Approach to the Case
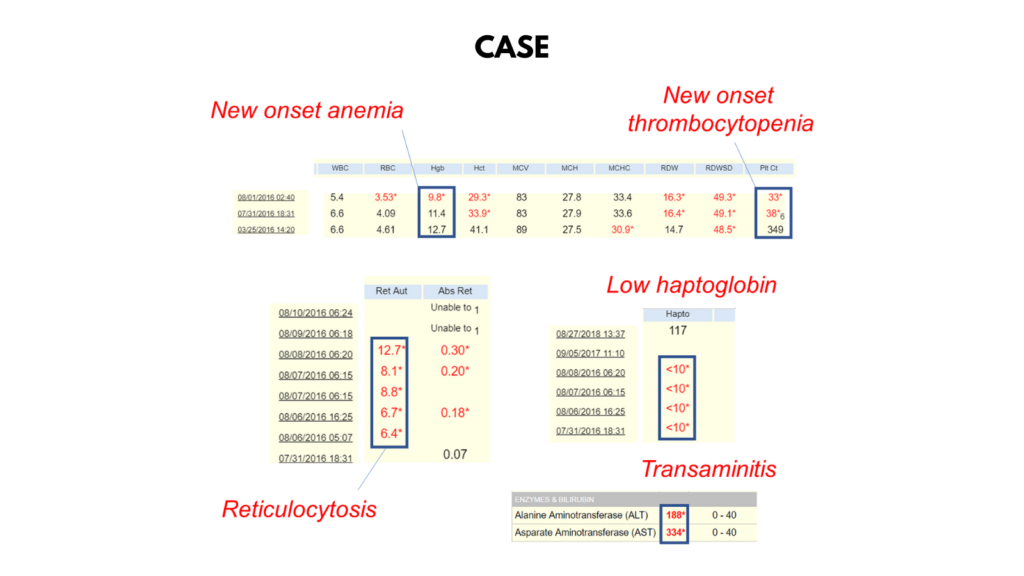
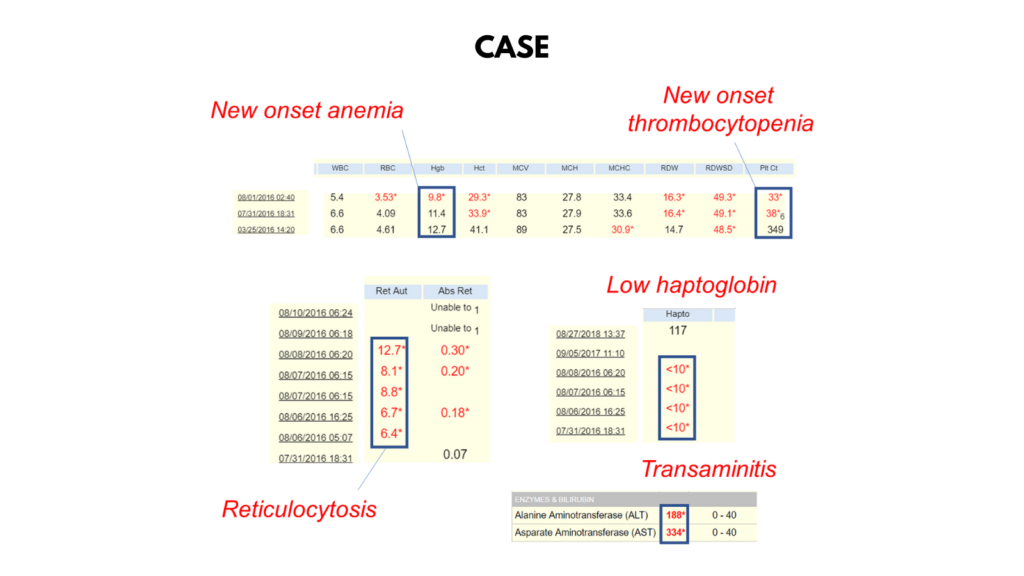
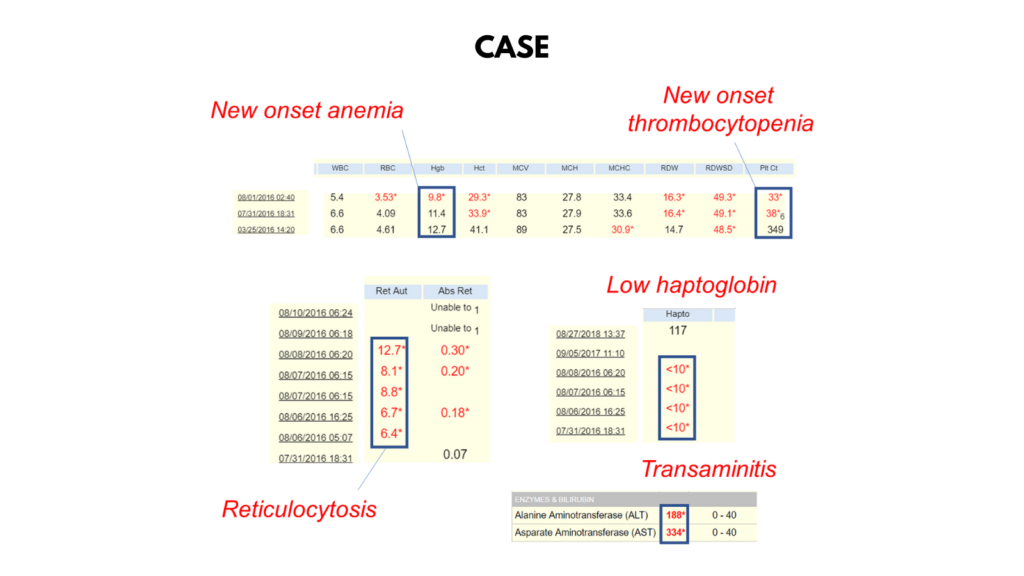
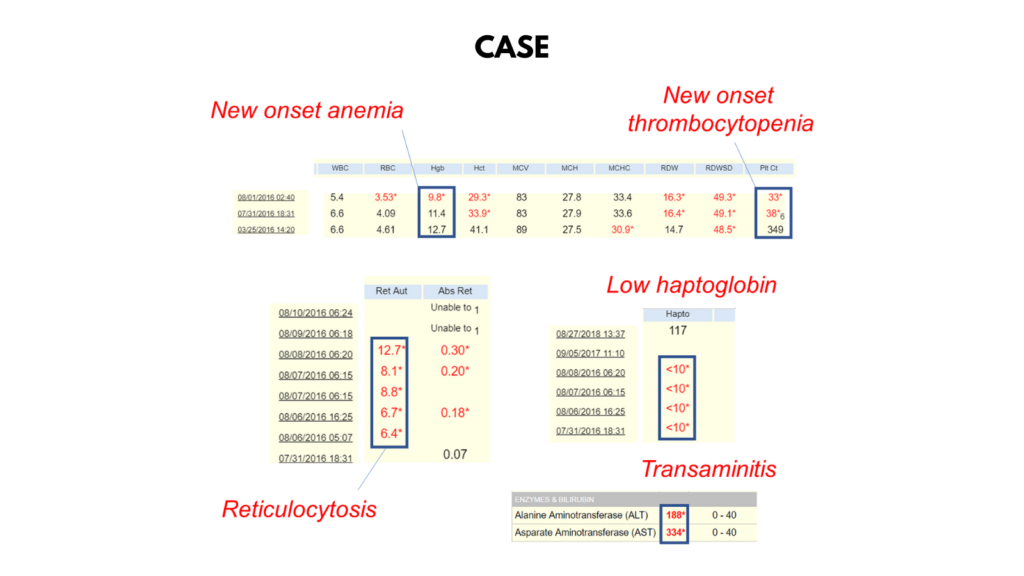
