A single lab value
Before laying eyes on the patient, consider the following:
The patient’s hemoglobin is 8.4 g/dL
Where do you go from here? Of the following labs, which are you most interested in?
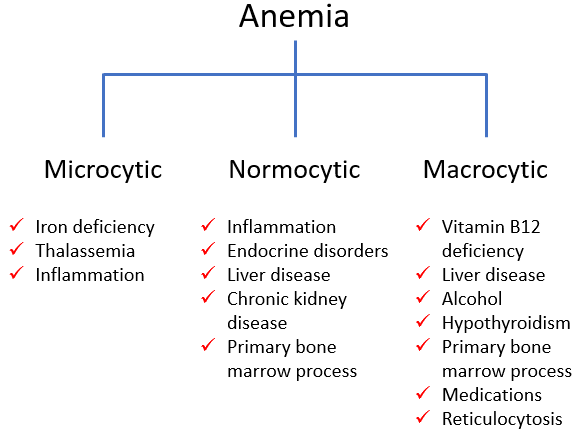
Morphological classification of anemia:
Here is the patient’s mean cell volume (MCV):
| Parameter | Patient value (fL) | Normal range (fL) |
|---|---|---|
| MCV | 117 | 80-100 |
This test result is indicative of:
You have been told that the patient has a congenital form of anemia, and indeed you would be suspicious of a hereditary condition given his young age. What is the one likeliest cause of the elevated mean cell volume?
Reticulocytosis appears on the morphological classification under macrocytosis, but sometimes an increased reticulocyte count does not elevate the mean cell volume above 100 fL. A better way of considering the reticulocyte count is to incorporate it as the first branch point in the morphological classification. It looks something like this:
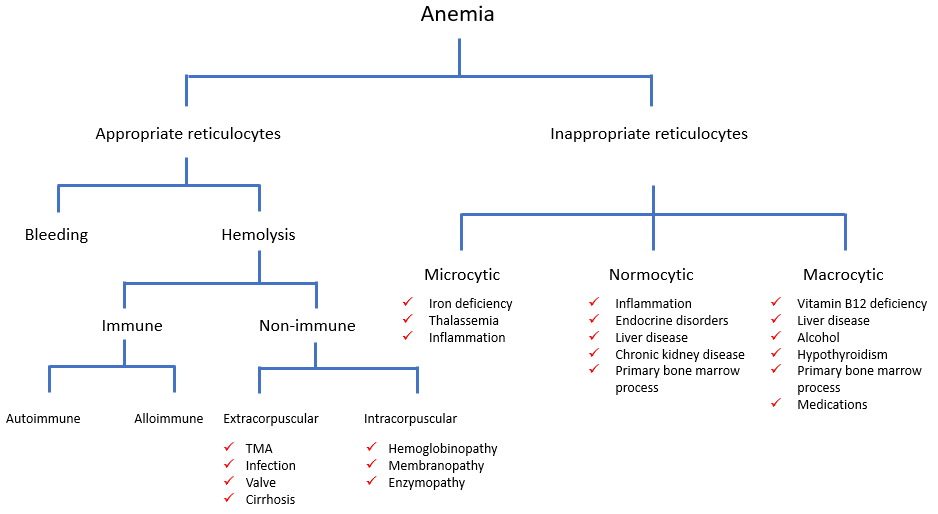
According to this classification, the first test we really want after the hemoglobin – the one that provides the most discriminatory power – is the reticulocyte count. But you will have to wait for that result!
