Postscript
Zieve syndrome is an alcohol-related hemolytic anemia in patients with and alcoholic steatohepatitis. It is characterized by the triad of:
- Hemolytic anemia
- Hyperlipidemia
- Jaundice
History of Zieve syndrome
In 1958, Leslie Zieve published data on 20 alcoholic patients seen at the Minneapolis Veterans Hospital during a period of eight years 1. The complex of jaundice, hyperlipidemia and hemolytic anaemia in association with moderate alcoholic liver disease (alcoholic fatty liver and cirrhosis) was ‘so strikingly similar’ that he concluded that this clinical picture was a ‘definite syndrome’. Importantly, the findings resolved following alcohol abstinence.

The following are the pertinent findings from Zieve’s study:
- Retrospective analysis of 20 patients, all male.
- Age range 26-65 years – average age 39 years.
- All patients were chronic alcoholics.
- Most complained of severe upper abdominal pain, either in right upper quadrant or epigastrium.
- The liver was enlarged, usually markedly, and generally receded rapidly (spleen was either not palpable or barely palpable).
- Liver tests were only mildly altered, typically during the first or second week following admission, improving thereafter.
- Hyperlipidemia:
- 10 patients had cloudy or milky serum.
- 6 others had elevated serum cholesterol was elevated (400 to 720 mg per cent).
- Cholesterol elevation > 500 mg/100 ml was observed in 60% of patients.
- Serum cholesterol normalized on average by the sixth week.
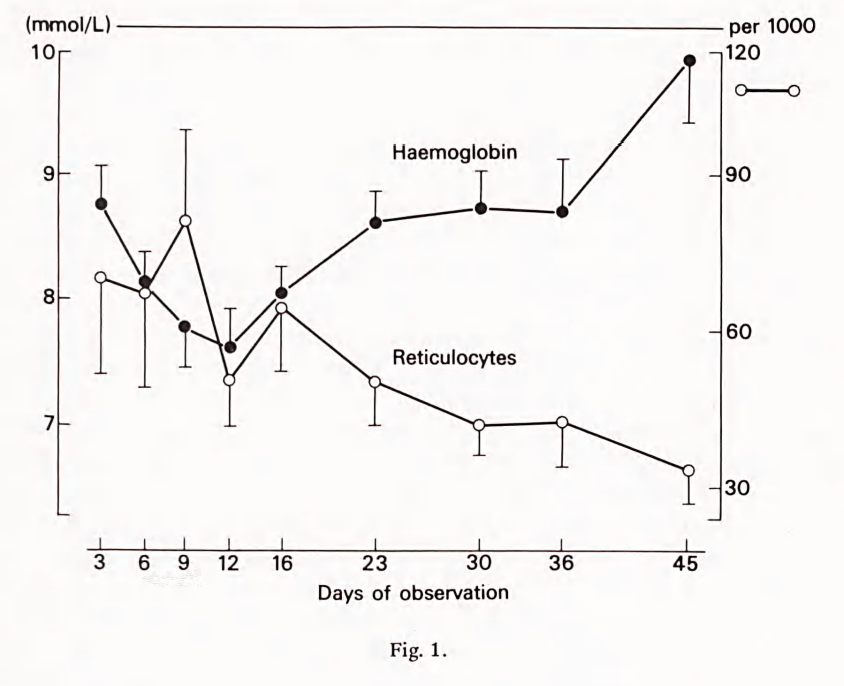
- Hemolytic anemia:
- All patients had elevated reticulocytes.
- Most had macrocytosis with average mean cell volume (MCV) 105 fL.
- Bone marrow studies were obtained in eight patients, six of whom had marked erythroid hyperplasia with over 50% normoblasts.
- Average interval to near-normal hemoglobin values around five weeks.
- Jaundice:
- Uniformly present.
- Improvement in the jaundice was rapid, near-normal values being recorded on the average by the third week.
- Of the 16 patients who underwent liver biopsy, fatty infiltration was present in 88%. Cirrhosis, if present was mild to moderate.
- There was rapid improvement of the patients with symptomatic treatment only, and return of the laboratory findings to normal values after about four to six weeks.
- Zieve proposed that
- The lipemia follows the release of lipid from the fatty liver during the early phase of the healing process.
