
- Definition:
- A rapid, systemic reaction to tissue injury, infection, or inflammation, characterized by a coordinated set of physiological and biochemical changes. It is part of the innate immune response.
- Pathophysiology:
- The acute phase response is initiated when pattern-recognition receptors on immune cells detect microbial products or tissue damage, leading to cytokine release and activation of downstream pathways. Primarily mediated by proinflammatory cytokines such as interleukin-1 (IL-1), interleukin-6 (IL-6), and tumor necrosis factor (TNF).
- These cytokines trigger a cascade that leads to the hepatic synthesis of acute-phase proteins (APPs), including C-reactive protein (CRP), serum amyloid A, fibrinogen, and complement components, while downregulating the production of negative acute-phase proteins such as albumin and transferrin.
- The liver is the principal source of circulating acute-phase proteins, but extrahepatic tissues (e.g., adipose tissue, endothelium, and muscle) also contribute to local and systemic responses.
- The acute phase response not only amplifies innate immunity but also modulates adaptive immune responses and tissue repair.
- Components:
- The response also involves:
- Altered production of plasma proteins (known as acute phase proteins)
- Neuroendocrine changes
- Metabolic changes, including fever
- Hematologic changes
- All aimed at restoring homeostasis and enhancing host defense
- The response also involves:
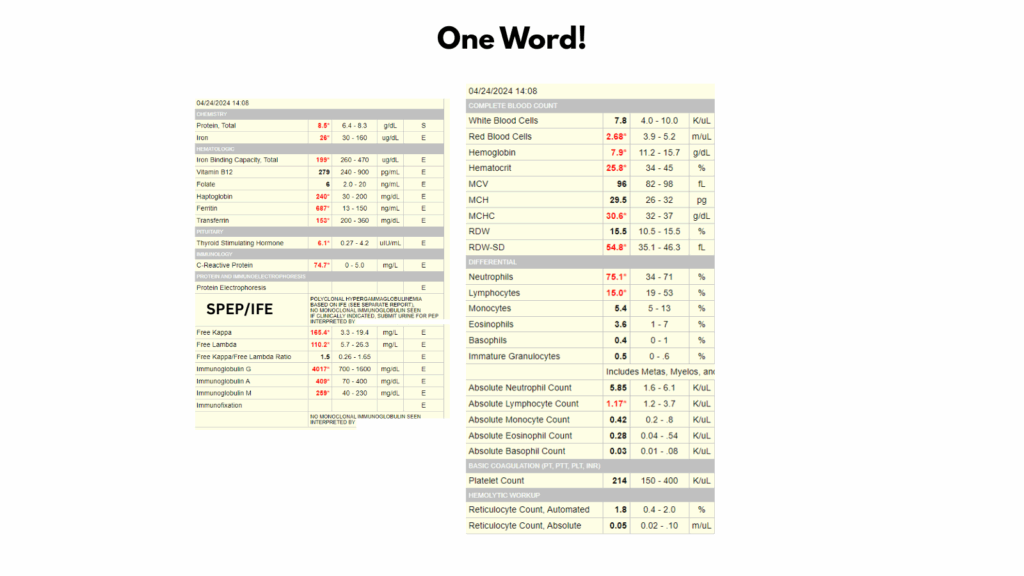
- Acute phase proteins (APPs) are blood proteins whose concentrations change significantly in response to inflammation:
- Increases or decreases in serum levels by at least 25% within 48 hours, driven by cytokines like IL-6, IL-1, and TNF-α.
- Positive APPs (increase in concentration):
- Examples include:
- C-reactive protein (CRP) – opsonization, complement activation
- Fibrinogen – promotes clot formation
- Ferritin – sequesters iron from pathogens
- Mannose-binding lectin (MBL)
- Serum amyloid A – chemotactic and proinflammatory
- Haptoglobin – binds free hemoglobin
- α1-antitrypsin
- Hemopexin – binds free heme
- Certain complement factors
- Examples include:
- Negative APPs (decrease in concentration): Examples include albumin and transferrin. Their reduction may help redirect resources toward producing positive APPs.
- While most acute phase reactants are synthesized by the liver, not all are.
- Primarily made in the liver:
- Hepatocyte expression/stimulation in response to IL-6, IL-1, and TNF-α:
- C-reactive protein (CRP)
- Serum amyloid A (SAA)
- Fibrinogen
- Haptoglobin
- Alpha-1 antitrypsin
- Ceruloplasmin
- Complement components (e.g., C3, C4)
- Hemopexin
- Ferritin (mostly liver, but also macrophages)
- Sinusoidal endothelial cells:
- FVIII
- Hepatocyte expression/stimulation in response to IL-6, IL-1, and TNF-α:
- Non-liver sources of acute phase reactants:
- von Willebrand factor – Endothelial cells and megakaryocytes
- Primarily made in the liver:
- Hematology aspects of the acute phase response:
- Leukocytosis – Especially neutrophilia, often with a left shift (↑ bands)
- Mild normocytic anemia – Called anemia of inflammation or anemia of chronic disease
- Thrombocytosis – Reactive thrombocytosis due to IL-6 stimulation of hepatic thrombopoietin and megakaryopoiesis