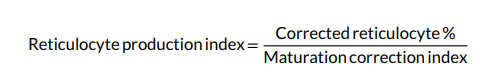
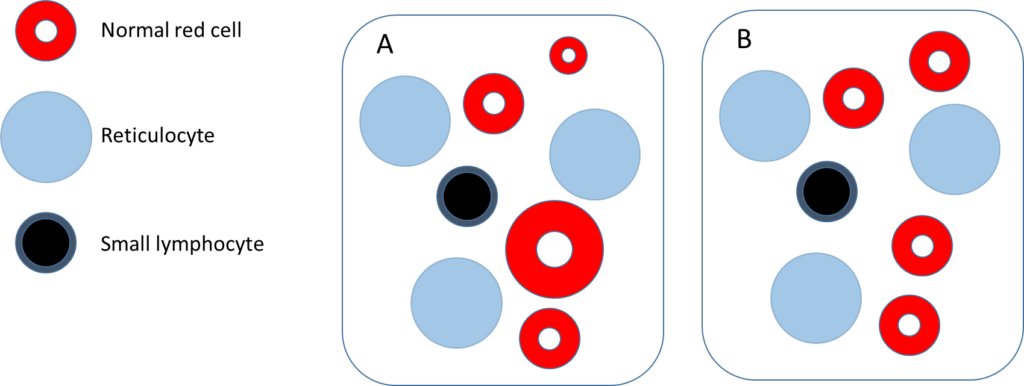
Assuming the elevated mean cell volume (MCV) is caused by reticulocytosis, which of the following 2 schematics is most likely to resemble the patient’s peripheral blood smear?
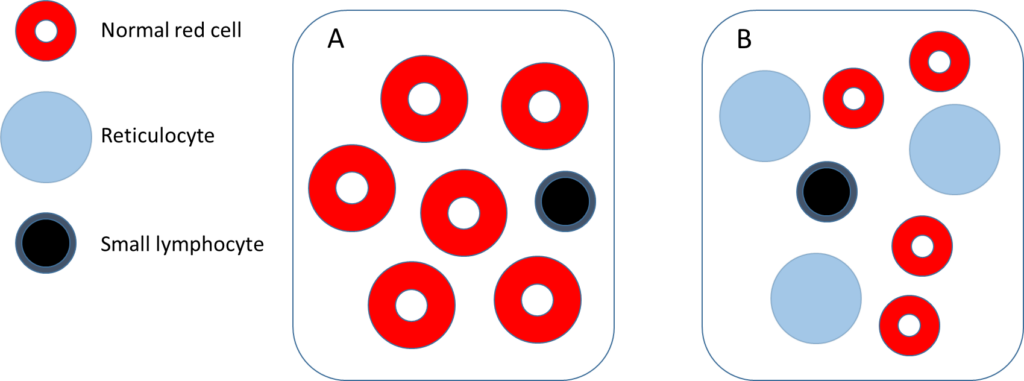
Hint: the diameter of a normal size red cell is approximately the same as the diameter of the nucleus of a small lymphocyte.
Here is the patient’s reticulocyte count:
Reticulocyte count
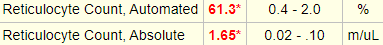
That is, the reticulocyte count is:
- 61.3% of the total red cell count
- 61.3% x 1.65 x 1012/L = 1650 x 109/L
There are several ways of looking at the reticulocyte count:
- As a percentage of red cells
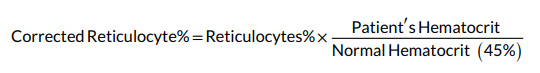
- As a corrected reticulocyte percentage:
- As a maturation correction index, which accounts for a longer life span of the reticulocytes in the peripheral circulation as they take longer time to mature. The maturation correction index varies from 1.0 (Hct 36%-45%), 1.5 (Hct 26%-35%), 2.0 (Hct 16%-25%) to 2.5 (Hct 15% and below).
- As a reticulocyte production index that takes both the Hct as well as the life span of the reticulocytes into account:
See Agarwal AM and Rets A. Int J Lab Hematol. 2020;42(Suppl. 1):107–112
- As an absolute reticulocyte count
- > 120 x 109/L is considered an appropriate response to anemia
Suggestion: Ignore the percentages and focus on the absolute reticulocyte count!
For more information in reticulocytes click here.
Normally, the lab will provide you with an absolute reticulocyte count. If they provide you with only the reticulocyte percentage, what lab value do you need to calculate the absolute count?
Consider the hypothetical patient with a total red cell count of 4 x 1012/L and a reticulocyte percentage of 5%.
Our patient’s mean cell volume (MCV) is 117 fL. Let’s assume that the MCV of the mature red cells is 90 fL. And let’s make the math simple and say that the reticulocyte count is 50%.