- Abnormal circulating lipid levels – possibly lysolecithin – altered red blood cell membranes and predisposed erythrocytes to hemolysis were involved.
Zieve summarized his findings as follows:
The hemolytic anemia in the syndrome of this report is of brief duration, not associated with prominent or persistent hepatic dysfunction, not associated with a prominent spleen, but associated with transient hyperlipemia or hypercholesterolemia.
Other cases were soon recognized elsewhere but it was Leizor Kessel’s publication from the State Veterans’ Hospital in Rocky Hill Connecticut in 1962 of a cohort of 6 similar cases that introduced the term Zieve’s syndrome for the first time.2
In 1968, Balcerzak published a prospective study of 6 men with an illness having features described by Zieve, corroborating the latter’s findings.3. He used cross-transfusion experiments to show that normal donor cells were consistently impaired during the acute illness… clearly [indicating the presence of] an extracorpuscular defect.”
In 1977, reflecting on the literature since Zieve’s publication, Benraad et al commented:4
These studies do not contain fresh arguments to confirm or deny Zieve’s concept of a definite syndrome.
They then go on to describe 11 patients (6 men, 5 women, all alcoholics) with the classic presentation of Zieve syndrome in a period of 42 months. They concluded:
Our data illustrate that in a period of still increasing alcohol abuse, the diagnosis of Zieve’s syndrome should be a matter of concern to every physician, general practitioner, surgeon and, last but not least, general internist.
Since that time, most published references to Zieve syndrome have been case reports. A PubMed search in September 2022 using the term Zieve syndrome yielded a total of 136 papers.
What do we know about Zieve’s syndrome?
Clinical presentation:
- Patients with Zieve syndrome present with the triad of anemia, jaundice and hyperlipidemia in the setting of alcohol abuse and liver disease.
- The presence of hemolysis due to Zieve’s syndrome should be suspected in any alcoholic patient with new-onset anemia and polychromatophilia (polychromasia) seen on a peripheral blood smear.
- There is a marked variability of the clinical picture and of the biochemical and histological findings.
- Most patients have pain in the upper abdomen (they may present as an acute abdomen). The pain has been characterized as:
- Crampy or dull
- Changing in localization but always in the upper part of the abdomen
- Independent of meals
- Lasting for minutes or hours
- Some patients also present with anorexia and vomiting.
- Many patients have constitutional symptoms, including:
- Loss of appetite
- General weakness
- Fatigue
- Fever
- Liver (but not spleen) is typically palpable and enlarged.
- Hemolytic anemia distinguishes Zieve syndrome from acute alcoholic hepatitis
- Absence of spur cells and end stage cirrhosis as well as the presence of hyperlipidemia distinguish Zieve syndrome from spur cell anemia. Moreover, Zieve syndrome is transient and reversible, whereas spur cell anemia is progressive and portends a high short-term mortality.
Hyperlipidemia:
- Only 50% of patients are lipemic at the time of diagnosis. Zieve proposed that this is likely due to the delay in presentation or diagnosis, since the abnormal lipid profile trends down and normalizes within 1–2 weeks.
- The lipid levels remain high enough to cause a cloudy or milky serum only for a very short time, usually from one to several days.
- Serum cholesterol concentration can exceed 1000 mg/dl.
- The reported pattern of lipid abnormalities is highly variable.
- Suggested mechanisms include:
- An episode of massive mobilization of fat to or from the fatty liver and dysregulated blood lipids due to damaged pancreatic alpha cells, as alcohol also damages the pancreas.
- Lipoprotein lipase deficiency
- Alcohol-induced injury of the red blood cell membrane with resultant hemolysis, consequent release of lipid from denatured membranes into the circulation causing hyperlipidemia.
Jaundice:
- The hyperbilirubinemia seen in patients with Zieve syndrome is often profound.
- Jaundice of this triad is caused mostly by direct bilirubin elevation, which suggests cholestasis caused by liver damage in alcoholism as the main reason instead of hemolytic anemia.
- Zieve observed that once the patients stopped consuming alcohol, their jaundice improved relatively quickly; in most of the patients, jaundice resolved by the third week of hospitalization.
Hemolytic anemia:
- A type of alcohol-related hemolytic anemia.
- Associated with reticulocytosis.
- Generally mild and short-lived (Hb normalizes over time).
