Labs
Here is the patient’s complete blood count (CBC) when you see him in clinic:
| WBC | Hb | Hct | MCV | MCHC | RDW-SD | PLT |
|---|---|---|---|---|---|---|
| 5.2 | 11.2 | 40 | 78 | 28 | 42 | 5 |
What’s what: WBC, white blood cell count; Hb, hemoglobin; MCV, mean cell volume; MCHC, mean cellular hemoglobin concentration; RDW-SD, red cell distribution width-standard deviation; platelets, PLT; Normal values: WBC 5-10 x 109/L, RBC 4-6 x 1012/L, Hb 12-16 g/dL, Hct 35-47%, MCV 80-100 fL, MCHC 32-36 g/dL, RDW-SD < 45%, platelets (PLT) 150-450 x 109/L
Thrombocytopenia is commonly graded according to the platelet count:
- Mild = 70-150 × 109/L
- Moderate = 20-70 × 109/L
- Severe = < 20 × 109/L
Thus, by definition, it is fair to say that the patient has microcytic, hypochromic anemia and severe thrombocytopenia.
We established in the section on Differential Diagnosis that the three likeliest possibilities in this outpatient with severe thrombocytopenia and an unremarkable history include:
- Immune thrombocytopenia
- Pseudothrombocytopenia
- Familial (congenital) thrombocytopenia
What would you expect to find for each condition on the peripheral smear? The answers are on the next slide.
| Condition | Findings |
|---|---|
| Pseudothrombocytopenia | |
| Familial thrombocytopenia (FT) | |
| ITP |
What would you expect to find for each condition on the peripheral smear? The answers are on the next slide.
| Condition | Findings |
|---|---|
| Pseudothrombocytopenia | Platelet clumping |
| Familial thrombocytopenia (FT) | Giant platelets (in some types of FT) |
| ITP | +/- Large platelets, but less than in FT |
The peripheral smear from our patient is shown here:
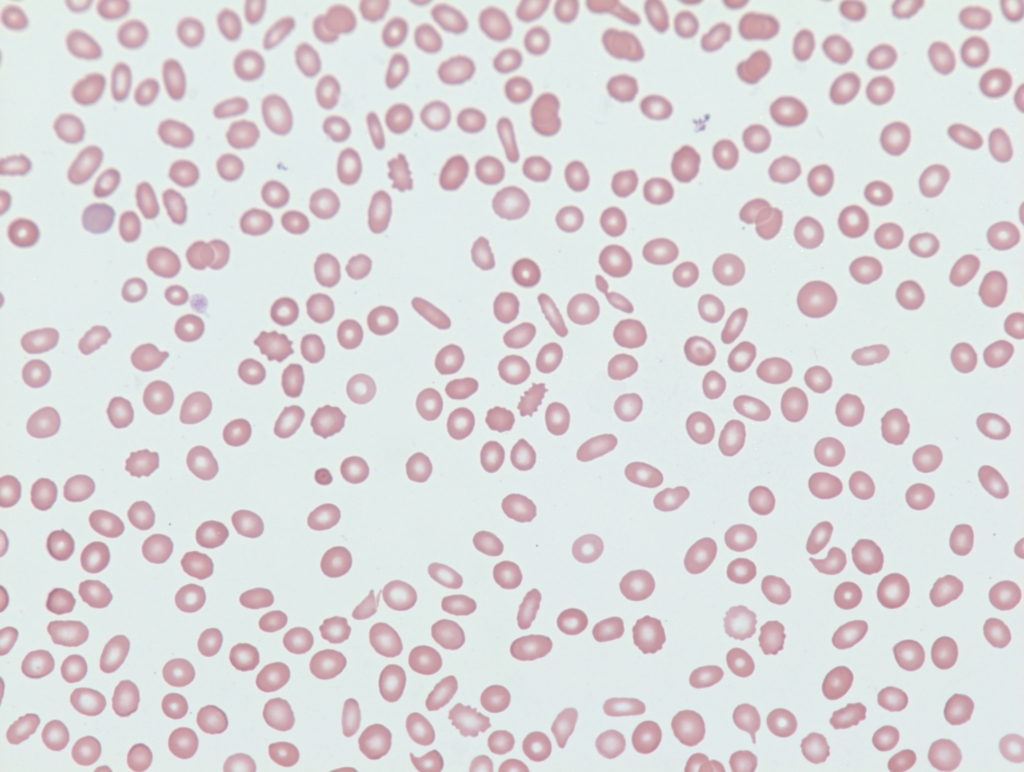
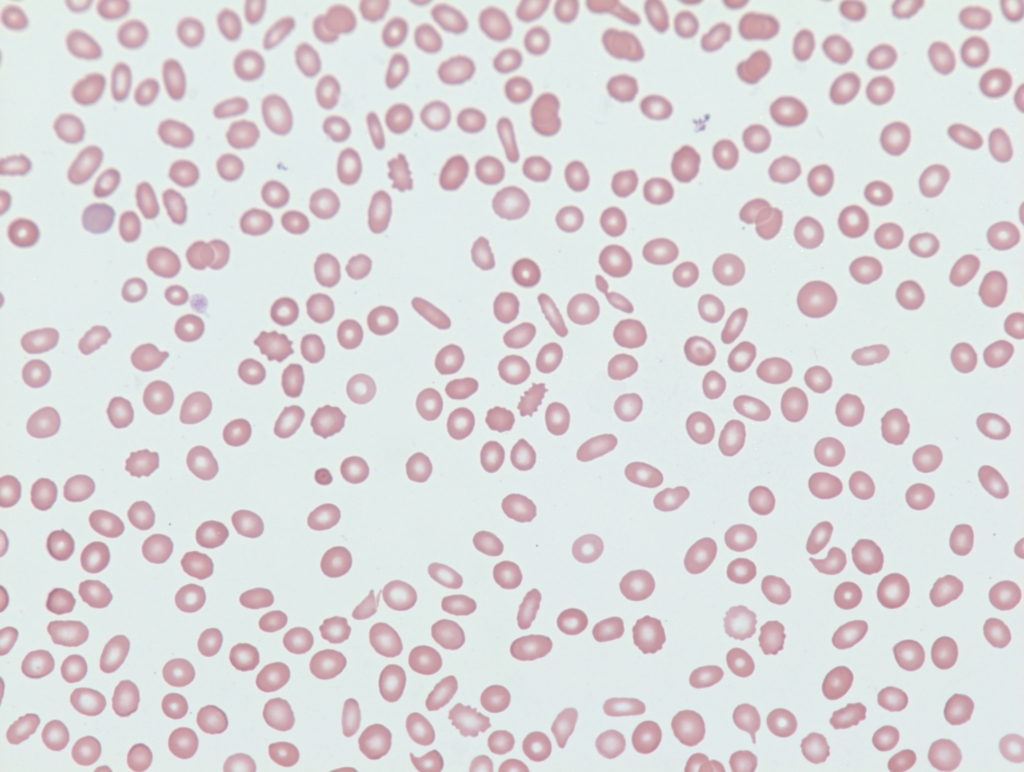
What is the mild microcytotic, hypochromic anemia, together with the presence of elliptocytes on the peripheral smear most suggestive of?
