Postscript
Introduction
- The spleen is a highly vascular organ that participates in hematologic and immune homeostasis.
- The spleen is the larges organ of the lymphatic system.
- The spleen is the primary site of blood filtration in the body.
- An enlarged spleen is a common imaging finding and has many possible causes.
- Splenomegaly most often occurs as a secondary manifestation of a primary disease process.
- The most common cause is portal hypertension, often associated with liver cirrhosis.
- The patient with splenomegaly can present as a diagnostic challenge.
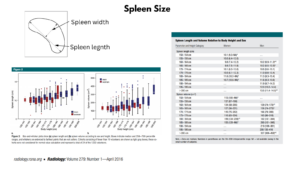
Definition of splenomegaly
- Splenomegaly is the abnormal enlargement of the spleen.
- The normal range for splenic size is only an estimate.
- The size of the spleen correlates with a person’s height, weight, and sex; it is larger in:
- Men compared with women
- Taller and heavier individuals
- Smartphone application (SplenoCalc) is available to determine the upper limit of normal for splenic length based on an individual’s sex and height.
- The ‘‘gold-standard” definition of splenomegaly is splenic weight:
- The normal adult spleen weighs about 50–250 g:
- Men: 80–200 g; women: 70–180 g
- Median weight of 150 g
- Splenic weight decreases with age
- Can only be established at splenectomy or post mortem examination.
- The normal adult spleen weighs about 50–250 g:
- A single radiological definition of normal splenic size has not been adopted:
- On ultrasound examination, ‘‘craniocaudal length”:
- Is used most often to measure splenic size.
- Correlates well with splenic volume.
- Quoted upper limit of normal varies from 11 to 14 cm.
- A maximum length of 13 cm is a typical limit.
- With CT examination, splenic length, the ‘‘splenic index” (product of length, depth and width) and the sum of volumes of consecutive scan slices have all been used (normal range is 160–440 cm³).
- On ultrasound examination, ‘‘craniocaudal length”:
- Massive splenomegaly:
- Variable defined as:
- Lower spleen pole within the pelvis.
- Spleen that crosses the midline.
- Spleen palpable > 8 cm below left costal margin.
- Spleen weight >1000 g.
- Variable defined as:
- Isolated splenomegaly:
- Splenomegaly that remains undiagnosed despite extensive investigation.
- Hypersplenism:
- Splenic sequestration and/or destruction of red blood cells, white blood cells and/or platelets leading to one or more cytopenias.
- Typically results from portal hypertension.
- May rarely occur with a normal-sized spleen (though some include splenomegaly as part of the definition).
Epidemiology
- 2.9% prevalence of a palpable spleen in college freshmen in 1966.1
- 2-5.6% prevalence of palpable spleen in unselected medical outpatients.
- 0.3 estimated incidence of splenomegaly in patients admitted to US hospitals from 1963 to 1995.
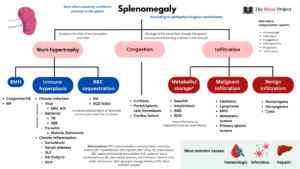
Classification of splenomegaly
- According to pathophysiological mechanisms:
- 3 major mechanisms:
- Increased splenic function (work hypertrophy):
- Results from excessive function of normal splenic activities:
- Hyperplasia associated with extramedullary hematopoiesis:
- Myelofibrosis:
- Primary
- Secondary
- Essential thrombocythemia
- Polycythemia vera
- Marrow infiltration
- Bone marrow toxicity
- Myelofibrosis:
- Hyperplasia of the reticuloendothelial system:
- Increased sequestration of abnormal erythrocytes from the circulation leading to engorgement of splenic cords and venous sinuses and hypertrophy of reticuloendothelial system, as seen in:
- Hereditary spherocytosis
- Sickle cell anemia:
- Early in life before the spleen atrophies
