Treatment

How would you treat this patient?
How would you treat this patient?
IVIG raises the platelet count within 1 to 4 days in 80% of patients, but effects last only 1 to 2 weeks. IVIG is indicated in patients with active serious bleeding and in those with very low platelet counts (<10 x 109/L), who are at increased risk for serious bleeding.
Glucocorticoid treatment is the standard initial therapy for patients with ITP
What are the recommended steroid regimens for newly diagnosed ITP?
What are the recommended steroid regimens for newly diagnosed ITP?
Is there anything to choose between prednisone 1 mg/kg and the 4-day dexamethasone regimen?
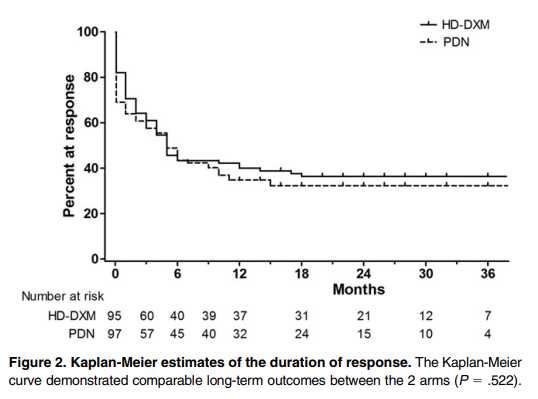
According to the 2019 ASH guideline, you might consider dexamethasone over prednisone if rapid initial platelet response is important. This recommendation is based on the results of a randomized trial comparing prednisone and dexamethasone showing shorter time to response in the dexamethasone arm. In a metanalysis of randomized trials comparing these two steroid regimens, platelet counts were higher at 14 days in patients receiving dexamethasone, but overall responses at 6 months did not differ significantly. Prednisone is associated with higher rates of weight gain and cushingoid appearance, whereas dexamethasone may be associated with higher rates of neuropsychiatric symptoms.
The following is a comparison between prednisone 1 mg/kg and the 4-day dexamethasone in treating newly diagnosed adult ITP:
| Parameter | Prednisone | Dexamethasone |
|---|---|---|
| Initial response rate | 60%-80% | 60-80% |
| Time to initial response | 4-14 days | 2-14 days |
| Time to peak response | 7-28 days | 4-28 days |
| Sustained response | 30%-50% | 30%-50% |
Which of the following is an appropriate option for treating the patient (we will address treatment of iron deficiency anemia in more detail in another case study)?
How do corticosteroids work in ITP?
In addition to corticosteroids, intravenous immune globulin (IVIG) is considered a first-line therapy. However, the response, while quick, is typically transient and does not lead to sustained responses. IVIG is typically reserved for patients:
- Who are bleeding or at high risk of bleeding (as an adjunctive treatment).
- Who are unresponsive to prednisone.
- Who have contraindications to high-dose corticosteroids.
Let’s look at a comparison in responses with the various first line therapies in immune thrombocytopenia (ITP):
| Initial response rate | Time to initial response | Time to peak response | |
|---|---|---|---|
| Prednisone | 60-80% | 4-14 days | 7-28 days |
| Dexamethasone | 60-80% | 2-14 days | 4-28 days |
| IVIG | 80% | 1-4 days | 2-7 days |
What if my patient was actively bleeding, for example he was having a major GI bleed?
What if my patient was having a major gastrointestinal (GI) bleed?
To summarize, treatment for a major bleed includes a combination of corticosteroids, immune globulin (IVIG) and platelet transfusions. For more information click here.
What is the treatment goal?
Fortunately, our patient did not have a major bleed.
He was administered dexamethasone 40 mg daily for 4 days. His platelet count was 36 x 109/L on day 4, at which time he was discharged home (most responsive patients will demonstrate improved platelet counts 2-4 days after initiation of corticosteroids, but response may take 5 to 7 days or longer in some patients).
What is the goal of treatment?
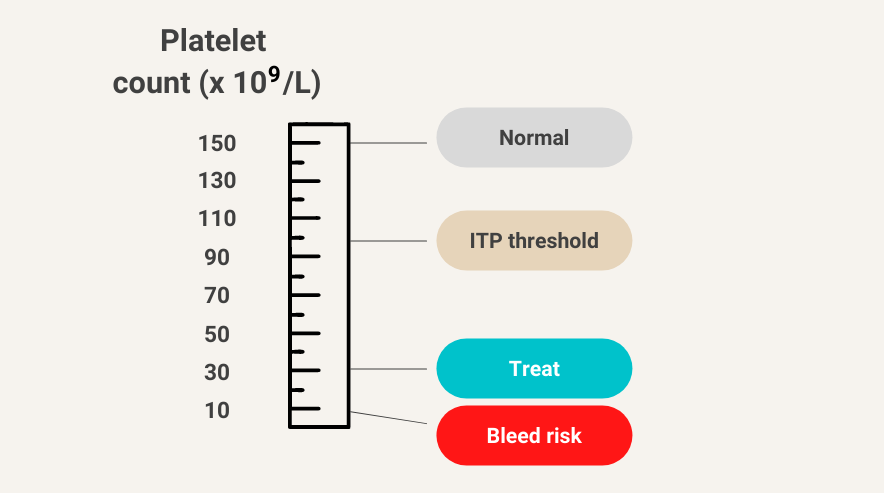
Maintain target platelet count > 20-30 × 109/L to reduce risk of major bleeding.
Spontaneous bleeding is uncommon at platelet counts >30 × 109/L
What is the treatment goal?
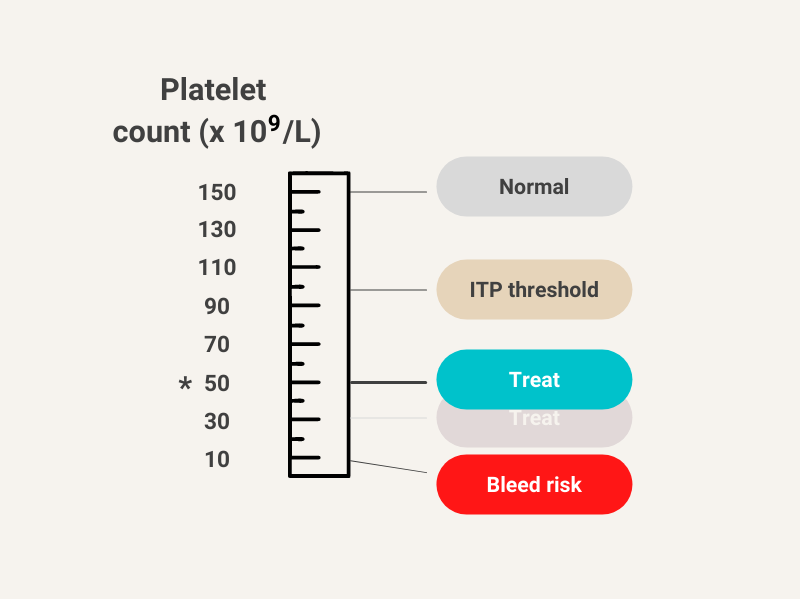
What if the patient was taking an anticoagulant for a recent deep venous thrombosis or atrial fibrillation? Do the treatment goals change?
Yes, patient should ideally receive treatment to maintain platelet counts above 50 x 109/L.
What is the likelihood he will relapse within the next 6 months?
What is the likelihood this patient will relapse in the next 6 months?