- Hemolytic anemia may be absent if bone marrow activity compensates for the loss of red cells.
- The red cell fragility is frequently normal.
- The hemolytic anemia was explained by Zieve as due to an abnormal lipid, probably lysolecithin.
- Other hypotheses include:
- Acquired pyruvate kinase deficiency – pyruvate kinase instability induced by vitamin E deficiency, leading to:
- Decreased red blood cell adenosine triphosphate concentrations
- Increased 2,3- diphosphoglycerate levels
- Decreased glucose utilization
- Alterations in the lipid composition of the red blood cell membranes, including increased:
- Cholesterol levels
- Polyunsaturated fatty acid levels
- Lipid peroxidation
- Acquired pyruvate kinase deficiency – pyruvate kinase instability induced by vitamin E deficiency, leading to:
- In the presence of hemolysis, circulating reticulocytes may be accompanied by the presence in circulation of several other types of red blood cells including target cells, acanthocytes [spur cells], echinocytes [burr cells], and stomatocytes. The precise pathogenesis of each of these cell types is uncertain but when continuously present in blood their presence usually indicates the presence of more advanced liver disease. Their presence in Zieve’s syndrome is uncommon and not essential to the diagnosis.
Treatment:
- Supportive
- Alcohol abstinence
- Plasmapheresis has been used to reduce triglyceride levels in patients with Zieve syndrome.5
Prognosis:
- Symptoms typically resolve in 4–6 weeks with alcohol abstinence and conservative therapy. Plasmapheresis is indicated in high-risk patients with severely elevated lipid level, a history of pancreatitis, and intracerebral hemorrhage due to increased risk for complication from the hypertriglyceridemia
- Most patients will recover 4 to 6 weeks after alcohol withdrawal.
Broader context
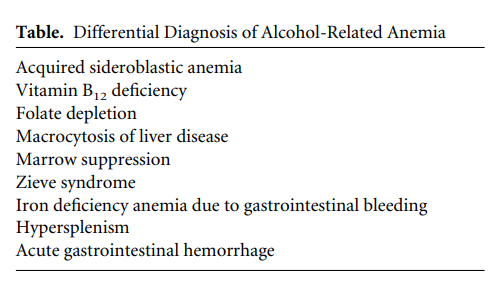
Liver disease and anemia:
Up to 70% of cirrhotic patients have anemia. The pathogenesis of anemia in cirrhosis is complex and multifactorial, and includes:
- Portal hypertension- induced splenic sequestration (hypersplenism)
- Alterations in erythropoietin
- Hemolysis
- Spur cell anaemia
- Zieve syndrome
- Transitory stomatocytosis
- Bone marrow suppression
- Vitamin deficiencies
- Occult or chronic bleeding from varices or gastropathy
Alcohol and anemia:
Alcohol per se may lead to changes in red cell precursors as well as anemia:
- May depress erythrocyte production
- May lead to vacuolated red cell precursors and/or sideroblasts in marrow
- Megaloblastic changes may be observed in connection with malnutrition and folate deficiency
Controversy: is Zieve syndrome a real entity?
The existence of a syndrome akin to Sieve’s original description has been questioned over the years. Zieve himself captured the initial skepticism in a reflective piece he wrote in 1983 for “This Week’s Citation Classic” in Current Contents. It is worth reading the passages below in full because they nicely summarize the nature of his discovery and its aftermath:
In 2006, Adrian Reuben wrote:
With this frame of reference, it is worth recalling that almost 50 years ago, the first description of a syndrome of hemolytic anemia, jaundice and hyperlipemia associated with alcoholic fatty liver and cirrhosis was reported, which later started a controversy that has not yet been completely resolved… After a latent period of indifference to the initial publication that ended with interest kindled 4 years later, two opposing camps formed of those who accepted that there is a distinct constellation of jaundice, hyperlipidemia and transient hemolytic anemia in some patients with alcoholic fatty liver cirrhosis, and of skeptics, who dismissed the “so-called Zieve’s syndrome” as representing an association of common independent occurrences in alcoholic patients… Reams have been published about the interrelationships between alcohol abuse, liver disease, lipid metabolism and hematological disorders. And yet it is still difficult to tell whether Zieve’s original syndrome truly represents a unique clustering of pathological findings. For what it is worth, most hematologists that the author questioned were inclined to think that it is.