- As a manifestation of acute splenic sequestration
- Thalassemia major
- Ovalocytosis
- Paroxysmal nocturnal hemoglobinemia
- Pernicious anemia
- Increased sequestration of abnormal erythrocytes from the circulation leading to engorgement of splenic cords and venous sinuses and hypertrophy of reticuloendothelial system, as seen in:
- Hyperplasia of the immune system leading to follicular hyperplasia (expansion of white pulp):
- Chronic systemic infections such as:
- Bacterial:
- Brucellosis
- Actinomycosis
- Tickborne diseases
- Infective endocarditis
- Syphilis
- Tb
- Typhoid fever
- Viral illnesses:
- MCV
- EBV
- Hepatitis
- HIV
- Fungal:
- Fungal microabscesses (especially candida)
- Histoplasmosis
- Parasitic:
- Echinococcosis
- visceral leishmaniasis
- malaria
- Bacterial:
- Immune/chronic inflammation-mediated disorders such as:
- Immune thrombocytic purpura
- Autoimmune hemolytic anemia
- Rheumatoid arthritis (Felty syndrome)
- Schistosomiasis
- Toxoplasmosis
- Systemic lupus erythematosus
- Drug reactions
- Sarcoidosis
- Thyrotoxicosis
- Hemophagocytic lymphohistiocytosis (HLH)
- Chronic systemic infections such as:
- Hyperplasia associated with extramedullary hematopoiesis:
- Results from excessive function of normal splenic activities:
- Infiltration (cells and/or extracellular substances):
- Splenic infiltration secondary to neoplasms:
- Malignant conditions:
- Mainly:
- Lymphoma – the most common malignant mass in the spleen
- Leukemia
- Primary myelofibrosis
- Non-hematological malignancies rarely metastasize to the spleen:
- Most common primary lesions to metastasize to the spleen include:
- Breast
- Lung
- Ovarian
- Colorectal
- Gastric
- Melanoma
- Most common primary lesions to metastasize to the spleen include:
- Mainly:
- Benign conditions:
- Hemangiomas – the most common benign neoplasm of the spleen
- Hamartomas
- Littoral cell angiomas
- Lymphangiomas
- Sclerosing angiomatoid nodular transformation (SANT)
- Malignant conditions:
- Splenic infiltration secondary to metabolic disorders:
- Gaucher’s disease (deficiency in glucocerebroside enzyme activity)
- Amyloidosis
- Glycogen storage disease
- Langerhans cell histiocytosis
- Mastocytosis
- Mucopolysaccharidoses
- Niemann-Pick disease
- Splenic infiltration secondary to pseudocysts or true cysts:
- Congenital
- Inflammatory
- Vascular
- Posttraumatic
- Neoplastic
- Splenic infiltration secondary to neoplasms:
- Congestion:
- Results from blockage of the blood flow through the splenic vasculature and pooling of blood in the red pulp, leading to:
- Dilated veins and sinuses
- Fibrosis of the red pulp
- Hemosiderin-laden macrophages
- Causes include:
- Cirrhosis
- Cardiac failure
- Thrombosis or other obstructions in the spleen-related circulation portal or hepatic vein
obstruction
- Results from blockage of the blood flow through the splenic vasculature and pooling of blood in the red pulp, leading to:
- Increased splenic function (work hypertrophy):
- In many cases, the presence of splenomegaly results from a combination of pathophysiologic mechanisms.
- 3 major mechanisms:
- According to underlying conditions:
- Hematologic
- Infectious
- Congestive
- Inflammatory
- Neoplastic
- Infiltrative
- Most common causes of splenomegaly are hematologic (especially hematologic malignancy), hepatic, or infectious in origin.
- Most of the mechanisms reflect passive engorgement with blood due to vascular pressure, increase in size due to hemolysis, or enlargement due to infiltration by cells or other material.
- The distribution of specific causes of splenomegaly differs in different populations.
