I posted a poll on Twitter asking the following question:
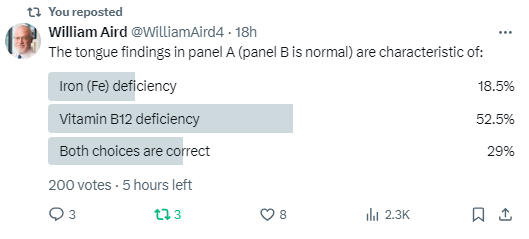
The correct answer is C!
Bottom line
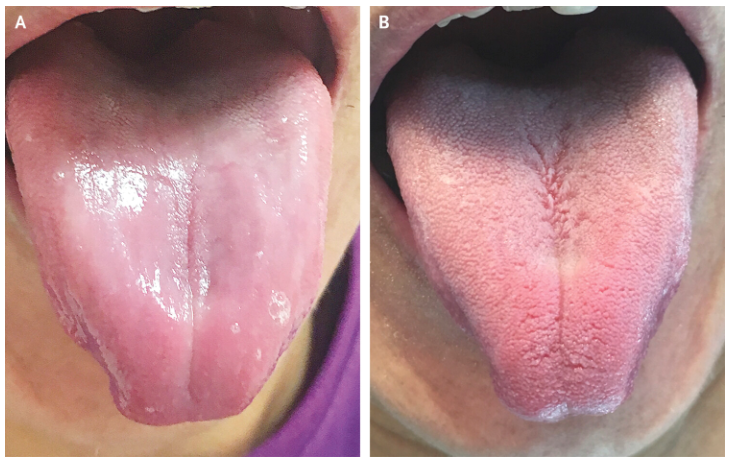
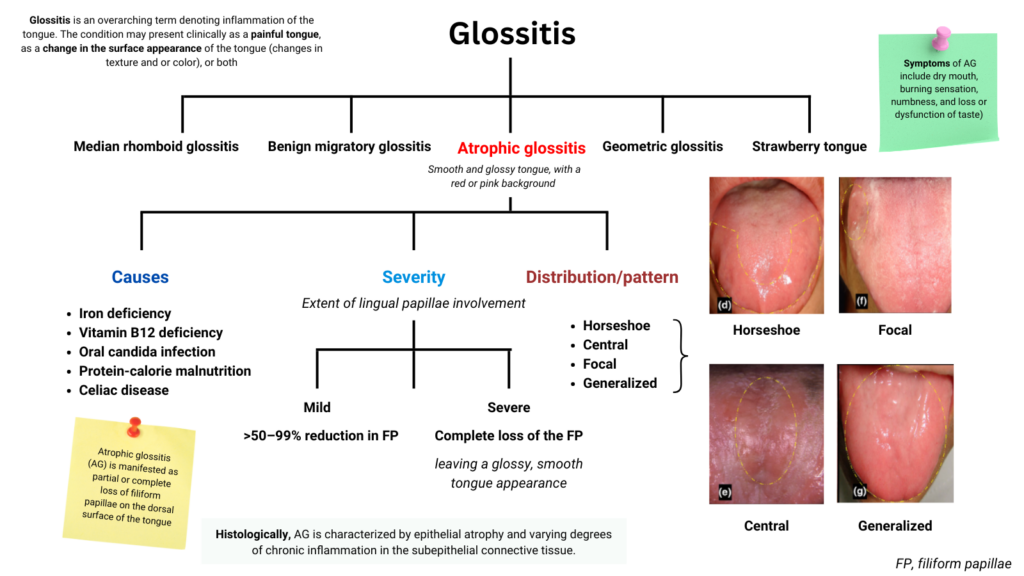
- Atrophic glossitis represents the loss of filiform papillae and (to some extent) fungiform papillae on the dorsal surface of the tongue, resulting in loss of protective function of the papillae, symptoms of burning, pain and dysfunction of taste, and a smooth, glossy appearance with a red or pink background.
- There are many causes of atrophic glossitis. Among these are iron and vitamin B12 deficiency. By contrast, studies have not shown an association with folate deficiency.
- Atrophic glossitis can be categorized according to its severity (mild vs severe) and pattern (focal vs generalized vs U- or horseshoe shaped). Iron deficiency is associated with focal and generalized but not U-shaped, atrophic glossitis.
