Labs and Course in Hospital
The following is the complete blood count (CBC) at the time of admission:
| WBC (109/L) | Hb (g/dL) | Hct (%) | MCV (fL) | RDW-SD (fL) | PLT (109/L) |
|---|---|---|---|---|---|
| 1.6 | 10.0 | 29 | 86 | 35.8 | 77 |
What’s what: WBC, white blood cell count; Hb, hemoglobin; MCV, mean cell volume; MCHC, mean cellular hemoglobin concentration; RDW-SD, red cell distribution width-standard deviation; platelets, PLT; Normal values: WBC 5-10 x 109/L, RBC 4-6 x 1012/L, Hb 12-16 g/dL, Hct 35-47%, MCV 80-100 fL, MCHC 32-36 g/dL, RDW-SD < 45 fL, platelets (PLT) 150-450 x 109/L
White blood cell differential:
| Cell type | Patient’s result |
|---|---|
| Neutrophil | 1.39 x 109/L |
| Lymphocyte | 0.14 x 109/L |
| Monocyte | 0.06 x 109/L |
| Eosinophil | 0.00 x 109/L |
| Basophil | 0.00 x 109/L |
In case you are not sure how to characterize white blood cell (WBC) subtype counts, here is a helpful cheat sheet!
Notice how elevated (cytosis) or reduced (cytopenia) counts of the 5 subtypes of white blood cells are defined by ABSOLUTE COUNTS, not percentages!!
For those who have the habit of examining the percentages, consider the following examples:
| Label | Total WBC (x 109/L) | Neutrophil % | ANC (x 109/L) | Lymphocyte % | Lymphocyte count (x 109/L |
|---|---|---|---|---|---|
| Normal | 10.0 | 60 | 6.0 | 20 | 2.0 |
| Patient 1 | 0.1 | 100 | 0.1 | 0 | 0 |
| Patient 2 | 200 | 2 | 4.0 | 80 | 160 |
Which the above case(s) is/are associated with neutropenia?
So, at this point we have a 44 year-old man with constitutional symptoms and pancytopenia.
The peripheral smear was unremarkable.
Other routine admission testing revealed:
- Normal renal function
- Normal electrolytes
- Normal Alk
- Normal bilirubin
- Normal PT
- Normal aPTT
- AST 163 IU/L (normal 0-40 IU/L)
- ALT 122 IU/L (normal 0-40 IU/L))
Now what? Let’s organize the differential diagnosis of pancytopenia in table format and consider likely diagnoses and next steps in lab testing:
| Comment | Lab tests to consider | |
|---|---|---|
| Underproduction | ||
| Drugs | No history | N/A |
| Toxins | No history | N/A |
| Infections | Cannot rule out | Viral serologies |
| Alcohol | No history | N/A |
| Radiation | No history | N/A |
| Anorexia | No history | N/A |
| PNH | No symptoms but cannot rule out | PNH screen |
| BM infiltration | ||
| Malignancy | Cannot rule out | Torso imaging, BM biopsy |
| Myelofibrosis | Peripheral smear not typical | N/A |
| Granuloma | Cannot rule out | BM biopsy |
| Nutritional | Cannot rule out | Vitamin B12/folate levels |
| Peripheral destruction | No history of autoimmune disease | ANA, hemolysis markers |
| Sequestration | No history of CLD but cannot rule out | Abdominal imaging |
Abbreviations: N/A, not applicable; BM, bone marrow; PNH, paroxysmal nocturnal hemoglobinuria; CLD, chronic liver disease
The following tests were performed:
| Test | Patient results (normal range) |
|---|---|
| Hemolysis (PNH, autoimmune pancytopenia) | |
| Haptoglobin | <10 (30-300 mg/dL) |
| LDH | 952 (40-130 IU/L |
| AST | 163 (0-40 IU/L) |
| ALT | 122 (0-40 IU/L) |
| Bilirubin | 0.6 (0-1.5 mg/dL) |
| Viral serologies | |
| EBV | IgG positive; IgM negative; viral load not detected |
| CMV | IgG positive; IgM negative; viral load not detected |
| Nutritional status | |
| Vitamin B12/folate | Normal |
| Torso imaging | Not done immediately |
Abbreviations: LDH, lactate dehydrogenase
The haptoglobin is decreased and the LDH increased, and there is no convincing data of chronic liver disease. These data raise the possibility of hemolysis. What do you expect the reticulocyte count to be?
The reticulocyte count was only 0.1 x 109/L. This is an inappropriate response to anemia.
Other testing revealed an elevated serum ferritin 7706 ng/mL.
What are general mechanisms of an elevated ferritin (more than one answer may apply)?
The results of this patient’s acute phase response:
| Marker | Patient results (normal range) |
|---|---|
| Positive acute phase protein | |
| CRP | 40.7 (0-5 mg/L) |
| Fibrinogen | 230 (180-400 mg/dL) |
| Haptoglobin | <10 (30-200 mg/dL) |
| Negative acute phase protein | |
| Transferrin (TIBC) | 128 (200-360 mg/dL) |
| Albumin | 3.3 g/dL (3.5-5.2 g/dL) |
The elevated ferritin and CRP, and the low TIBC and albumin support the presence of inflammation. While haptoglobin is a positive acute phase reactant, it is highly sensitive to hemolysis and levels will be low when there is concomitant inflammation and hemolysis. The fibrinogen is inappropriately low relative to other acute phase proteins.
Note that an ESR was not obtained.