- Most common causes of massive splenomegaly:
- Hematological disorders:
- Chronic myeloid leukemia
- Agnogenic myeloid metaplasia
- Polycythemia vera
- Essential thrombocythemia
- Indolent lymphomas
- Hairy cell leukemia
- Beta-thalassemia major
- Infectious diseases:
- Kala-azar (visceral leishmaniasis)
- Malaria
- Infiltrative conditions:
- Gaucher disease
- Primary angiosarcoma of the spleen
- Hematological disorders:

International Journal of Biochemistry and Cell Biology 94 (2018) 40–43
Patient cohorts
- Cohort of 129 patients given the ICD-10 splenomegaly diagnosis code in 1994–2013 at Odense University Hospital Denmark, excluding patients with prior splenomegaly, malignant haematological neoplasia or liver cirrhosis:
- Hematological 39%:
- Lymphoma 17%
- MPN 14%
- CLL/HCL 5%
- Hemolytic disease 2%
- Other hematological diseases 3%
- Hepatic 18%:
- Cirrhosis 11%
- Portal vein thrombosis 3%
- Portal hypertension from other causes 3%
- Cancer 1%
- Infections (10%):
- Acute mononucleosis 3%
- CMV 2%
- Endocarditis 1%
- Unidentified infection 5%
- Primary splenic 3%
- Inflammatory 2%
- Other diseases 3%
- Unknown/idiopathic 25%
- Hematological 39%:
- Cohort of 449 patients (mostly inpatients)
- Splenomegaly was defined as an enlarged spleen determined by one of the following:
- Palpable by at least two clinicians or noted on two written observations
- Greater than 12 cm in length on radiologic imaging study
- More than 250 grams wet weight on an excised spleen from a surgical procedure or autopsy
- Causes in 301 patients from University of California, San Francisco (UCSF) included:
- Hepatic 29%
- Hematologic 32%
- Infectious 16%
- Congestive or inflammatory 10%
- Other 5%
- Cause unknown 2%
- Causes in 148 patients from San Francisco General Hospital Medical Center (SFGH):
- Hepatic 41%
- Hematologic 16%
- Infectious 36%
- Congestive or inflammatory 4%
- Other 1%
- Cause unknown 1%
- Splenomegaly was defined as an enlarged spleen determined by one of the following:
- Cohort of 170 patients (inpatients and outpatients)
- All inpatient and outpatient hospital records for patients of any age that were diagnostically coded as having splenomegaly from 1983 through 1993 were reviewed retrospectively for an 11-year period.
- Splenomegaly was defined as a palpable spleen verified by one of the following:
- At least two clinicians, two observations on abdominal examination
- Over 12 cm in length as seen on a radiographic imaging study such as abdominal computerized tomography or abdominal ultrasound
- An excised spleen from surgery or autopsy that weighed over 250 g wet weight.
- Causes included:
- Hepatic 36%
- Hematologic 35%
- Infection 16%
- Inflammatory 5%
- Primary splenic 4%
- Other 3%
Pathophysiology
- Normal anatomy
- The spleen occupies the left upper quadrant of the abdominal cavity, posterior to ribs 9 through 11.
- The spleen is attached to:
- The stomach anteriorly by the gastrosplenic ligament
- The left kidney posteriorly by the splenorenal ligament
- The adult human spleen typically constitutes ∼0.2% of total body weight and is not palpable upon physical examination.
- The splenic artery, derived from the celiac artery, supplies arterial blood to the spleen with little collateral flow.
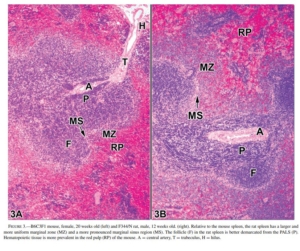
- The internal tissue of the spleen is divided into two distinct macroscopic compartments:
- Red pulp:
- Accounts for three-fourths of the splenic volume.
- Acts as a:
- Blood filter that removes foreign material and damaged and effete erythrocytes.
- Storage site for iron, erythrocytes, and platelets.
- Consists of an open circulation system of macrophage-lined venous sinuses and splenic cords (cord-like projections of fibroblasts and fibrils of connective tissue; also known as Cords of Billroth).
- The cords:
- Are blind-ending structures with very small openings through which red blood cells must traverse to reenter the sinusoids and systemic circulation.
- Act as a bottleneck for erythrocytes, only allowing highly deformable erythrocytes to navigate these passages.
- Abnormal cells are engulfed and destroyed by splenic macrophages.
- White pulp:
- Plays a role in adaptive immunity.
- A major secondary lymphoid compartment that contains approximately one-fourth of the lymphocytes in the body.
- Consists of:
- B-cell follicles
- Marginal zones surrounding follicles
- T-cell lymphoid tissue surrounding the arterioles (periarteriolar lymphoid sheath [PALS])
- White pulp is bordered by the marginal zone, a transit area that allows the migration of blood cells between the circulation and the white pulp.