- The tongue findings are the same in iron and vitamin B12 deficiency with the exception of atrophic linear lesions appearing on the tongue and hard palate that may develop specifically in patients with vitamin B12 deficiency.1
- Most of the published studies on nutrient-associated atrophic gastritis use serum iron, not serum ferritin, as an indicator of iron deficiency, raising questions about the diagnostic accuracy.
- Treatment is nutrient replacement.
Introduction
- The tongue is a mirror of general health or disease.2
- Atrophic glossitis is a condition that occurs when the tongue loses a significant number of papillae. This can cause the tongue to appear smooth and glossy, and may also cause it to be red, edematous, and painful.
Definitions
- Glossitis refers to inflammation of the tongue. The condition may present clinically as a painful tongue, as a change in the surface appearance of the tongue (changes in texture and or color), or both.3
- Atrophic glossitis (AG):
- Represents partial or complete loss of filiform papillae and (to some extent) fungiform papillae on the dorsal surface of the tongue.4
- “Atrophic glossitis is also known as smooth tongue because of the smooth, glossy appearance with a red or pink background. The smooth quality is caused by the atrophy of filiform papillae.”5
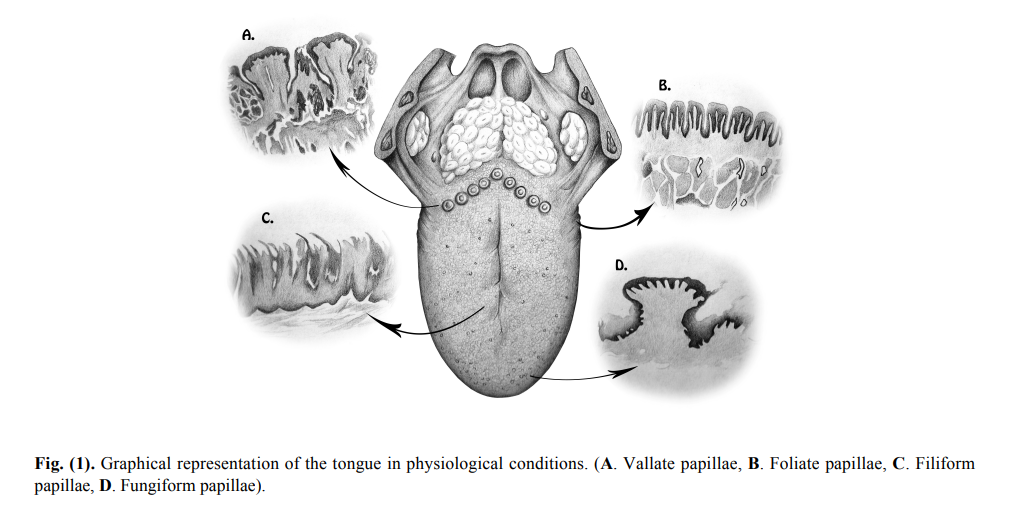
Normal anatomy and function
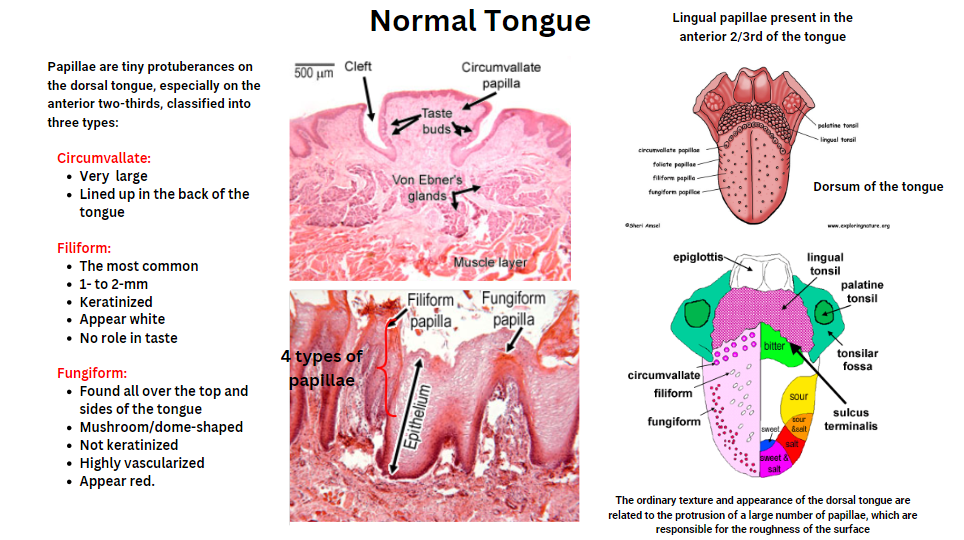
- The normal texture/appearance of the dorsal tongue are related to the protrusion of a large number of papillae, which are responsible for the roughness of the surface.6
- Lingual papillae are small structures on the dorsal surface of the tongue.7
- Filiform papillae:
- Contain a relatively thick layer of keratinized stratified squamous epithelium that can protect the underlying connective and nerve cells from chemical, mechanical and physical stimuli.8
- The usual texture and appearance of the anterior two-thirds of the dorsum of the tongue are predominantly related to the presence of filiform papillae, which are responsible for the roughness of the surface.