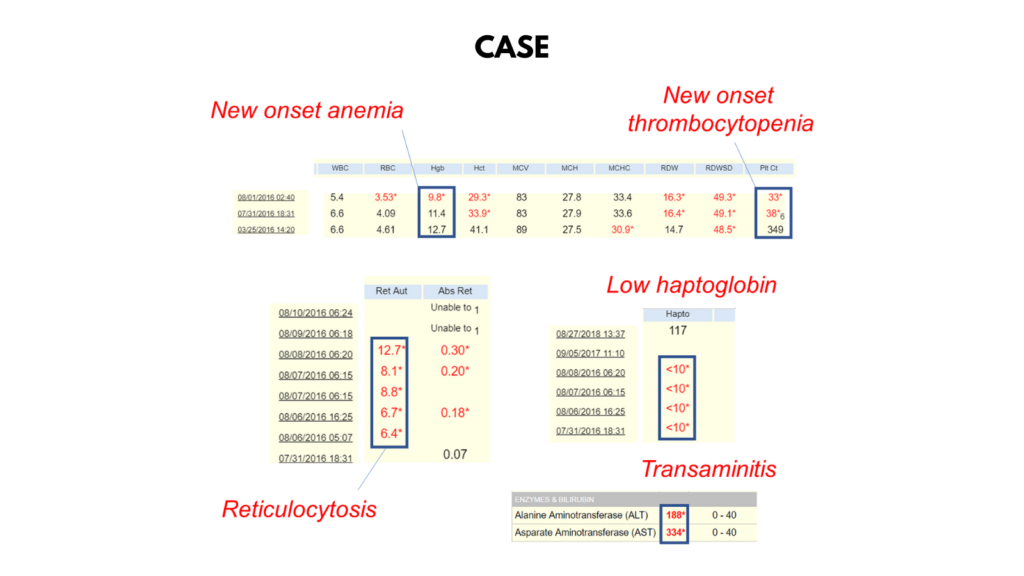
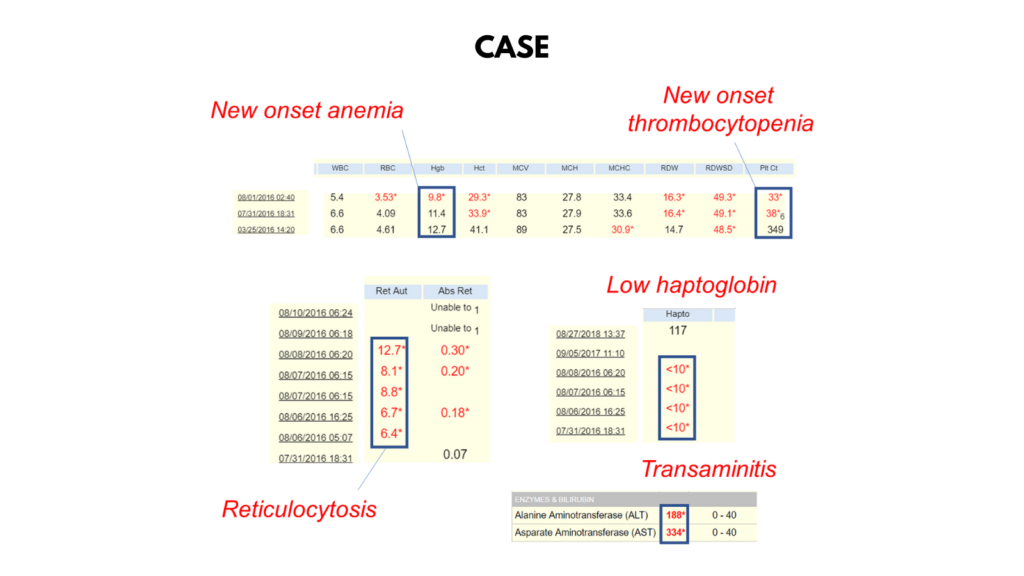











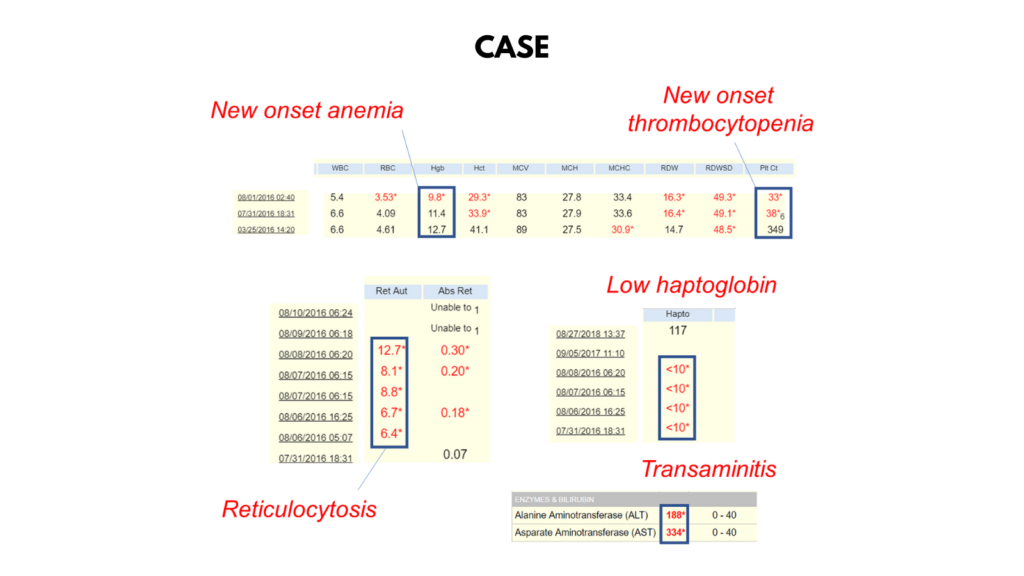
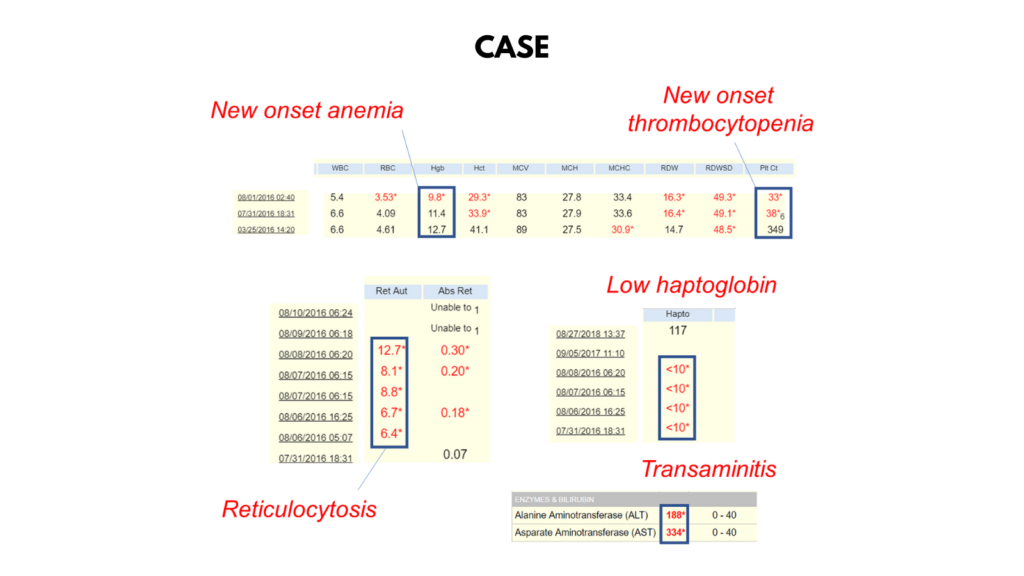
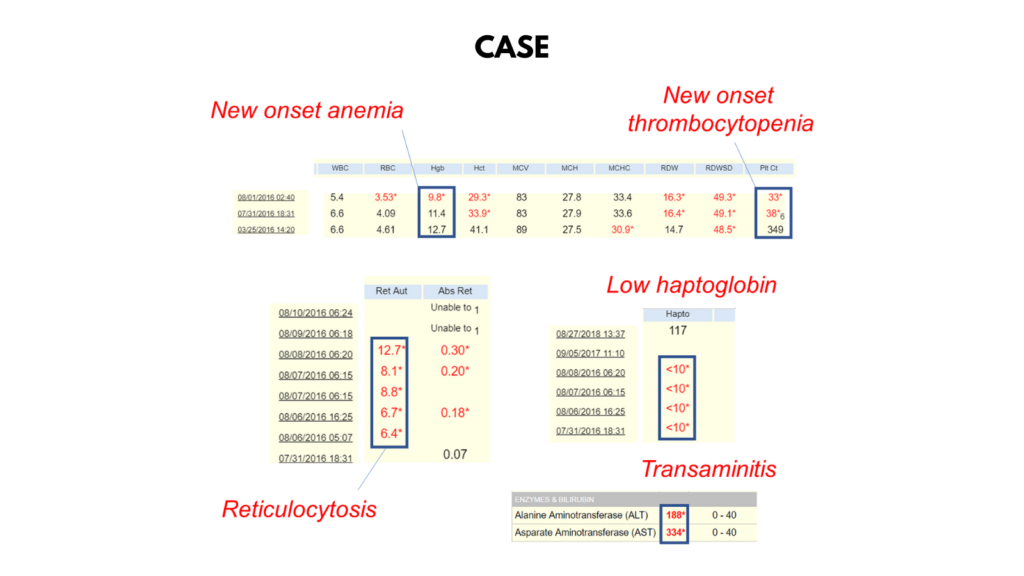