What is the mild microcytotic, hypochromic anemia, together with the presence of elliptocytes on the peripheral smear, most suggestive of?
What is the most likely diagnosis?
What other labs would you like to order?
There are two goals in working up a patient with suspected ITP:
- Rule out other causes of thrombocytopenia
- Test for causes of secondary ITP (underlying conditions that are associated with/cause ITP)
For details about ITP classification, click here.
Different guideline organizations and evidence-based resources recommend overlapping but distinct panels of tests for patients with suspected ITP. For details, click here. They can be broadly summarized as follows:
All patients should be tested with/for:
- Complete blood count
- Peripheral blood smear
- HIV serology (a cause of secondary ITP whose treatment may normal platelet count)
- HCV serology (a cause of secondary ITP whose treatment may normal platelet count)
Selected patients may be tested with/for:
- H. pylori (a cause of secondary ITP whose treatment may normal platelet count)
- Serum immunoglobulins (to rule out combined variable immunodeficiency)
- Bone marrow biopsy
- PT and aPTT
What do you do next?
You have assessed the CBC and peripheral smear. You may have ordered liver function tests to evaluate for possible chronic liver disease as the cause of the patient’s thrombocytopenia. And perhaps you ordered a serum ferritin to confirm iron deficiency. Results for HIV and HCV serology will not be available until the next day.
What do you do next?
Correct. Clinical practice guidelines recommend: 1) treating a patient with ITP if platelet count < 20-30 x 109/L, and 2) admitting such patients to the hospital for initial management.
The patient is admitted directly to the hospital