- Red pulp:
- The ratio of white to red pulp increases with age due to accumulated antigenic exposure and stimulation.
- The spleen is encased in a capsule of composed of dense fibrous tissue, elastic fibers, and smooth muscle.
- There are two circulatory routes through the splenic pulp: open and closed circulation:
- The closed ‘fast flow’ circulation drains blood directly into the venous sinusoids, flowing together to become trabecular veins.
- The open ‘slow flow’ circulation, in which blood flows into a reticular fibrous framework of the red pulp and/or via the marginal zone of the lymphatic tissue before reaching the sinusoids.

The afferent splenic artery turns into central arterioles, which are covered by the white pulp, a region supporting adaptive immune responses and consisting of distinct T and B cell compartments. The blood from the arterioles reaches the red pulp cords and venous sinuses. The red pulp contains macrophages and erythrocytes and plays a major role in surveillance of blood-borne pathogens, elimination of old erythrocytes, and iron recycling. The organ is surrounded by the capsule, a connective layer of fibers entering the splenic parenchyma and forming the trabeculae. Abbreviations: CA, central arteriole; FL, follicle; MZ, marginal zone; MBC, marginal zone bridging channels; PALS, periarteriolar lymphoid sheath. Trends in Immunology, June 2018, Vol. 39, No. 6.
Toxicologic Pathology, 34:455–465, 2006
- Normal functions of the spleen
- Immunity (white pulp):
- Spleen is a secondary lymphoid organ.
- Mature B cells interact with T cells, leading to antibody synthesis.
- Continuous filtration (red pulp):
- Erythrocyte quality control via removal (phagocytosis) of:
- Abnormal or effete (aged) RBCs
- Nuclear remnants (Howell-Jolly bodies)
- Insoluble globin precipitates (Heinz bodies)
- Endocytic vacuoles
- Clearance of bacteria and blood cells coated by antibodies.
- Recycling of iron.
- Erythrocyte quality control via removal (phagocytosis) of:
- Storage:
- 240 ml of red cells can be stored and mobilized via splenic contraction (though role of splenic contraction in humans is debated).
- 30% of platelets.
- Extramedullary hematopoiesis, occurring:
- In early gestation, until 4-5 months gestation, at which time bone marrow becomes hematopoietic site in the fetus.
- As part of normal physiologic response during pregnancy.
- Can be reactivated in certain diseases in adults.
- Immunity (white pulp):
- Pathophysiology of splenomegaly
- Expansion of red pulp
- Expansion of white pulp
- Infiltration with:
- Other types of cells
- Extracellular substances
- Intracellular substances
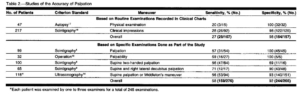
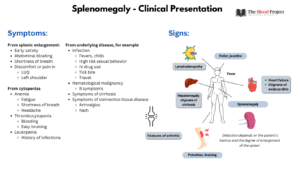
Clinical presentation
- Symptoms:
- Related to enlarged spleen
- Related to underlying causes
- Physical findings
- Enlarged spleen:
- Detected using:
- Percussion
- Loss of tympany as the enlarging spleen impinges on the adjacent air-filled lung, stomach, and colon.
- Three percussion methods:
- Percussion by Nixon’s method:
- Patient is placed in the right lateral decubitus position.
- Percussion is initiated midway along the left costal margin and continued upward along a line perpendicular to the costal margin.
- In a normal examination, dullness extends no further than 8 cm above the costal margin.
- Splenomegaly is diagnosed when the upper limit of dullness extends more than 8 cm above the costal margin.
- Percussion by Castell’s method:
- The patient is placed in the supine position.
- Percussion is carried out in the lowest intercostal space in the left anterior axillary line in both expiration and full inspiration.
- In a normal examination, the percussion note remains resonant throughout this maneuver.
- Splenomegaly is diagnosed when the percussion note is dull or becomes dull on full inspiration.
- Percussion of Traube’s Space.
- Percussion by Nixon’s method:
- Palpation
- Two-handed palpation, with patient in right lateral decubitus:
- Patient in the right lateral decubitus position.