Based on the information so far, is there another diagnosis we should consider that was not included in our original differential diagnosis of pancytopenia?
But is hemophagocytic lymphohistiocytosis (HLH) associated with low haptoglobin and high LDH?
True of false: the patient’s ferritin of 7706 ng/ml is diagnostic of hemophagocytic lymphohistiocytosis (HLH).
Which of the following findings is diagnostic for hemophagocytic lymphohistiocytosis (HLH)?
At this point, the diagnosis of hemophagocytic lymphohistiocytosis (HLH) is on the table. Are you familiar with any diagnostic scoring system for HLH?
Let’s look at each scoring system in turn:
HLH-2004
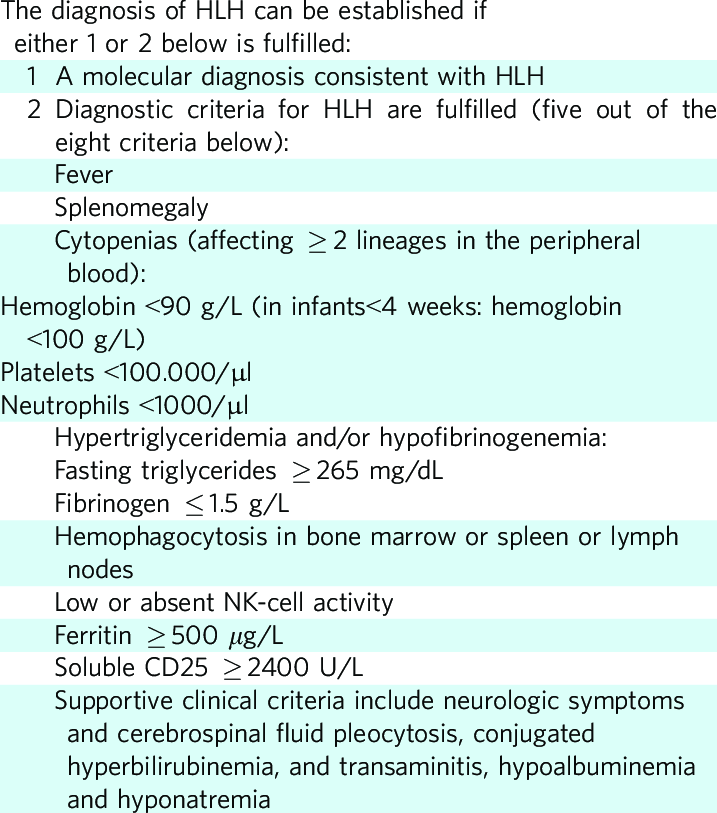
This patient met the following criteria:
- Fever
- Splenomegaly
- Cytopenias
- Increased triglycerides (results were 320 mg/dL)
- Increased ferritin
Note: sIL2R and pathology take several days to come back. But in this case, we have 5/8 criteria, suggestive of HLH.
HScore
The calculator for the HScore can be found here.
This patient’s score was 254 suggesting > 99% probability of HLH.
Scoring breakdown:
- Temperature > 102.9 (+49)
- Splenomegaly alone (+23)
- 3 lineagecytopenia (+34)
- Ferritin > 6,000 ng/mL (+50)
- Triglycerides 132.7-354 mg/dL (+44)
- Fibrinogen > 250 mg/dL (+0)
- AST > 30 U/L (+19)
- Hemophagocytosis features on bone marrow aspirate (+35)
We are admittedly concerned about the possibility of hemophagocytic lymphohistiocytosis (HLH). What additional studies would you want to pursue next given this concern?
Given leukopenia, cough, and fevers, the patient is started on broad-spectrum antibiotics. A CT torso is obtained to further evaluate possible pulmonary infection as well as axillary lymphadenopathy.
CT abdomen/pelvis showed:
- No evidence of malignancy
- Moderate splenomegaly (15.7 cm)
CT chest showed bilateral axillary lymphadenopathy.
Given concern for an underlying malignancy as the driver of his pathologic condition, the patient undergoes an excisional biopsy of an enlarged right axillary lymph node. He subsequently undergoes PET-CT to evaluate for other areas of FDG uptake.

Why is fine needle aspiration (FNA) inadequate for the diagnosis of suspected lymphoma?
Click for AnswerFDG PET:CT – no abnormal FDG uptake identified
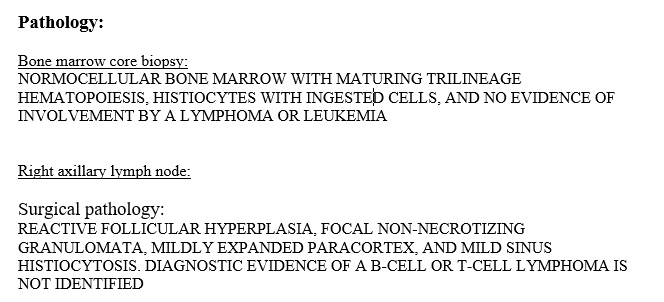
The bone marrow biopsy results showed hemophagocytosis.
The patient now meets 6/8 criteria:
- Fever
- Splenomegaly
- Cytopenias
- Increased triglycerides (320)
- Increased ferritin
- Hemophagocytosis
Recall that the remaining criteria include:
- sIL2R (this would ultimately come back markedly elevated [3131 pg/mL])
- Low NK cell function (rarely performed)
The soluble IL-2 receptor was 3131 pg/mL (normal range 175.3-858.2 pg/ml).