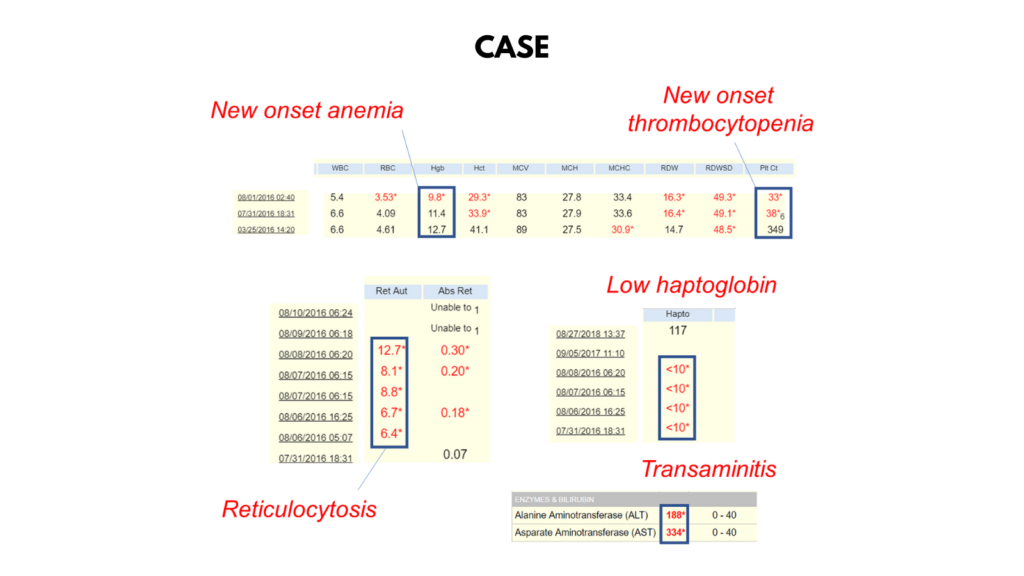
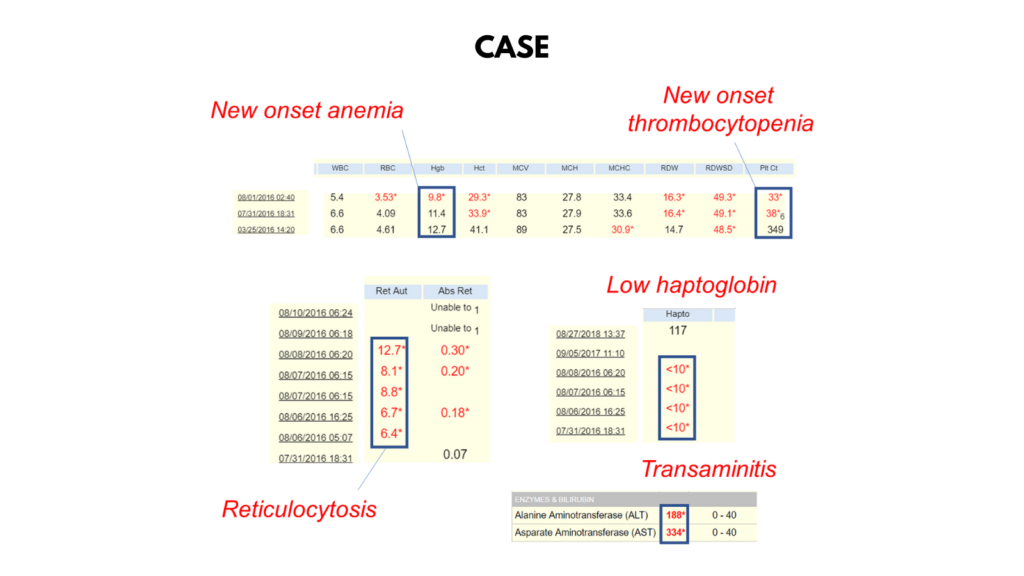
The Hb dropped from 11.4 to 9.8 g/dL in just one day. Is this because the bone marrow shut down?