- Examiner’s left hand is slipped from front to back around the left lower thorax, gently lifting the left lowermost rib cage anteriorly and medially.
- The tips of the fingers of the examiner’s right hand are pressed gently just beneath the left costal margin, and the patient is asked to take a long, deep breath as the palpation of a descending spleen is sought.
- If none is felt, the procedure is repeated, lowering the right hand 2 cm toward the umbilicus each cycle, until the examiner is confident that a massive spleen has not been
missed.
- One-handed palpation, with patient supine:
- Method is identical to the former one, except that no counter pressure is applied by the left hand to the rib cage.
- Hooking maneuver of Middleton, with patient supine:
- Patient is asked to lie flat with his or her left fist under the left costovertebral angle.
- The examiner is positioned to the patient’s left, facing the patient’s feet.
- The fingers of both the examiner’s hands are curled under the left costal margin, and
the patient is asked to take a long, deep breath as the palpation of a descending spleen is sought.
- Two-handed palpation, with patient in right lateral decubitus:
- Percussion
- Dullness to percussion in the lowest intercostal space at the left axillary line has an 82% sensitivity for splenomegaly.
- The overall sensitivity of palpation is 58%.2
- Up to 16% of palpable spleens have been found to be of normal size on radiological assessment.
- Detected using:
- Enlarged spleen:
JAMA 1993;270:2218.
-
- Signs associated with underlying causes
Diagnosis
- Physical exam for splenomegaly is discussed in the previous section.
- Confirmation of splenomegaly requires imaging studies:
- Ultrasonography:
- Advantages include:
- Accuracy
- Cost-effectiveness
- Lack of radiation
- Colour Doppler is useful in the evaluation of vascular pathology in the splenic hilum.
- Every focal heterogeneity detected on US should be further evaluated by CT or MR imaging.
- Advantages include:
- Unenhanced CT
- Mainly used for the detection of splenic calcifications.
- Contrast-enhanced computed tomography:
- After intravenous contrast injection, the normal spleen enhances in a mottled pattern during the arterial and early portal venous phases.
- Enhancement pattern is caused by variable flow rates through the open and closed circulation. This
inhomogeneous enhancement pattern should not be confused with splenic disease.
- Contrast-enhanced computed tomography:
- If portal vein thrombosis is suspected.
- Ultrasonography:
- Radiology has four major roles in the investigation of splenomegaly:
- Confirmation of splenic size
- Evaluation of splenic architecture:
- Distinguishes between:
- Focal lesions
- Single
- Multiple
- Diffuse splenomegaly – most commonly finding
- Focal lesions
- Distinguishes between:
- Assessment of other organs affecting the differential diagnosis:
- Imaging findings specific to a single disease are uncommon
- Allows for evaluation of:
- Liver
- Lymph nodes
- Radiologically-guided biopsy
- Lab tests include:
- First-line:
- Hematology
- CBC
- Peripheral smear
- PT, aPTT
- Biochemistry:
- BUN and creatinine
- Liver function tests
- CRP
- LDH
- Vitamin B12
- Microbiology (if indicated)
- Monospot test
- Serology for:
- HIV
- CMV
- Toxoplasmosis
- Brucella
- Immunology (if indicated)
- ANA
- RF
- Hematology
- Second line (depending on findings in first-line testing and clinical context):
- Bone marrow biopsy
- JAK2 V617F mutation
- Peripheral blood flow cytometry
- First-line:
- Splenic biopsy
-
- Fine-needle aspiration (FNA)
- Core biopsy:
- May be used to diagnose a wide range of infectious, benign and malignant conditions.
- Allows one to avoid diagnostic splenectomy.
-
- Diagnostic splenectomy
Treatment
- Therapeutic options for splenomegaly include:
- Treatment of the underlying disease process
- Spleen reduction therapies:
- Irradiation
- Chemotherapy
- Transfusions
- Radiofrequency ablation
- Partial splenic embolization
- Radical splenectomy:
- Techniques include:
- Open
- Laparoscopic
- Indications include:
- A painfully enlarged spleen
- Splenic rupture
- Splenic artery aneurysm
- Isolated splenic vascular or parenchymal lesions
- Hypersplenism
- Complications include:
- Infection
- Thromboembolism
- Techniques include:
