
Answer to Case
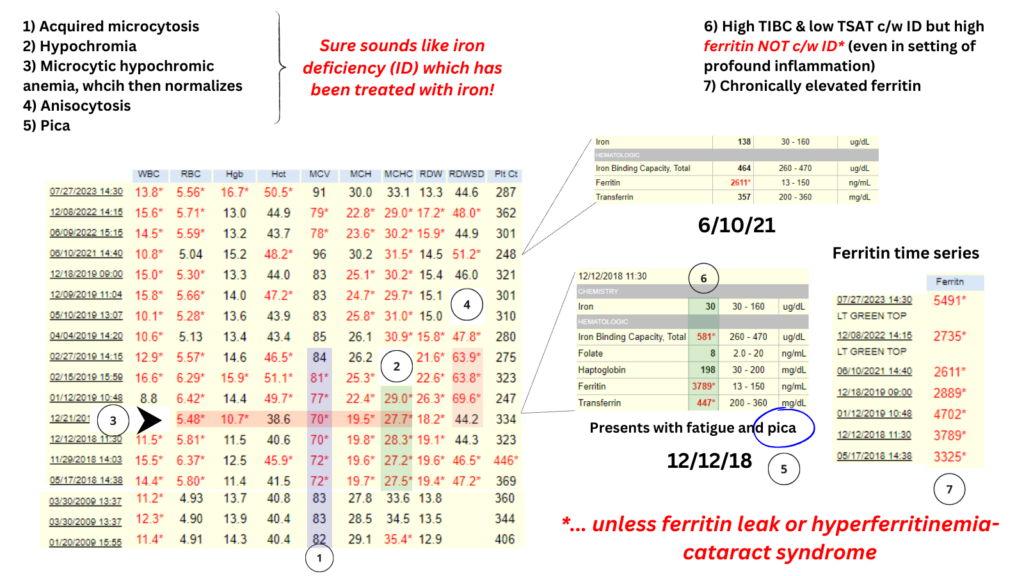
Let’s look at the data a little more closely. Follow along with the numbers on the graphic:
Let’s begin with the CBC:
1. Acquired microcytosis, thus not thalassemia (unless acquired HbH). Iron deficiency (ID) most likely, though cannot r/u anemia of inflammation based on just the MCV.
2. Hypochromia (low MCHC) concomitant with the microcytosis, most c/w ID.
3. On this date patient has microcytic hypochromic anemia…
4. … and presents with fatigue and pica, again highly suggestive of ID.
5. RDW increases as the MCV normalizes, c/w effects of iron supplementation.
Now let’s look at the iron indices:
6) Very high TIBC and low Fe/TSAT, classic for iron deficiency. But ferritin is elevated. As a general rule iron deficiency is NOT present if the ferritin is > 100 ng/ml with RARE exceptions (chronic kidney disease, ferritin leak or hereditary hyperferritinaemia-cataract syndrome [HHCS]).
7) Serum ferritin levels over time reveal chronic hyperferritinemia. This argues against ferritin leak (which occurs in setting of acute cell damage as occurs in in acute hepatitis). Absolute ID has been reported in CKD with ferritins in the hundreds, but not this high.
Why is the ferritin high in HHCS? Because there is a mutation in the IRE of the ferritin L chain gene that renders the mRNA impervious to iron levels in the cell. L chain expression is constitutively active, leading to elevated serum ferritin (in absence of iron overload)!
So, these lab data alone are sufficient to arrive at a tentative diagnosis of HHCS.
This patient did indeed have HHCS. And we proved that she was iron deficient in 2018 based on a markedly elevated zinc protoporphyrin. She was treated with iron, and her symptoms resolved.