This patient has profound reticulocytosis. This degree of reticulocytosis is seen in very few conditions. In fact, there is an extremely high pretest probability for a rare condition, given his history of congenital anemia and this extreme value. But, we will come back to that!
What do you predict the mean corpuscular hemoglobin concentration (MCHC) to be?
Here is the patient’s mean corpuscular Hb concentration (MCHC):
| Parameter | Patient value (g/dL) | Normal range (g/dL) |
|---|---|---|
| MCHC | 30.1 | 32-36 |
This test result is indicative of:
Which smear is most likely to resemble the patient’s?
What do you predict the red cell distribution width (RDW) to be?
Here are are the results of the red cell distribution width (RDW):
Red cell distribution width
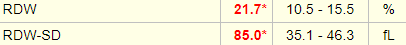
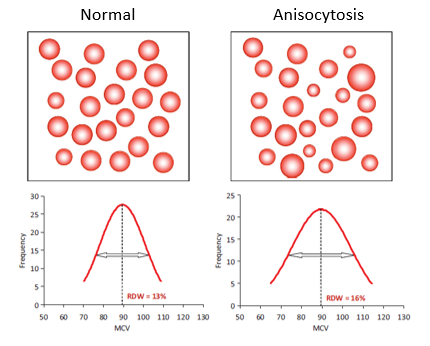
Which RDW is most likely to resemble the patient’s?
Here are are the results of the red cell distribution width (RDW):
Red cell distribution width
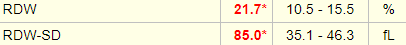
Note that two different RDW values are provided for this patient:
- RDW-coefficient of variation or RDW-CV (abbreviated simply as RDW in the above results)
- RDW-standard deviation or RDW-SD
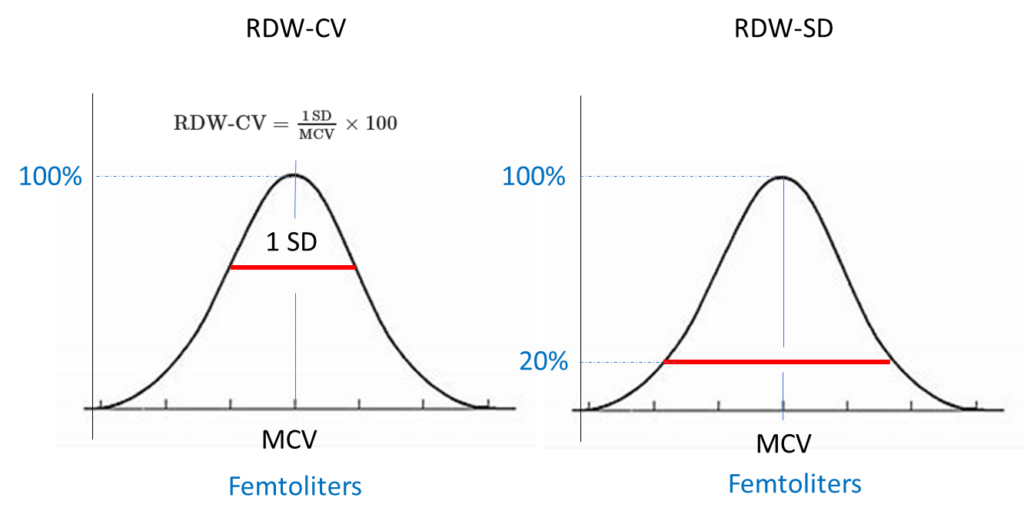
Based on the above information, which RDW measurement is influenced by the mean cell volume?
What should I do if both red cell distribution width (RDW) values are provided?
- Focus on just one of the two values, RDW-CV or RDW-SD. There is nothing to be gained from looking at both.
- The RDW-SD is more accurate than the RDW-CV because the latter is influenced by the mean cell volume (MCV).
- Consider the RDW-SD if it is available.
- RDW-SD > 42 fL is considered increased and is consistent with anisocytosis (there is no such thing as a too-low RDW).
Which smear is most likely to resemble the patient’s?
With rare exceptions, there are two broad causes of reticulocytosis.
There is no reason to suspect that this 29 year-old outpatient with a history of congenital anemia is suddenly bleeding. It is much more likely that the patient has a type of congenital hemolytic anemia. We can divide these into three groups.
Let’s consider each of these categories in turn.
Hemoglobinopathy
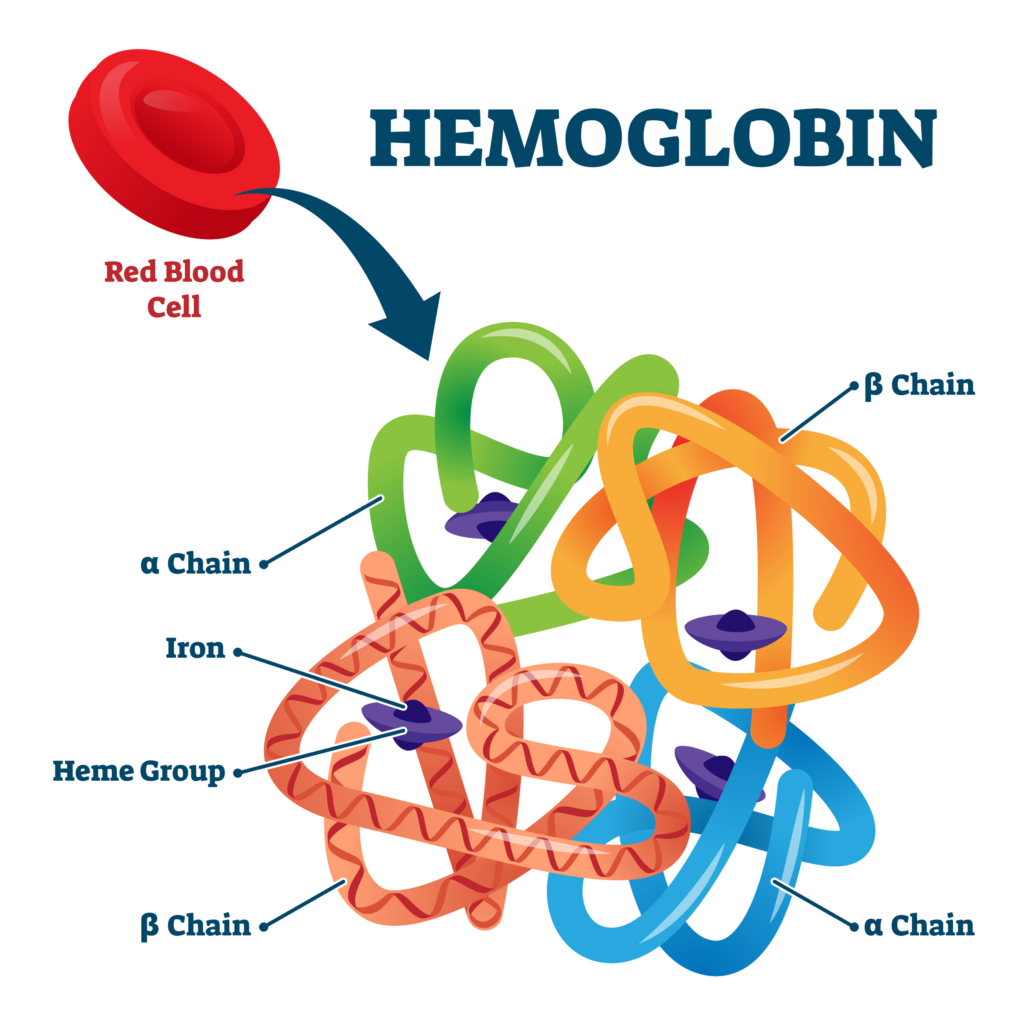
| Condition | Comments |
|---|---|
| Sickle cell disease | Not ruled out so far. |
| Thalassemia | The anemia is too low for thalassemia minor and the mean cell volume (MCV) too high for any type of thalassemia. |
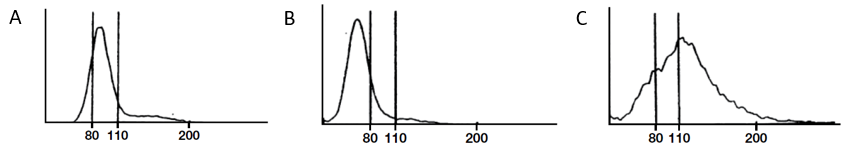
The following are schematics of peripheral blood smears. Schematic A is the one we arrived at after considering the patient’s red cell indices and reticulocyte count.
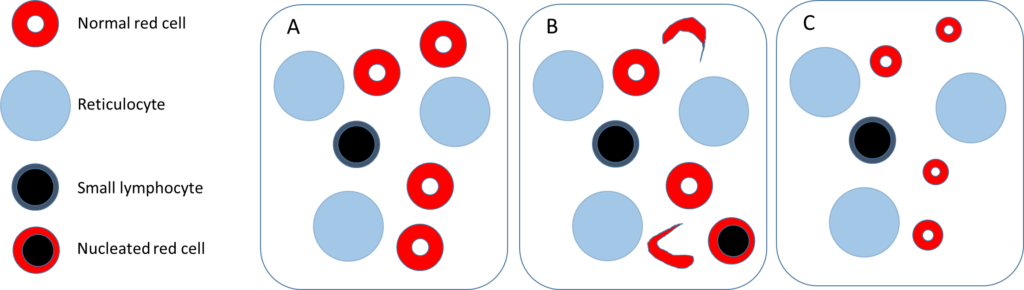
Which statement(s) is/are true?
Membranopathy
| Condition | Comments |
|---|---|
| Hereditary spherocytosis | Not ruled out so far, though the mean corpuscular hemoglobin concentration tends to be high in this condition. |
| Hereditary elliptocytosis | Not ruled out so far. |
| Hereditary pyropoikilocytosis | Not ruled out so far. |
The following are schematics of peripheral blood smears. Schematic A is the one we arrived at after considering the patients red cell indices and reticulocyte count.
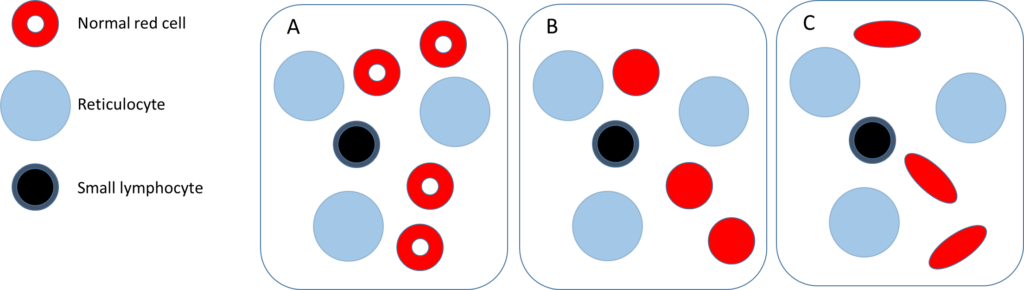
Which statement(s) is/are true?