Click for Answer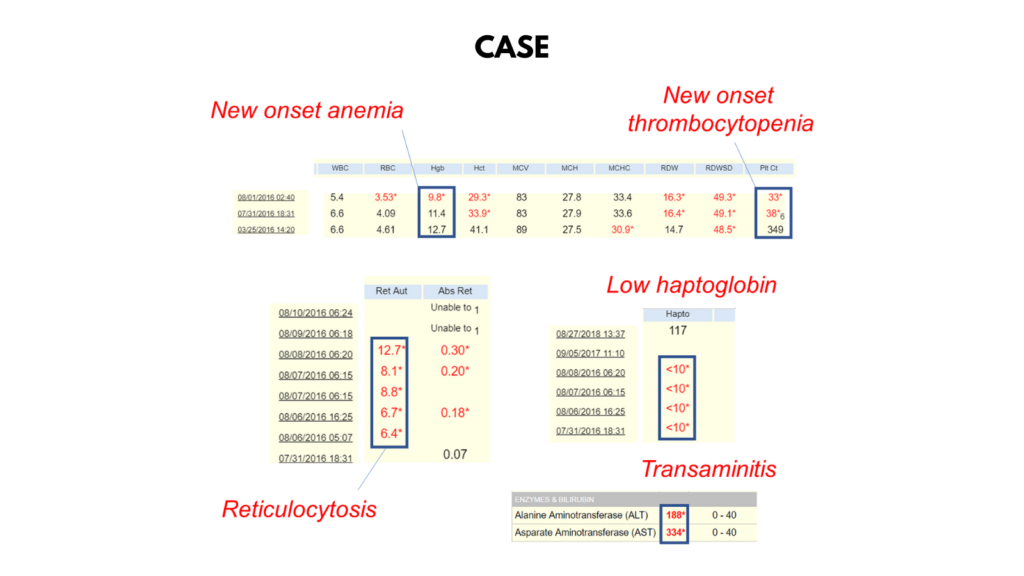
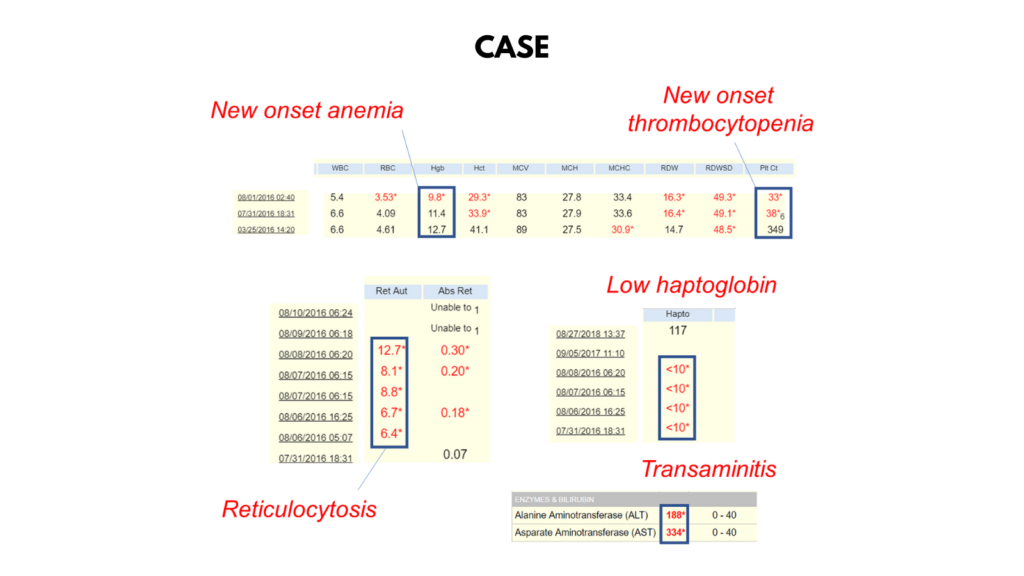
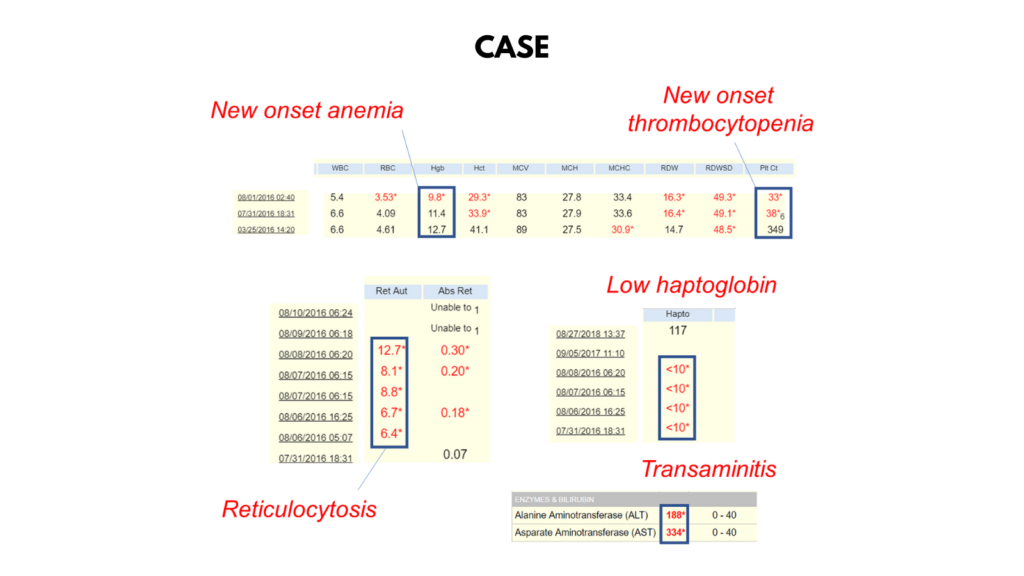
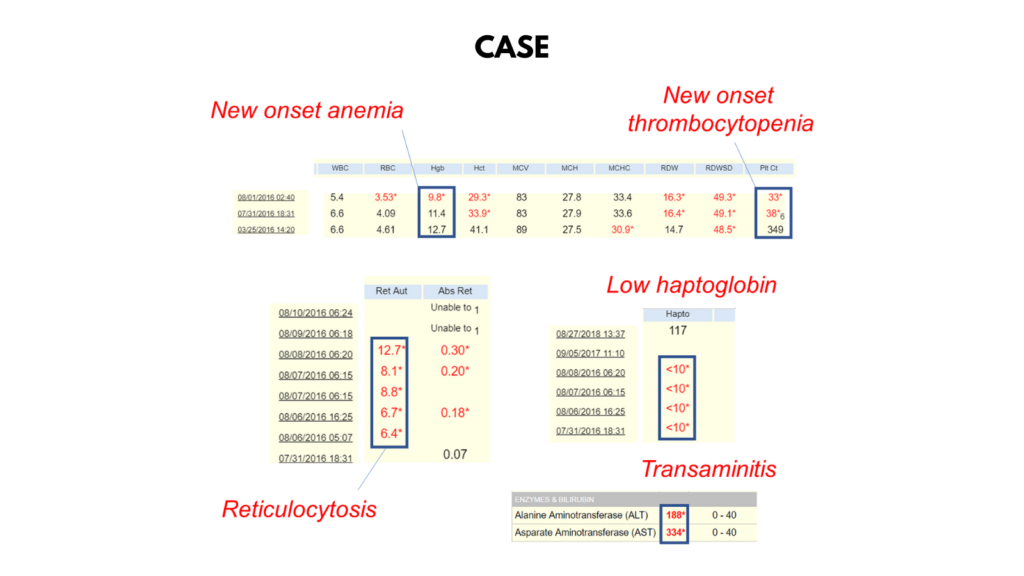
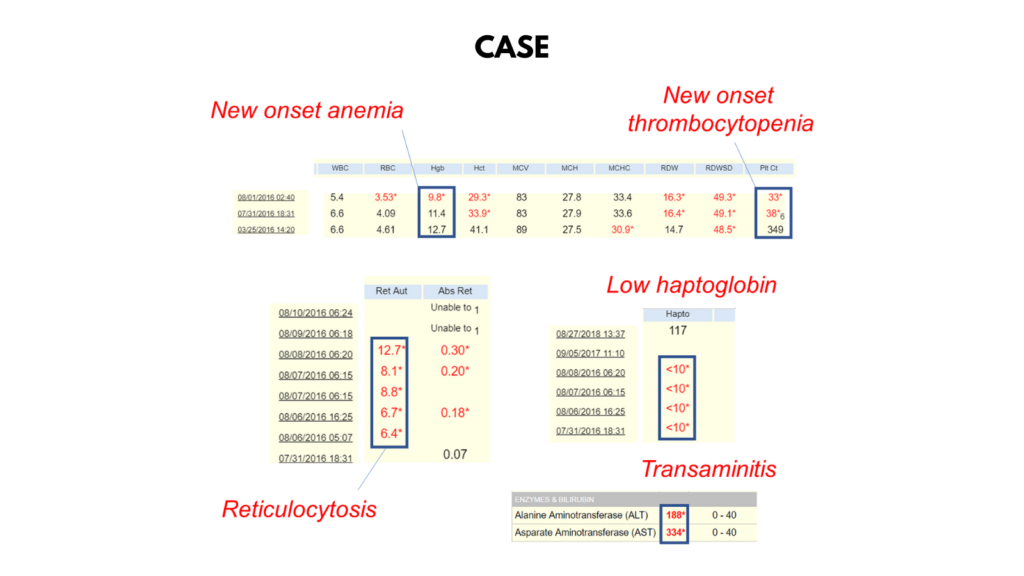
Which of the following data support a diagnosis of hemolysis?











Assuming that the patient has hemolysis, is it likely to be congenital or acquired?
Click for Answer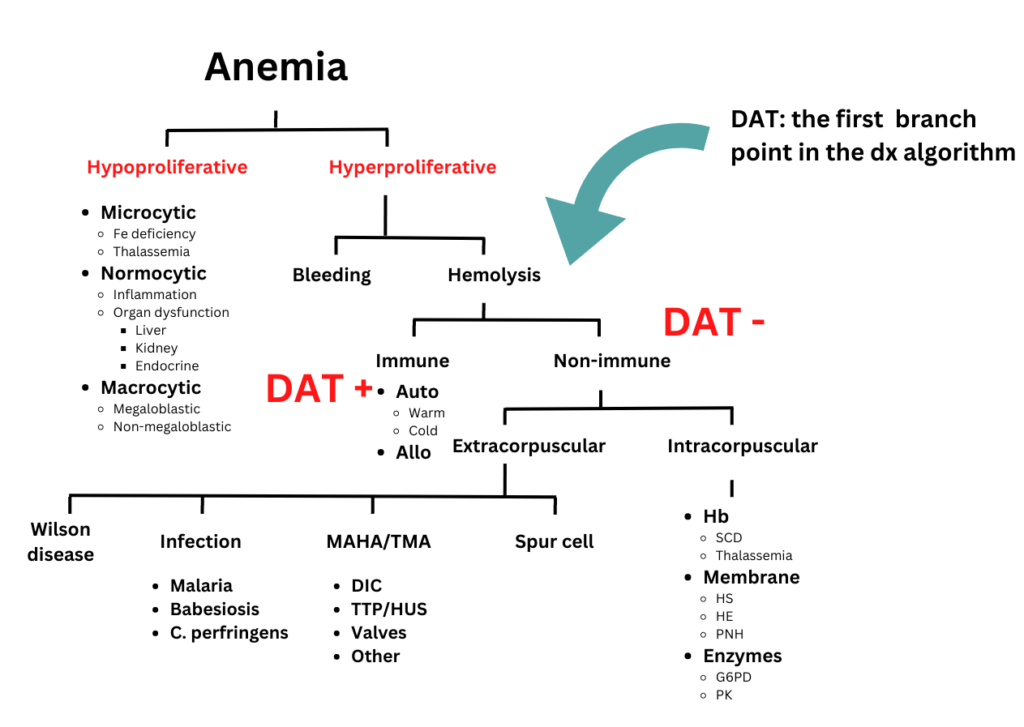
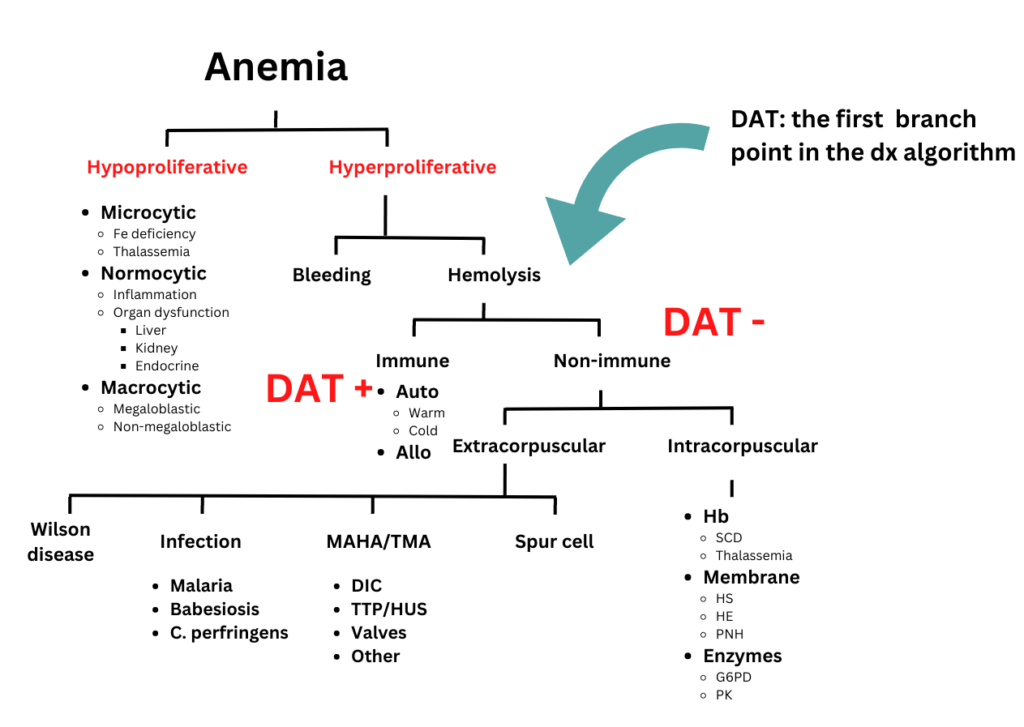
You will not be provided with the result of the DAT 🙂
The patient also has thrombocytopenia.











If the patient were an outpatient, what are some causes of thrombocytopenia to consider?
Click for Answer










If the patient developed thrombocytopenia while in hospital, what are the top 2 considerations?
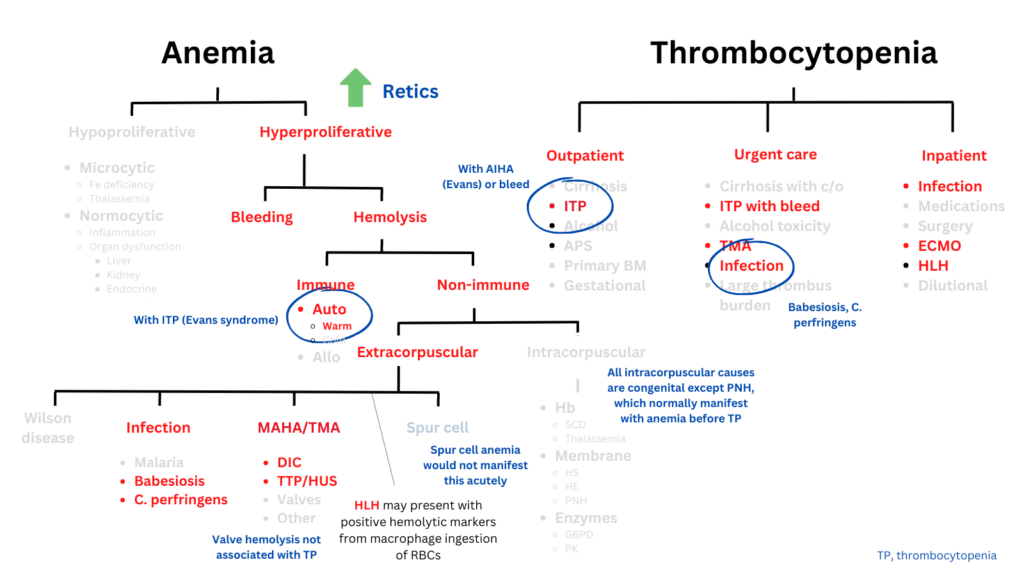
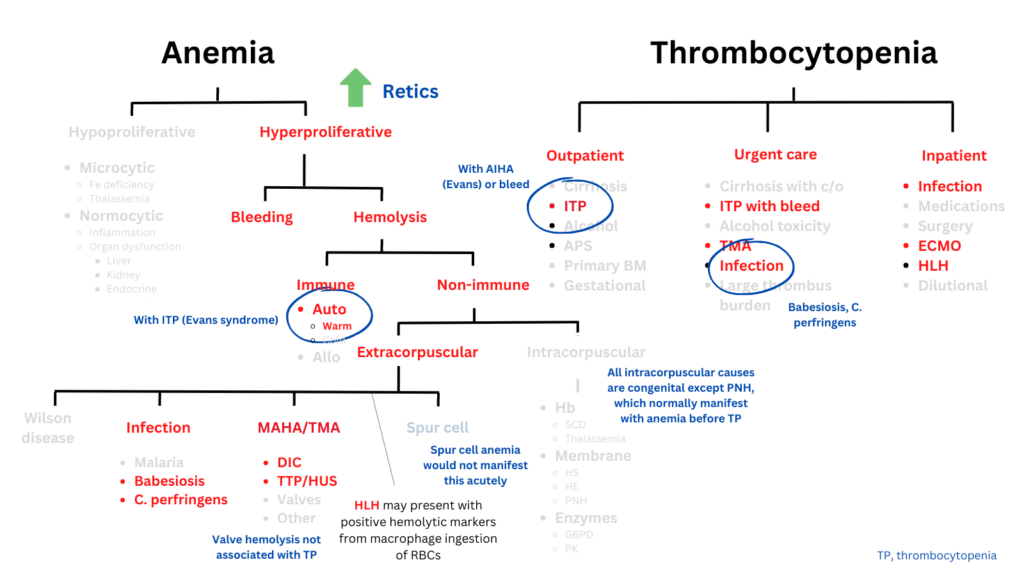
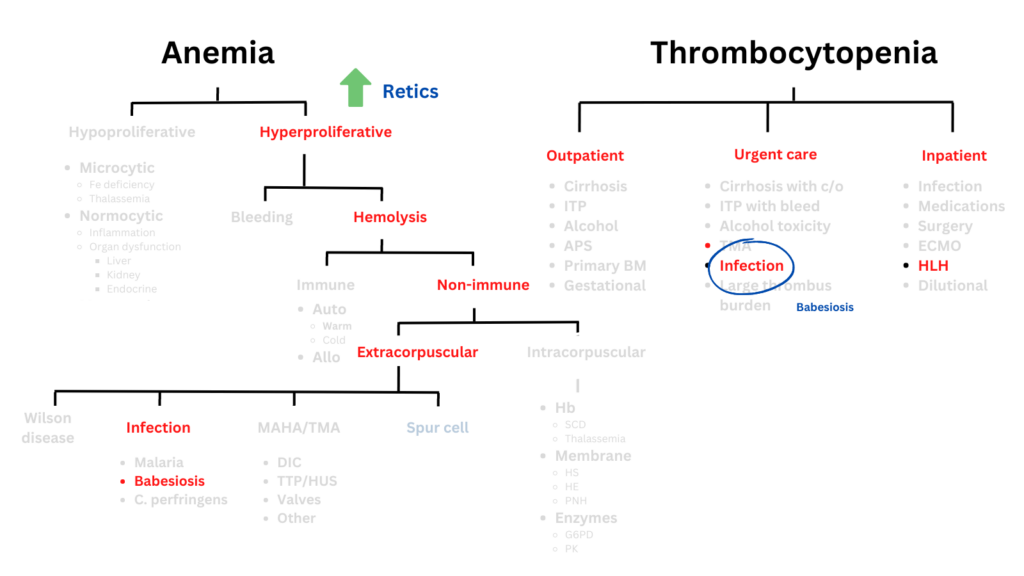
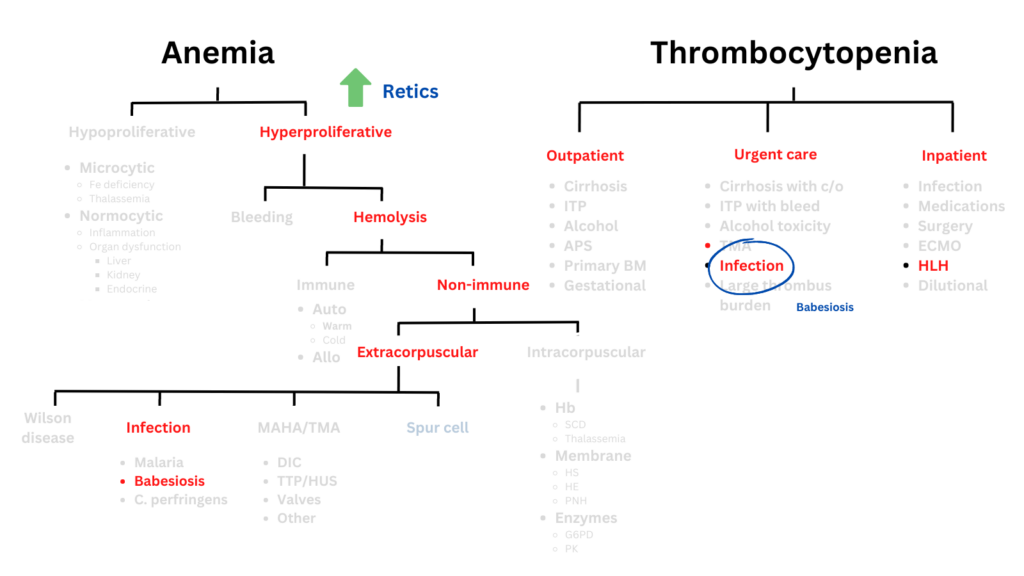
Click for AnswerThis patient presented with anemia and thrombocytopenia. Let’s place the differential diagnosis of these two findings side by side:
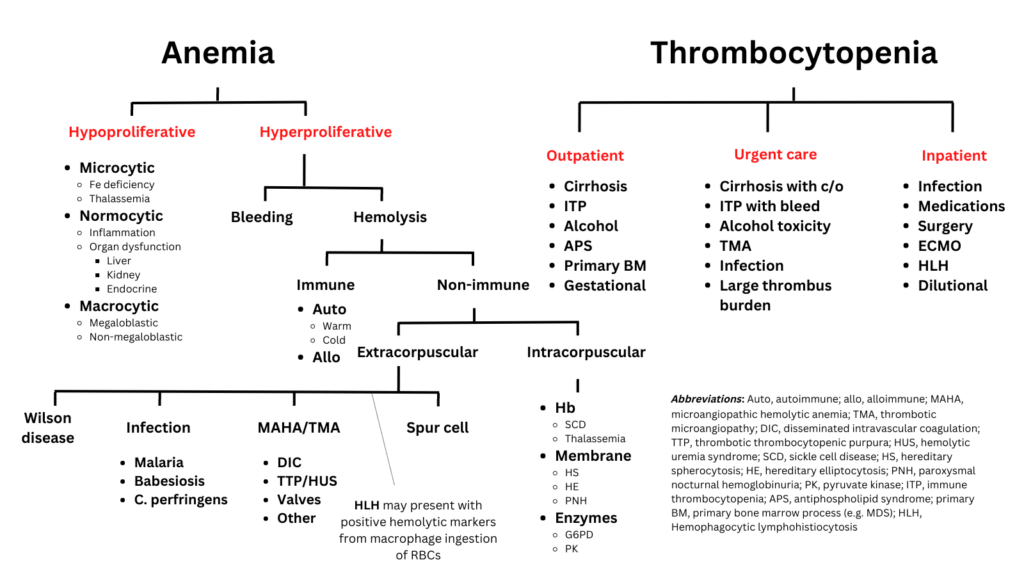
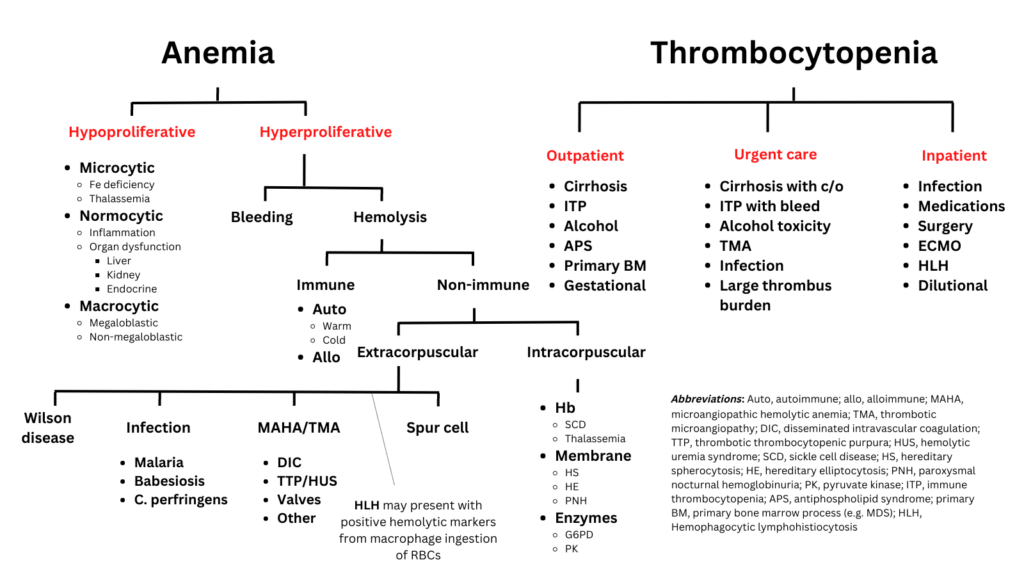
Assuming that there is one overarching diagnosis, which of the following are unlikely explanations:
The following schematic shows conditions that are more likely to be associated with concomitant anemia and thrombocytopenia (in red) vs. those that are less likely (light gray). Selected explanations are in blue.
We can reorganize the algorithms from the previous slides in table form. The conditions that may be associated with both anemia and thrombocytopenia are bolded. The abbreviations are found in a graphic on a previous slide:
| Condition | Hemolytic anemia | Thrombocytopenia (TP) |
|---|---|---|
| Hypoproliferative | – | In B12 deficiency, primary BM process |
| Cold agglutinin disease | + | Not typically associated with TP |
| Alloimmune hemolysis | + | Not typically associated with TP |
| Evans syndrome | + | + |
| Wilson disease | + | Could present with TP, but not typically this acute |
| Babesiosis | + | + |
| C. perfringens | + | + (most of these patients have TP from DIC) |
| DIC | + | + |
| TMA (TTP, HUS) | + | + |
| Valve hemolysis | + | Not typically associated with TP |
| Spur cell anemia | + | The anemia and TP would not typically develop this rapidly |
| Intracorpuscular causes | + | Maybe in PNH, but not with an acute drop in platelets |
| ITP with bleed | Positive hemolytic markers if resorbing internal hematoma | + |
| Alcohol | – | + |
| Primary BM process | – | + |
| TMA | + | + |
| ECMO | + (though hemolytic anemia not common in this setting) | + |
| HLH | Positive hemolytic markers common owing to engulfment and destruction of red blood cells by activated macrophages; retics usually inappropriately low | + |
Now let’s consider the fact that the ALT and AST are elevated. Red blood cells release AST when they are lysed, but very little if any ALT. Thus, although the elevated ratio of AST:ALT is increased, the elevated absolute level of ALT argues for the a hepatic origin. Refer back to the table on the previous slide and identify those conditions that are associated with hepatic injury.
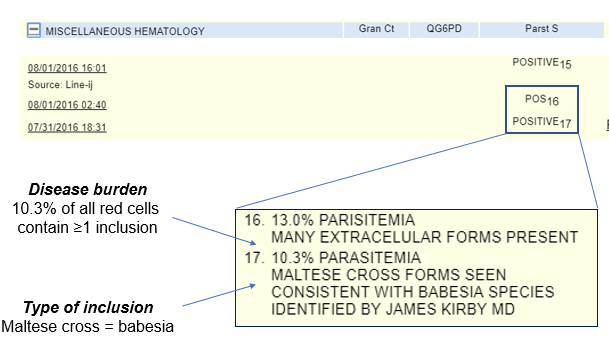
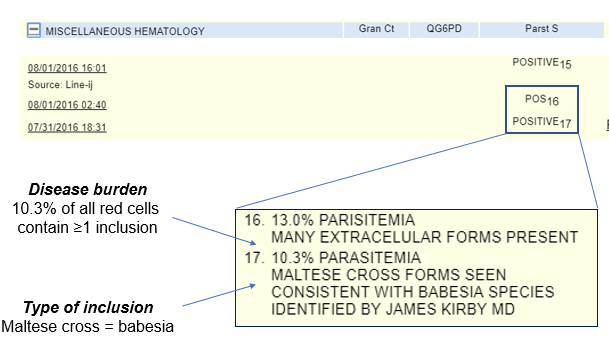
The this smear shows the following:
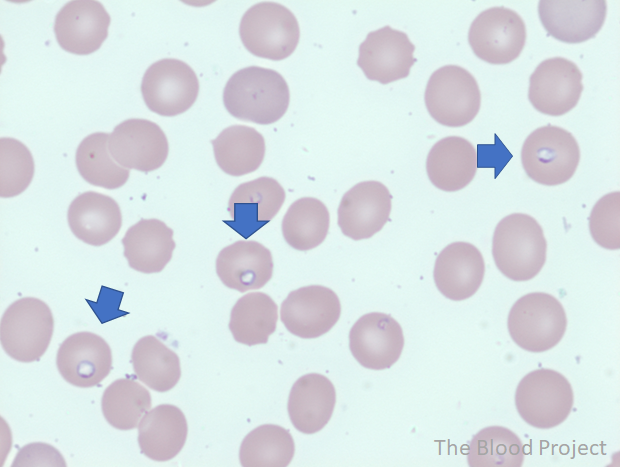
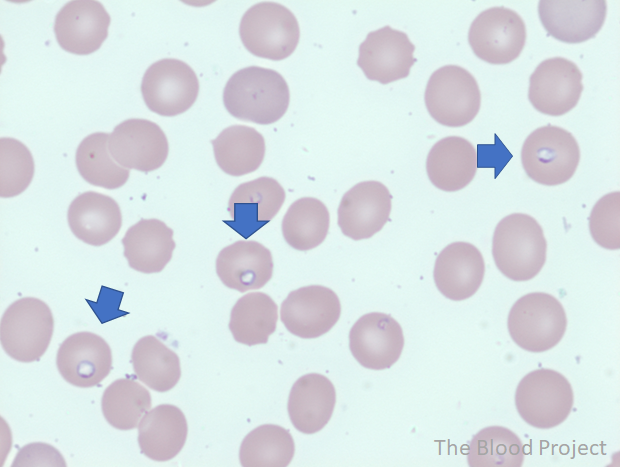
The blue arrows point to red blood cells that have been infected with babesia (ring forms).
Is a thin smear diagnostic for babesiosis or do we need to order serology or PCR testing?
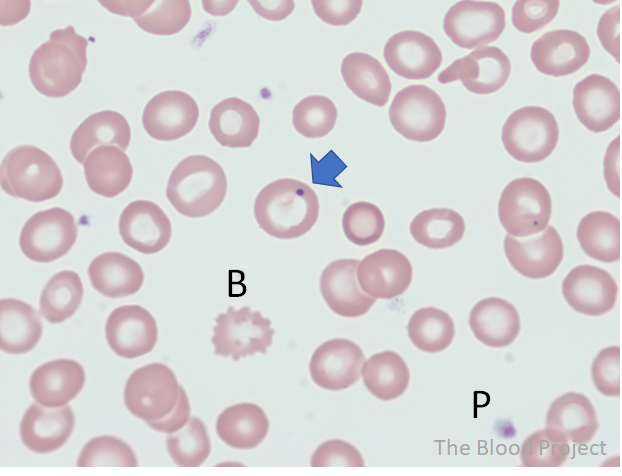
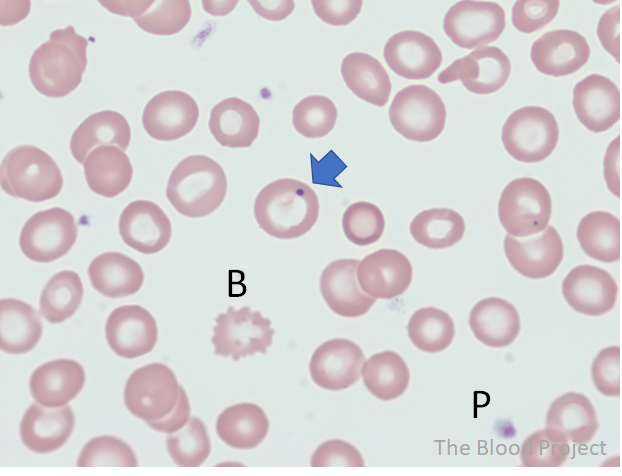
Would the following peripheral blood smear be a reassuring or concerning finding?
Treatment of babesiosis may consist of:
More about the case
56 yo M previously well presented with fevers up to 103 degrees F at home with headaches. He went to urgent care where a CBC revealed a low platelet count. As a result, he was referred to the ED. Further questioning revealed nausea and fatigue. He lived a in wooded area, but had not noticed any tick bites. In the ED, his heart rate was 100, BP 100/60, T 100.9. Labs showed anemia, thrombocytopenia, positive hemolytic markers and transaminitis. A thin smear was ordered and showed the following:
He was admitted to hospital and treated with:
- Quinine and clindamycin
- 6 rounds of exchange transfusion
Testing for anaplasmosis and Lyme was negative.
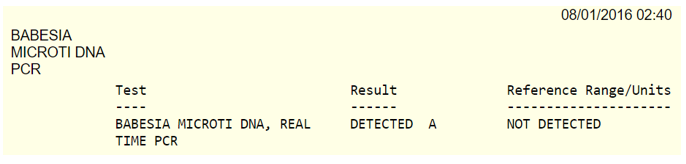
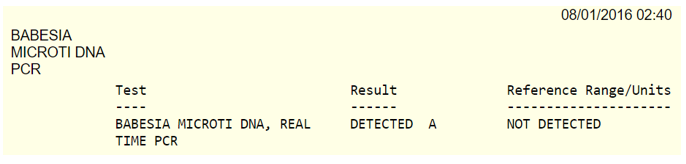
Babesiosis was confirmed with PCR:
His anemia and thrombocytopenia improved over the next several days, as did the degree of parasitemia. He was discharged on day 10 and followed up in ID clinic.