- The most common type of papilla
- 1- to 2-mm
- Keratinized
- Appear white
- No role in taste
- Fungiform papillae:
- Consist of plenty of taste cells that are responsible for mainly sweet and salty taste sensations.9
- Found all over the top and sides of the tongue
- Mushroom/dome-shaped
- Not keratinized
- Highly vascularized
- Appear red
- Circumvallate papillae::
- Very large
- Lined up at back of tongue (about 14 of them)
- Filiform papillae:
Epidemiology
- Prevalence of AG in recently admitted elderly patients:10
- 13.2% of men
- 5.6% of women
- Up to 20.3% of AG patients of different types have iron, vitamin B12 and folic acid deficiencies.11
| Deficiency | % AG patients (n=1064) |
|---|---|
| Iron | 16.9% |
| Vitamin B12 | 5.3% |
| Folic acid | 2.3% |
- Atrophic glossitis reported in:
- Up to 25 % of cases of cobalamin deficiency with oral manifestations.12
- About 15-30% of patients with iron deficiency anemia.
Etiology
- Atrophy of the filiform papillae may occur from mechanical damages of the mucosa, or in the setting of systemic or local conditions.13
- Causes of AG include:14
- Nutrient deficiencies:
- Vitamin B12
- Iron
- Riboflavin (B2)
- Niacin (B3)
- Pyridoxine (B6)
- Folic acid
- Zinc
- Vitamin E
- Protein-calorie malnutrition
- Candidiasis
- Helicobacter pylori infection
- Xerostomia
- Diabetes mellitus
- Alcohol abuse
- Celiac disease
- Medications:15
- Anti-diabetics
- Contraceptives
- Acid-lowering agents
- Anti-cancer
- Antihypertensives
- Neurologic drugs
- Nutrient deficiencies:
Pathophysiology
- Atrophic glossitis (AG) is caused by an absence of filiform or fungiform papillae on the dorsal surface of the tongue, causing it to be soft and smooth.16
- When severe, these changes favor the secondary formation of erosions and ulcers, compromising the oral function and provoking symptoms.17
- AG is associated with impaired:18
- Protective function from filiform papillae.
- Taste function from loss of taste buds in fungiform papillae on the dorsal surface and lateral border of the tongue.
- It has been proposed that the burning sensation and numbness of the tongue in patients with AG is caused by the loss of protection of dorsal surface mucosa of the tongue by filiform papillae and easy access of the free nerve ending in the atrophic dorsal surface mucosa of the tongue, respectively.19
Symptoms
- Pain
- Burning sensation
- Numbness of the tongue
- Dysfunction of taste
- Dry mouth
- In a study of 1064 patients with AG:20
- Burning sensation of the tongue in 98.5%
- Dry mouth in 70.1%
- Numbness of the tongue 50.7%
- Dysfunction of taste in 23.5%
Signs
- Tongue findings include:
- Smooth, shiny appearance
- Red or pink color
- Thinning of the tongue surface
- Fissures
Literature
- Drinka et al, 1993
- 30 elderly subjects
- Outcomes:
- Percentage of normal papillary development (%NPD) relative to a reference photograph.
- 16 nutritional blood levels
- Results:
- %NPD correlated significantly (p < 0.0031) with levels of vitamin E and prealbumin, but not with 14 other laboratory indices.
- Subjects with overt atrophic glossitis (%NPD < 50%) tended to have multiple nutritional deficiencies.
- Bohmer and Mowe, 2000
- Randomized population survey of 310 elderly people recently admitted to hospital and 106 randomly selected elderly people at home.
- Outcomes:
- Presence of atrophic glossitis
- Nutritional indices
- Results:
- Atrophic glossitis occurred in:
- 13.2% of men at home
- 5.6% of women at home
- 26.6% of men in hospital
- 37% of women in hospital
- The atrophic glossitis was related to:
- Reduced weight:
- Body mass index
- Triceps skinfold thickness
- Arm-muscle circumference
- Muscular strength, activities of daily living
- Serum concentrations of:
- Cholesterol
- Ascorbic acid
- Cholecalcidiol
- Vitamin B12
- Reduced weight:
- Atrophic glossitis occurred in:
- Sun et al, 2012
- 176 AG patients
- Blood hemoglobin, iron, vitamin B12, folic acid, and homocysteine concentrations and the serum GPCA level in 176 AG patients were measured and compared with the corresponding levels in 176 age- and sex-matched healthy control subjects.
- Results:
- Deficiency found for:
- Hb in 22.2% of cases
- Iron 26.7% of cases
- Vitamin B12 7.4% of cases
- Folate 1.7% of cases
- AG patients had a significantly higher frequency of Hb, iron or vitamin B12 deficiency, of abnormally elevated blood homocysteine level, or of serum GPCA positivity than healthy control subjects (all P-values = 0.000).
- No significant difference in frequency of folic acid deficiency was found between AG patients and healthy control subjects.
- Deficiency found for:
- Wu et al, 2014
- The oral manifestations and mean red blood cell (RBC) count, corpuscular cell volume, RBC distribution width, Mentzer index, and Green and King index as well as blood concentrations of hemoglobin, iron, total iron binding capacity, vitamin B12, folic acid, and homocysteine in 75 IDA patients and in 150 age- and sex-matched healthy controls were measured and compared.
- IDA patients [note: it appears the diagnosis of IDA was made on the basis of serum Fe, not ferritin] had significantly higher frequencies of all oral manifestations than healthy controls (p < 0.001 for all); the five leading oral manifestations for IDA patients were:
- Burning sensation of oral mucosa (76.0%)
- Lingual varicosity (56.0%)
- Dry mouth (49.3%)
- Oral lichen planus (33.3%)
- Atrophic glossitis (26.7%)
- IDA patients had significantly lower mean hemoglobin level, RBC count, corpuscular cell volume, Mentzer index, iron level, and vitamin B12 level (p < 0.001 for all except p = 0.003 for vitamin B12) as well as significantly higher mean RBC distribution width, Green and King index and total iron binding capacity level (p < 0.001 for all) than healthy controls.
- No significant difference in the mean blood folic acid or homocysteine level was found between 75 IDA patients and 150 healthy controls.
- Chiang et al
- 1064 AG patients and 532 age- and sex-matched healthy control subjects.
- Measured the complete blood count, serum iron, vitamin B12, folic acid, homocysteine, and serum GPCA level [note: it appears the diagnosis of IDA was made on the basis of serum Fe, not ferritin].
- Results:
- Microcytosis 7.4%
- Macrocytosis 3.9%
- Deficiency in:
- Hemoglobin 19%
- Iron 16.9%
- Vitamin B12 5.5%
- Folic acid 2.3%
- Esquivel-Pedraza et al
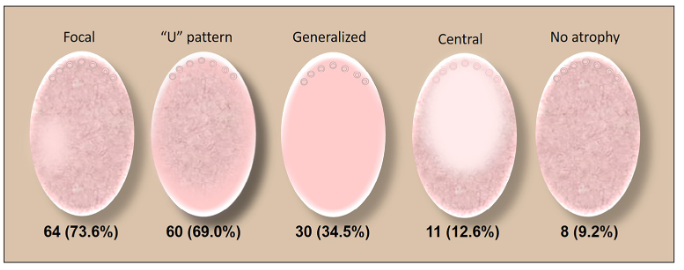
- Cross-sectional, analytical, research study involving systematic tongue examination to evaluate the presence and clinical patterns of FP atrophy.
- 87 patients included from outpatient Mouth Diseases Clinic of the Dermatology Department.
- Inclusion criteria to the study were subjects >18 years old who attended the clinic during the study period
- Atrophy of the FP in 90.8% of the patients:
- Severity:
- Mild in 83.5% of the cases
- Severe in 16.5%
- Pattern:
- Focalized in 73.6% of cases
- “U”-shaped pattern in 69%
- Generalized in 34.5%
- Lower titers of serum iron were detected in cases with focal and generalized FP atrophy (P = 0.03 and P = 0.009, respectively), than their counterparts. On the contrary, subjects with a horseshoe or “U”-shaped pattern had higher serum levels of iron.
- The presence of symptomatology was related to the focal pattern of atrophy (P = 0.038).
- Severity: