Answer to Case

The correct answer was RBC exchange, which was in fact the least popular choice!
Let’s work through the case.
Follow the numbers in the graphic:
1) Acquired (CBC previously normal)
2) Pancytopenia (all three cell lines down)
3) Appropriate retic response (> 0.12 x 10^9/L) = bleeding or hemolysis
4) Elevated hemolytic markers
5) Elevated ALT (not a hemolytic marker)
So, in summary, the labs show pancytopenia, hemolytic anemia and elevated ALT (the latter indicating something “liver-ish” going on).
If we approach the case from the standpoint of hemolytic anemia (see graphic), the patient is unlikely to have immune hemolysis (would not explain the low platelet count unless he had Evans syndrome).
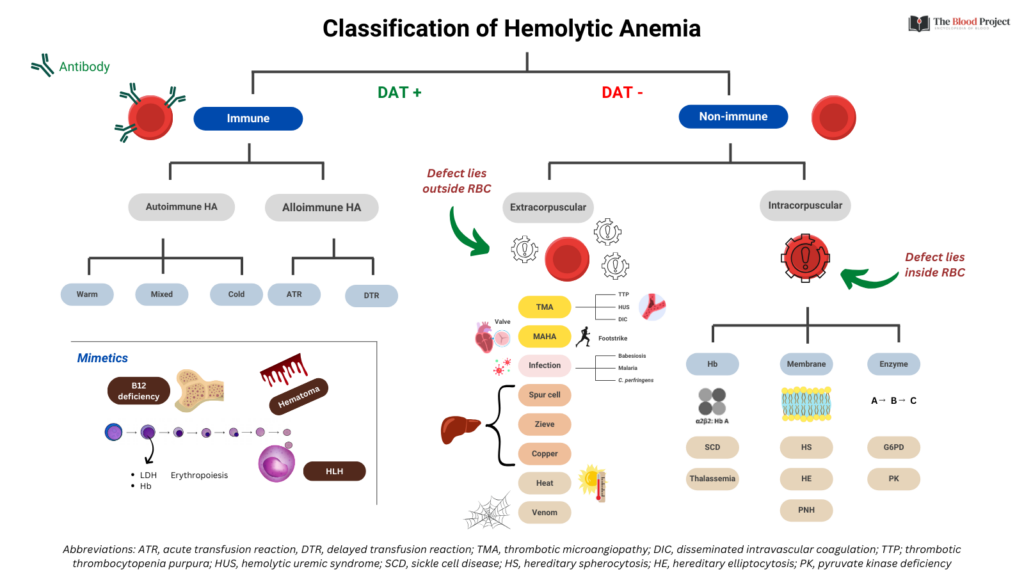
That puts us on the non-immune side (though we would want a DAT/Coombs to be sure). The only causes of intracorpuscular non-immune hemolysis to consider are paroxysmal nocturnal hemoglobinuria (PNH) or acquired G6PD deficiency (the rest are congenital, and this patient’s CBC was previously normal).
That leaves a list of potential causes in the extracorpuscular non-immune bucket. We can narrow these down based on the questions in the poll.
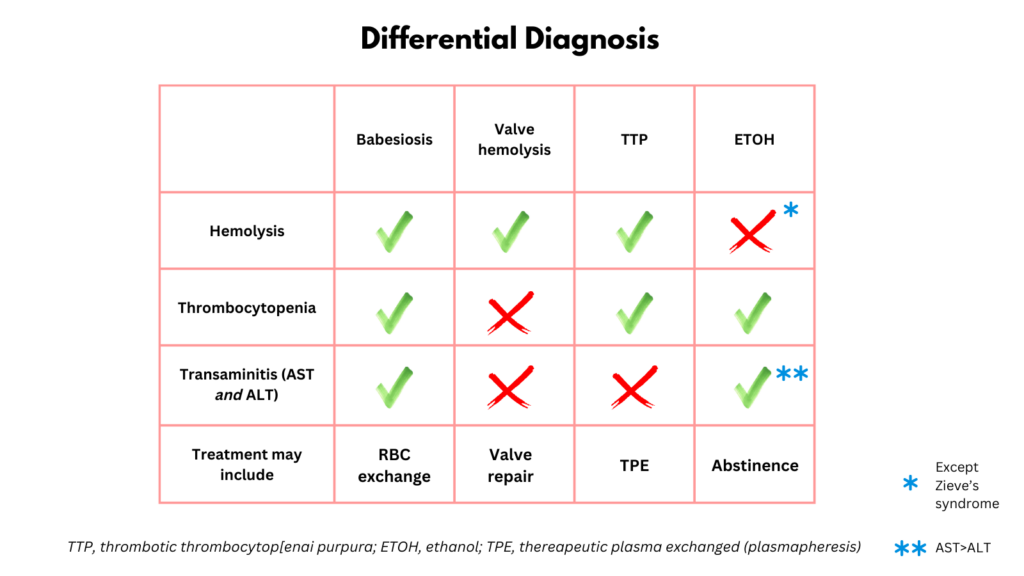
1) RBC exchange – typically used in patients with sickle cell disease (SCD) or babesiosis. The previously normal CBC virtually r/o SCD. Babesiosis is associated with fatigue, loss of appetite and nausea, cytopenias (especially anemia and low PLTs but also low WBC), hemolysis and transaminitis (both AST/ALT).

2) Valve replacement – valve hemolysis is associated with new onset hemolytic anemia, but not thrombocytopenia to this level and not an elevated ALT unless congestive hepatopathy.
3) Plasmapheresis – indicated in acquired thrombotic thrombocytopenia purpura (TTP). TTP would explain the hemolytic anemia and thrombocytopenia (the leukopenia is mild and may simply reflect stress-induced lymphocytopenia), but not the elevated ALT (reported to be rarely affected).
4) Alcohol abstinence – Acute alcohol toxicity can cause cytopenias and elevated AST:ALT. However, hemolysis is rare, typically seen only in Zieve syndrome where the bilirubin tends to be much higher.
The patient did have babesiosis, diagnosed based on parasite smear (15% parasitemia) and treated with atovaquone & azithromycin, and RBC exchange.

The graphic below summarizes an approach to the case based on the limited information that was offered.