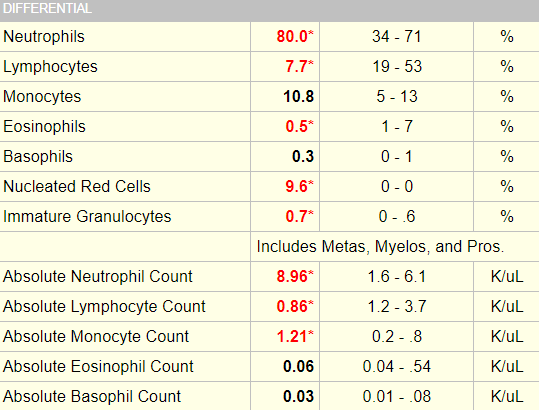

These data indicate neutrophilia, lymphopenia and monocytosis (remember, focus on the absolute counts). How can we make these determinations? By referring to our cheat sheet!
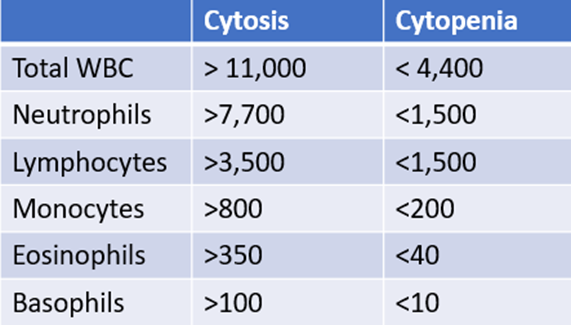
The patient’s white cell differential is consistent with stress.
Which of the following lab values would you expect to be elevated?
The results of her hemolysis labs are shown in the following table:
| Date | AST (IU/L) | LDH (IU/L) | Bilirubin (mg/dL) | Haptoglobin (mg/dL) |
|---|---|---|---|---|
| Day of admission | 32 | 408 | 2.9 | Undetectable |
| 2 months earlier | 23 | 384 | 0.5 | 86 |
Normal values: AST 040 IU/L, LDH 115-275 IU/L, bilirubin 0.0-1.5 mg/dL, Haptoglobin 30-200 mg/dL.
Other labs and imaging:
- Creatinine and electrolytes were normal.
- Chest X-ray in the emergency room was normal.
In summary, the labs reveal acute hemolysis on a background of low-grade hemolysis (based on the elevated LDH at baseline).
Are there any specific tests for vaso-occlusive (pain) crisis in sickle cell disease?
Does this patient have vaso-occlusive crisis?