Enzymopathy
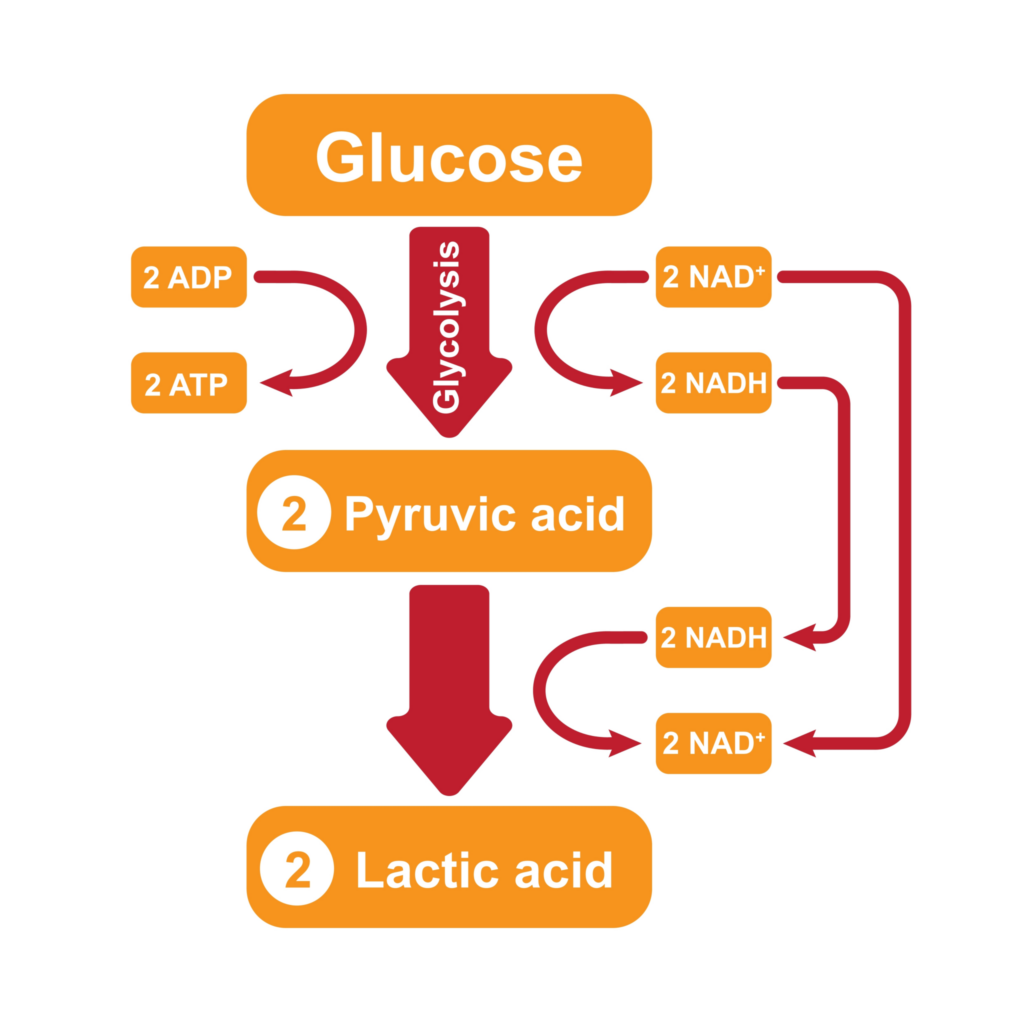
| Condition | Comments |
|---|---|
| G6PD deficiency | Not ruled out so far, though the patient’s current labs would be more consistent with an acute hemolytic crisis. |
| Hereditary pyruvate kinase deficiency | Not ruled out so far. |
The following are schematics of peripheral blood smears. Schematic A is the one we arrived at after considering the patients red cell indices and reticulocyte count.
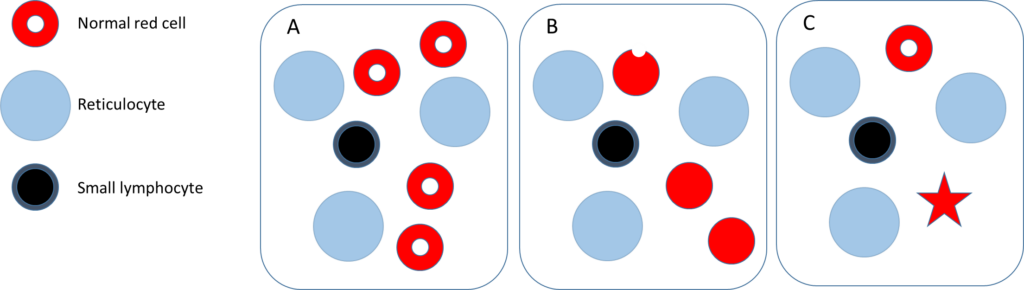
Which statement(s) is/are true?
Before moving on, what do you expect to find in the patient’s serum chemistry (more than once answer may apply):
With these considerations mind, let’s move on to the patient encounter.

